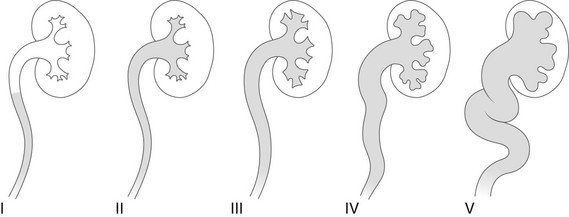
Chapter 120 Overview: Vesicoureteral reflux (VUR) refers to the retrograde passage of urine from the urinary bladder into the ureter and often to the calyces. It is a common and potentially important childhood problem that generally is regarded as abnormal at all ages. Because of recent insights into the natural history of fetal and neonatal urinary tract development, this judgment is increasingly under discussion and review. VUR itself causes neither urinary tract infection (UTI) nor renal damage, but it may be associated with bladder dysfunction. However, VUR is a risk factor for the development of upper UTI and pyelonephritis, with consequent renal scarring and potential long-term sequelae (Box 120-1).1–15 The major objective in the evaluation of children with documented UTI traditionally has been to diagnose or exclude VUR. Today, the focus of imaging in UTI has shifted to evaluation of renal inflammatory involvement or existing renal scarring and to assessment of structural or functional abnormalities of the urinary tract that may predispose to renal damage (i.e., prenatal “hydronephrosis”), complicated UTI, and VUR, particularly early depiction of anomalies that may require prompt interventional or surgical treatment to prevent renal damage.1,16–34 Overview: The most common cause of VUR is a developmental anomaly of the ureterovesicular junction (UVJ) in which the ureteral orifice may be lateralized or too large (“golf hole ostium”) or the submucosal ureter is too short and/or deficient in longitudinal muscle fibers. VUR often is seen in patients with other urinary tract anomalies (Box 120-2). Additionally, some sort of immaturity of the UVJ may play a role in fetal and neonatal VUR, because a large percentage of congenital VUR decreases spontaneously within the first years of life. This type of VUR, often referred to as primary or congenital VUR, is seen more frequently in girls than in boys. High-grade congenital VUR in male infants, often with severe congenital renal dysplasia (“congenital reflux nephropathy”), constitutes a different entity with a far more serious prognosis. Secondary VUR is seen in patients with bladder outlet obstruction (e.g., posterior urethral valves) or with neurogenic bladder disease (e.g., myelomeningocele). It is caused in part by thinning and weakening of the UVJ musculature precipitated by chronically increased intravesical pressure. However, the fact that VUR in these disorders may be absent and frequently is unilateral suggests the possibility of an associated congenital weakness of the UVJ or a protective measure of a potentially thickened bladder wall that otherwise may lead to ureteral obstruction. Although lesser degrees of lower urinary tract obstruction per se do not seem to cause VUR in patients with a completely normal UVJ, they may precipitate VUR (with ascending spread of infection to the kidneys) in people with ostia of borderline competence as the result of local edema and cellular infiltration, causing further weakening of the UVJ.1,35–38 Overview: The diagnostic imaging modalities available for the evaluation of VUR include ultrasound, voiding cystourethrogram (VCUG), and nuclear cystography (Box 120-3). A new method for VUR assessment is contrast-enhanced voiding urosonography (ce-VUS). This method uses ultrasound contrast material (e.g., shaken saline solution, air, or commercially available contrast agents) instilled into the urinary bladder via suprapubic or transurethral catheterization and bladder filling (Fig. 120-1 and e-Fig. 120-2). The reflux of contrast into the upper tracts can be appreciated readily by alternately scanning both kidneys as well as the retrovesical space during filling and before and after voiding. Ultrasound techniques such as harmonic imaging, stimulated acoustic emission, or other contrast-specific techniques have further enhanced ce-VUS potential for VUR depiction and grading, resulting in a reported sensitivity and specificity equal to VCUG (Fig. 120-3 and e-Fig. 120-4).1,39–55 Figure 120-1 Vesicoureteral reflux demonstrated by echo-enhanced urosonography. Figure 120-3 Improved detection of vesicoureteral reflux using contrast-specific techniques. e-Figure 120-2 Vesicoureteral reflux demonstrated by echo-enhanced urosonography, in the same patient as in Figure 120-1. e-Figure 120-4 Improved detection of vesicoureteral reflux using contrast-specific techniques in the same patient as in Figure 120-3. A generic image shown with simultaneous contrast and harmonic imaging gray-scale information. VCUG is and remains the basic imaging technique for VUR assessment. It uses radiopaque contrast material instilled into the catheterized and emptied urinary bladder for detection of VUR into the upper urinary tract. For a reliable assessment, the bladder must be filled to near capacity. For infants younger than 1 year of age, bladder capacity in milliliters is determined by the patient’s weight in kilograms × 7. For patients older than 1 year of age, bladder capacity in milliliters equals age in years plus 2, multiplied by 30. Fluoroscopic observation of the (early) filling phase, the distal ureters (in oblique projections), the renal collecting system, and the urethra during voiding (lateral projection in boys) enables focused imaging of critical areas and conditions such as intrarenal VUR and UVJ anatomy. Cyclic VCUG should be performed in infants to avoid missing significant VUR, because VUR may not occur during the first fill and void.1,56–69 For studying the renal parenchyma, ultrasound and dimercaptosuccinic acid (DMSA) scintigraphy commonly are used. Other methods for the evaluation of the upper tract are contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI), which may become indicated for assessment of complicated disease. The choice of imaging method for VUR assessment depends in large part on individual preference, availability, and the experience of the examiner. Other variables include the age, sex, and race of the patient; whether an initial or a follow-up examination is being done; and the cost of and time required to perform the procedure. All male infants and all patients before surgery should have a conventional VCUG performed for detailed anatomic assessment.1,20,21,23,24,28,30,31,70–85 Overview: The international criteria for grading VUR is based on the VCUG (Fig. 120-5). Similar comparable grading scales exist for ce-VUS and nuclear cystography. Although simple and easy to use, this classification and other similar classifications reflect only the appearance of the upper tracts and do not take into consideration other important factors such as the age and sex of the patient, the presence of intrarenal reflux or urinary tract obstruction, renal function and scarring, high- or low-pressure VUR, early or late VUR, slow or quick clearance from the upper collecting system, cystoscopic findings, and the presence or absence of associated disorders (e.g., ureteral duplication, ureteral ectopia, ureterocele, bladder diverticula, prunebelly syndrome, urethral obstruction, megacystis-megaureter association, or neurogenic bladder). This additional information sometimes is essential for making decisions about therapy.1,86–88 On ultrasound, the ureters and pelvocalyceal systems of patients with VUR often appear normal even if they appear dilated on VCUG (particularly when the bladder is empty or catheterized). Indirect sonographic signs for VUR are uroepithelial thickening of the ureter or renal pelvis, changing diameter of the pelvocalyceal system and ureter, quick refilling of the bladder after voiding, asymmetric ureteral inflow jets, and a lateralized position or unusual shape of the ureteral ostium (Fig. 120-6). In more severe cases, the refluxing upper tracts are grossly dilated, with clubbing of the calyces and elongated and tortuous ureters (e-Fig. 120-7). Ureteral peristalsis generally is poor, especially in the presence of urinary infection and high-grade VUR. Kinks in the proximal ureter or distal segment of the ureter are common. Direct sonographic evidence of VUR may be identified on ce-VUS as described previously.1,89–103 Figure 120-6 Lateralized ureteral orifice. e-Figure 120-7 Reflux nephropathy. The appearance of refluxing ureters and pelvocalyceal systems on VCUG is quite variable, ranging from normal-sized upper tracts to extreme upper tract dilatation and marked ureteral tortuosity (Fig. 120-8 and e-Fig. 120-9). These changes may reflect only an increased volume and decreased motility of the ureters, but in some cases a developmental defect of the ureter related either to inutero VUR or to an inadequate development of the ureteral musculature is suspected (e.g., prune-belly syndrome). In some patients, VUR is accompanied by marked ballooning of the pelvocalyceal system without evidence of UPJ obstruction (e-Fig. 120-10). The phenomenon may be transient and reflects an increased elasticity of unknown cause in the upper collecting system. Sometimes VUR may induce a kink at the UPJ, with a valvelike mechanism that may even deteriorate after antireflux procedures, producing a functional UPJ obstruction (Fig. 120-11). The obstruction may be related to local scarring from infection, anatomic kinks in the ureter, or overlying aberrant vessels or fibrous bands. Thus a primary congenital UPJ obstruction and primary VUR may coexist as associated anomalies.1,104–107 Figure 120-8 Vesicoureteral reflux. Figure 120-11 Vesicoureteral reflux and functional ureteropelvic junction obstruction. e-Figure 120-9 Vesicoureteral reflux. e-Figure 120-10 Vesicoureteral reflux. In patients with VUR to the calyces, one may observe transient pyelotubular and interstitial reflux of contrast material extending outward in a wedge-shaped pattern from one or more papillae to the renal cortical surface (Fig. 120-12). Intrarenal reflux is an important finding because of its association with renal scarring. It is believed that the morphology of the opening of the collecting ducts of Bellini on the renal papilla is partly responsible for intrarenal reflux. The opening of these ducts on compound, flat-topped papillae (more common at the poles) are round and therefore less resistant to retrograde flow than the slitlike openings of the ducts of simple or conical papillae. The fact that intrarenal reflux does not occur in all infants and that it is rarely seen after age 4 years suggests an additional local defect that improves with age.1–3,6,8,9,12,15,19,56–59,62,63,66,69,88,105,107 Overview: VUR has a tendency to improve and to disappear spontaneously during the first decade of life, often during the preschool years. This tendency is attributed to a maturation process of the UVJ with age, with an increase in the length of the intramural ureter and strengthening of its musculature. Mild VUR (grades I and II) with normal-sized ureters and ureteral orifices has a favorable prognosis and disappears with time in more than 80% of cases, whereas more severe forms of VUR with dilated ureters have a lower incidence of spontaneous recovery (grade III, about 50%; grade IV, 30%; grade V, rarely). VUR that is associated with anatomic anomalies such as a large ureteral orifice and a short submucosal tunnel at cystoscopy is not likely to resolve. VUR occurring in an ectopically ending ureter (i.e., defective UVJ accompanying lateral ureteral ectopia of the lower pole moiety of a duplex kidney) or associated with a large paraureteral diverticulum also tends to persist, especially if the ureter ends in the diverticulum. VUR that occurs in patients with a lower urinary tract obstruction may disappear after correction of the lesion but is considered uncured if it is still present 1 year postoperatively. VUR that occurs in persons with neurogenic bladder disease or bladder dysfunction also tends to persist until the functional disturbance is treated successfully.1,108–117 Overview and Pathophysiology: Renal scarring is a common and potentially serious problem in patients with VUR and upper UTI (acute pyelonephritis). Renal scarring is characterized by one or more areas of renal cortical atrophy that is almost always associated with blunting or distortion of the underlying calyx or group of calyces, retraction of the papillae, and reduction of the medullary zone. Histologically, the affected kidneys show areas of cortical loss with tubular destruction and atrophy and interstitial fibrosis. Obliteration of glomeruli, arteriolar changes, and minor signs of interstitial inflammation also may be observed. The scarring characteristically has a focal or segmental pattern with a predisposition for the upper pole (38%) and less frequently for the lower pole. In some cases the process affects the entire kidney diffusely. The areas of scarring result in one or more clefts or depressions of various sizes in the outline of the kidney. The unaffected renal parenchyma may be hypertrophied, sometimes simulating a renal mass (pseudotumor). When the process is diffuse and severe, it results in global renal atrophy.
Vesicoureteral Reflux
Definition and Imaging Objectives
Etiology
Imaging Techniques
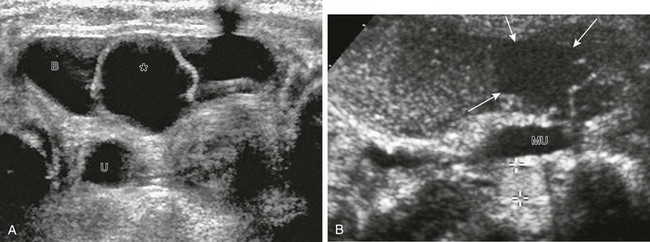
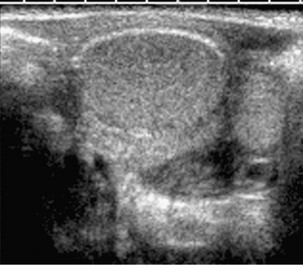
A, A transverse unenhanced bladder sonogram reveals a ureterocele (asterisk) within and a dilated ureter (U) behind the urinary bladder (B). B, A longitudinal sonogram after instillation of contrast material (Levovist) into the urinary bladder shows the nonrefluxing ureterocele (arrows) and corresponding megaureter (MU) and echogenic contrast material within the refluxing lower pole ureter (cursors). See also e-Figure 120-2.
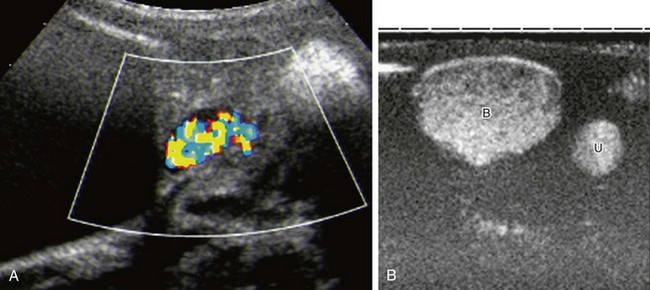
A, The same patient as in Figure 120-1 and e-Figure 120-2, with reflux into the right lower moiety. Reflux is now depicted using stimulated acoustic emission with high ultrasound power (high mechanical index) to burst the contrast bubbles, thus creating strong color signals. B, Contrast-specific imaging techniques (CDI, Siemens, Mountain View, CA) provide exquisite contrast delineation in a patient with refluxing megaureter, using double-image technique for visualization contrast image (B, bladder; U, ureter). See e-Figure 120-4 for a generic image with simultaneous contrast and harmonic imaging gray-scale information.
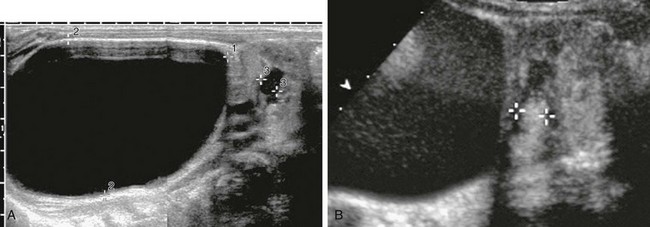
A, A longitudinal sonogram of the duplex right kidney shows a markedly dilated upper moiety and only mild dilatation of the lower pole moiety. B, A longitudinal renal sonogram shows echogenic contrast in the dilated pelvocalyceal system of the lower pole moiety (cursors), thus diagnosing high-grade vesicoureteral reflux.
Grading
VUR Imaging
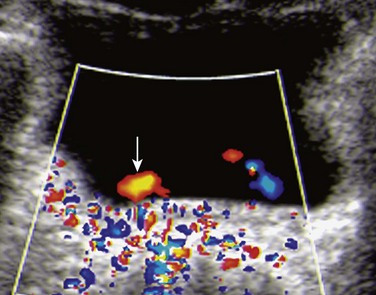
A transverse color Doppler image shows a laterally positioned and abnormally oriented right ureteral jet (arrow). Such indirect signs may help ultrasound diagnosis of vesicoureteral reflux.
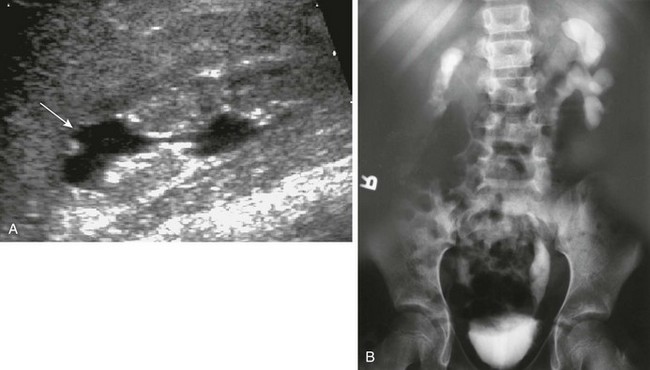
A, A longitudinal sonogram shows features of a scarred kidney from severe vesicoureteral reflux with recurrent urinary tract infection: dilated and clubbed calyces with focal overlying parenchymal narrowing (arrow) and echogenic nondifferentiated parenchyma with irregular contours. B, An intravenous urogram image shows a small and atrophic functioning right kidney with markedly thinned parenchyma. The left kidney collecting system is distorted as well.
Voiding Cystourethrogram

A voiding cystourethrogram image shows bilateral grade IV vesicoureteral reflux. Also see e-Figure 120-9.

A voiding cystourethrogram image after voiding shows bilateral vesicoureteral reflux and ballooning of the left renal pelvis. The intravenous urogram image (not shown) was entirely normal. Bilateral paraureteral (Hutch) diverticula also are present.

A voiding cystourethrogram image shows left grade II vesicoureteral reflux with thin and delicate calyces and right grade III reflux where the calyces are dilated and blunted.
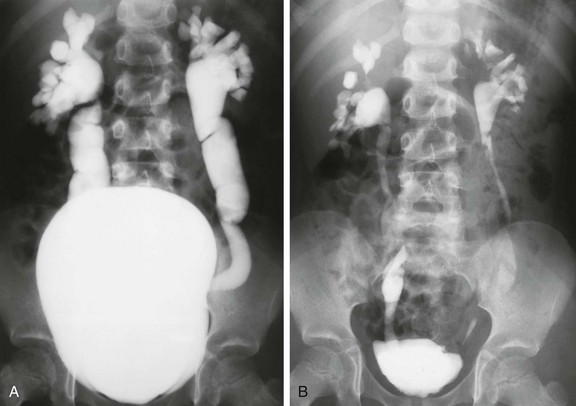
A, A voiding cystourethrogram in a 5-year-old girl with recurrent urinary tract infections shows a large, smooth-walled bladder and bilateral grade V vesicoureteral reflux. B, An image after voiding shows only mild hydroureteronephrosis, along with bilateral renal parenchymal loss.
Natural History
Renal Scarring and VUR
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree