Fig. 17.1
(a, b) The Couinaud segments of the liver. (a) Anterior surface view; (b) visceral surface view. I, caudate/Spigel’s lobe; II, left, posterolateral segment; III, left anterolateral segment; IVa, left superomedial segment; IVb, left inferomedial segment; V, right anteroinferior segment; VI, right posteroinferior segment; VII, right posterosuperior segment; VIII, right anterosuperior segment
Within the lobes and segments are multiple, smaller anatomical units called liver lobules. These lobules are formed of plates of hepatocytes, which are the functional cells of the liver. In addition, the parenchyma of the liver is composed of another type of cells: the reticuloendothelial cells or Kupffer’s cells. Almost 90 % of the reticuloendothelial cells in the body are found in the liver. The sinusoids are capillaries located between the plates of hepatocytes; they receive a mixture of venous and arterial blood from branches of the portal vein and the hepatic artery, respectively. Blood from the sinusoids drains to central veins that continue to empty into the hepatic vein, which enters the inferior vena cava. Kupffer’s cells line the sinusoids and destroy microorganisms.
The liver has digestive, metabolic, hematological, and immunological functions. The hepatocytes synthesize approximately 1 l of bile per day and secrete it into the bile canaliculi, which are small channels between the hepatocytes. The bile canaliculi empty into bile ducts that unite and finally form the right and left hepatic ducts, which join to form the common hepatic duct. Past the point where the cystic duct begins, the hepatic duct is called the common bile duct, which drains into the duodenum through the major duodenal papilla. Bile is necessary for fat digestion and absorption. Unconjugated bilirubin is converted to water-soluble, conjugated bilirubin by hepatocytes and is secreted with bile. The gallbladder stores bile and ejects it when chyme enters the duodenum and stimulates the secretion of cholecystokinin. The hepatocytes are capable of regeneration. Most regeneration takes place in the left lobe in disease states such as alcoholic damage or chronic hepatitis.
17.3 Hepatobiliary Radiopharmaceuticals
Technetium-99m (Tc-99m)-sulfur colloid (SC) is a radiopharmaceutical for liver/spleen imaging. This compound is cleared by cells of the reticuloendothelial system: approximately 85 % by Kupffer’s cells in the liver, 10 % by the spleen, and 5 % by the bone marrow. Tc-99m-phytate is also used for liver/spleen imaging in some countries. However, due to smaller particle size, its splenic uptake is significantly less than that of SC.
Tc-99m-disofenin (2,6-diisopropyl iminodiacetic acid (DISIDA)) and Tc-99m-mebrofenin (2,4,6-trim-ethyl, 5-bromoiminodiacetic acid (BrIDA)) are exclusively used for cholescintigraphy by most laboratories in the United States. Various other iminodiacetic acid (IDA) compounds are available in other countries. These compounds, after being injected intravenously, are bound to plasma albumin, transported to the liver, and actively taken up by the hepatocytes via carrier-mediated, non-sodium-dependent, organic anionic pathways similar to those responsible for bilirubin uptake [1]. The IDA compounds are not conjugated. They are excreted into the bile canaliculi by both active and passive transport mechanisms [2]. Compared with Tc99m-disofenin, mebrofenin demonstrates higher hepatic excretion and lower urinary excretion, especially in patients with a high bilirubin level. Depending on the agents used, 2–15 % of the injected dose is excreted in urine. The more severe the hepatic dysfunction, the greater the renal excretion [3, 4].
Tc-99m-aglactosyl-neoglycoalbumin (Tc-99m-NGA) and Tc-99m-galactosyl human serum albumin (Tc-99m-GSA) are liver imaging agents that bind to the hepatocyte-specific asialoglycoprotein membrane receptors (ASGCP receptor) [5, 6]. These agents have been used primarily to evaluate the functional liver mass/reserve in various clinical settings.
17.4 Evaluation of Liver Diseases
17.4.1 Functional Hepatic Mass/Reserve
It is important to assess the functional hepatic reserve prior to major hepatic resection because postoperative liver failure can significantly affect the clinical course. Several parameters such as the indocyanine green retention/clearance rate, prothrombin time, hepaplastin test, and serum albumin level are useful for the assessment of total hepatic function. The Child-Turcotte-Pugh (CTP) score is a grading system that has been used to classify liver dysfunction and determine the prognosis of chronic liver disease [7, 8]. However, the regional distribution of hepatic function cannot be evaluated by any of the methods mentioned above.
Prediction of the regional hepatic reserve was attempted by morphologically measuring the remnant liver volume by CT scan [9, 10]. However, the liver morphology assessed with CT scan may not reflect the functional status [11, 12].
Functional hepatic reserve has been assessed scintigraphically using various radiopharmaceuticals, including Tc-99m-colloids, Tc-99m-DTPA-human serum albumin (blood pool imaging agent), and a hepatobiliary agent such as Tc-99m-IDA and Tc-99m-N-pyridoxyl-5-methyltryptophan (PMT). Bennink et al. found a strong positive association between hepatic function reserve determined with hepatobiliary scintigraphy (HBS) and indocyanine clearance, little or no association between CT volumetric analysis and indocyanine clearance, and a strong positive association between the remnant liver function determined preoperatively on hepatobiliary scintigraphy and the actually measured value postoperatively. These authors also reported that liver function determination using HBS was highly reproducible [12]. Erdogan et al. reported similar results [13].
Tc-99m-GSA scintigraphy has been used for assessing functional hepatic reserve in a variety of clinical settings [14–20]. This tracer is taken up only by functional hepatocytes, independent of hepatic blood flow [21, 22]. A strong correlation was found between parameters based on Tc-99m-GSA studies and previously known parameters of hepatic function [11, 23]. Tc-99m GSA does not compete with bilirubin, which is an additional advantage in the evaluation of hepatic reserve in patients with hyperbilirubinemia [24]. Overall, Tc-99m-GSA imaging performed prior to surgery and/or other procedures such as a TIPS (transjugular intrahepatic portosystemic shunt) and percutaneous transhepatic portal embolization appears to be a reliable method of predicting functional hepatic reserve after the procedure. While this tracer has not been approved for routine clinical use in the United States, this technique has become a routine test in Japan [25].
17.4.2 Primary Hepatic Neoplasms and Tumor-Like Conditions
17.4.2.1 Hepatocellular Carcinoma
While hepatocellular carcinoma (HCC) usually displays marked arterial vascularity on dynamic perfusion imaging, its appearance on static colloid imaging (focally decreased activity) is nonspecific. Sulfur colloid imaging can be used to differentiate regenerating nodules from HCC in a cirrhotic liver. The presence of colloid uptake typically represents regenerating nodules, while decreased uptake is nonspecific but may include HCC [26].
Approximately 40–50 % of HCCs concentrate hepatobiliary tracers (Fig. 17.2), i.e., Tc-99m-IDA or Tc-99m-PMT. The degree of uptake seems to correlate with tumor differentiation, as well as with survival [27, 28]. Tc-99m-IDA uptake was seen in 70 % of well-differentiated tumors, in 30 % of moderately differentiated tumors, and in no poorly differentiated tumors [27]. In another series of 162 patients, the median survival of 82 patients with increased tumor uptake on delayed Tc-99m-PMT imaging was 1,013 days, compared with 398.5 days in 80 patients with no tumor uptake [28].
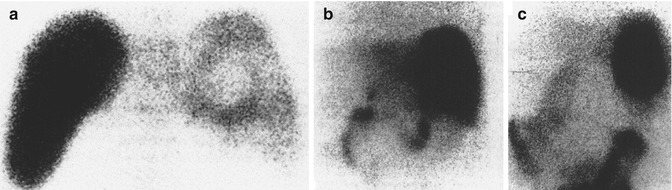
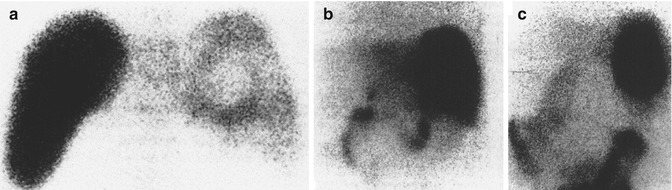
Fig. 17.2
(a) Hepatic scintigraphy with Tc-99m-SC in a patient with hepatoma complicating liver cirrhosis. A defect is observed in the posterior view. (b) Hepatic scintigraphy with Tc-99m-DISIDA 15 min after tracer administration (posterior view). Marked tracer uptake fills the cold area previously observed, as well as the rest of the liver parenchyma. (c) Hepatic scintigraphy with Tc-99m-DISIDA 3 h after tracer administration (posterior view). Tracer is clearly retained in the HCC area while it has been excreted from the nontumoral liver (reprinted from Calvet et al. [27] with permission)
Uptake of hepatobiliary tracers on delayed imaging can be present in other liver lesions that contain hepatocytes, such as focal nodular hyperplasia (FNH) [29]. Kotzerke et al. claimed that the distinction between FNH and HCC is possible with 3-phase imaging (perfusion, 5–10 min, and 2–3 h) [30]. In their series, most FNH exhibited normal or increased uptake at 5–10 min, whereas most HCC displayed decreased or no uptake during this phase.
Gallium-67 and thallium-201 were used in the past for evaluation of HCC in various clinical settings. However, the utility of these tracers in HCC appears to have been replaced largely by positron-emitting tracers recently. These tracers will not be discussed in this chapter.
17.4.2.2 Hepatic Cavernous Hemangioma
Hemangioma is the most common benign tumor of the liver. Most hemangiomas are of the cavernous type, constituted by dilated nonanastomotic vascular spaces lined by flat endothelial cells and supported by fibrous tissue. Thrombi in different stages of organization are often encountered. Long-standing lesions can show extensive hyalinization or calcification [31].
The classic finding of hepatic cavernous hemangiomas (HH) on Tc-99m-RBC imaging was described as a perfusion/blood pool mismatch, i.e., a lack of increased activity on early flow images and a gradual increase in activity on blood pool images over time [32]. This initially seemed to be an important finding especially when one study from the 1980s [33] reported four cases of HCC which showed increased activity on delayed images and claimed that distinction between HH and HCC can be made on early dynamic imaging because HCCs show increased flow as well as increased activity on delayed images, whereas HHs do not show increased activity on flow images. However, other studies, including a large series from Japan, found no cases in which HCC demonstrated increased activity on either planar or SPECT-delayed images [34, 35]. In addition, perfusion in small and/or deeply situated lesions is difficult due to the limited resolution of dynamic imaging. Moreover, it quickly became obvious that the sensitivity of planar Tc-99m-RBC imaging is unacceptably low, ranging from 30 to 53 % [35–41]. The sensitivity of SPECT RBC imaging is higher but still heavily dependent on the lesion size. Reports published in the 1990s showed overall sensitivity of 70–80 % using single-head SPECT [38–40, 42]. Using triple-head cameras [36, 41], the sensitivity was 17–20 % for the detection of lesions smaller than 1 cm, 65–80 % for lesions between 1 and 2 cm, and virtually 100 % for lesions equal to or larger than 1.4 cm (Fig. 17.3). It is remarkable that the specificity and positive-predictive value of both planar and SPECT RBC imaging is essentially 100 % [35–41]. For all of these reasons, neither flow nor delayed planar imaging needs to be a routine part of the Tc-99m RBC study for evaluation of HH.
Fig. 17.3
Tc-99m-RBC SPECT images of the liver (triple-head) reveal multiple hemangiomas. The smallest one (arrow) was 0.7 cm
False-negative results were reported in cases of HH with extensive thrombosis and/or fibrosis [32, 33]. Several false-positive cases related to various malignancies, including HCC as mentioned above, angiosarcomas, metastases, and hepatic lymphoma, have been reported in the literature [33, 43–45]. However, the occurrence of such false-positive results seems extremely rare in view of the 100 % specificity in virtually all studies other than case reports.
When dedicated SPECT imaging is performed, a lesion situated adjacent to large intrahepatic vessels, inferior vena cava, or right kidney needs to be cautiously evaluated to avoid either false-negative or false-positive results [46]. A SPECT/CT hybrid system is becoming more widely available, and fusion imaging will clearly lower the false results [47, 48]. If a SPECT/CT hybrid system is not available, review of all three orthogonal SPECT slices can be helpful when the lesion is adjacent to these structures [46]. Alternatively, a software fusion of SPECT images and CT or MR images may be performed, but this technique is not practical and therefore has never gained popularity. If a multi-head SPECT system is available, obtaining several sequential dynamic SPECT scans at short intervals following injection of Tc-99m-RBC can help distinguish HH from vascular structures as well as from other vascular tumors, since HHs exhibit a gradual increase in blood pool activity over time, while blood vessels and other tumors do not (Fig. 17.4) [46, 49]. It is also essential that labeled RBC scans be correlated with anatomical images obtained separately.
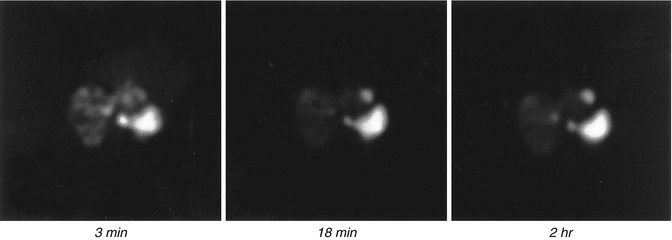
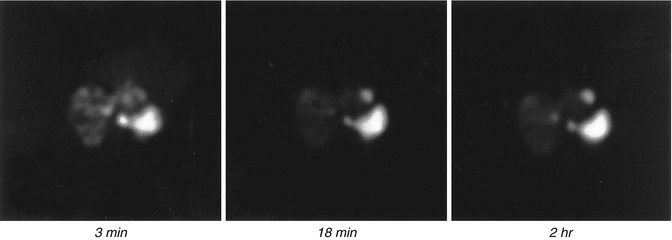
Fig. 17.4
Selected transverse views (3 and 18 min) from a dynamic Tc-99m-RBC SPECT of the liver and an image from a delayed SPECT (right) show a lesion in the tip of the left lobe of the liver that becomes progressively more intense. The findings are consistent with a hemangioma (courtesy of Alan Siegel, MD, Dartmouth Hitchcock Medical Center, Lebanon, NH, USA)
Tc-99m RBC SPECT imaging was reported to be more useful than MRI for evaluation of HH in 1990 because of the lower cost and higher specificity [42]. Despite its near-perfect specificity and positive-predictive value, Tc-99m RBC imaging does not appear to be fully utilized, which may be in part due to improved specificity of other anatomical imaging modalities [50, 51]. Given that, a new prospective head-to-head comparison of SPECT/CT with MRI or ultrasound for evaluation of HH may be needed.
17.4.2.3 Focal Nodular Hyperplasia
Focal nodular hyperplasia contains variable quantities of normal hepatic cellular elements, including Kupffer’s cells, hepatocytes, and bile ducts arranged in a characteristic pattern. The characteristic triad suggesting FNH has been described as arterial blood flow (Fig. 17.5), normal colloid uptake, and accumulation of Tc-99m-IDA tracer [52].
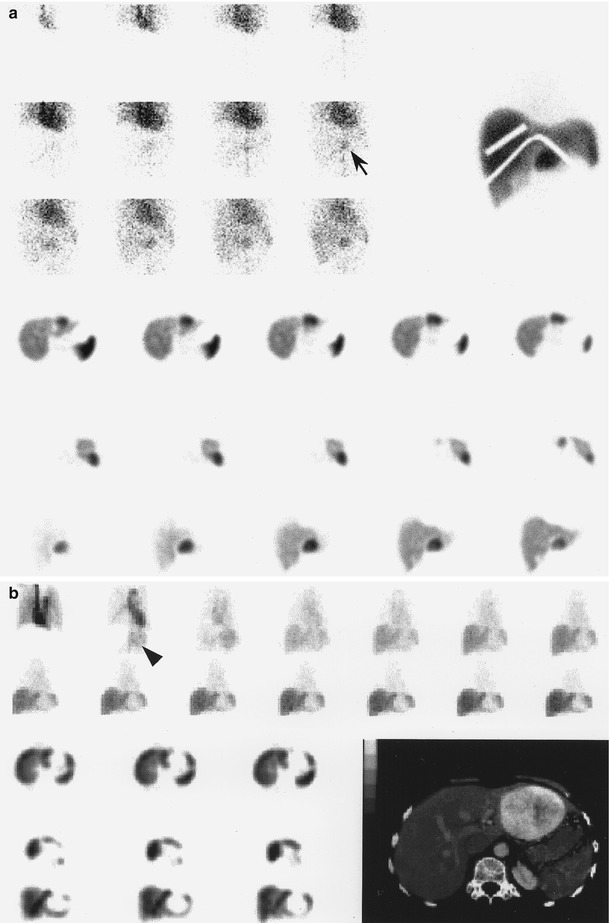
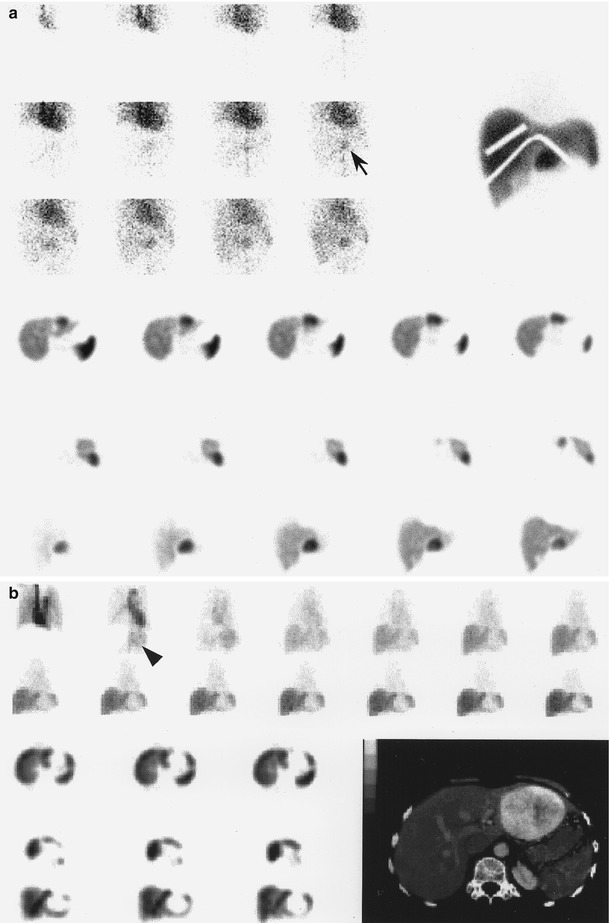
Fig. 17.5
(a, b) Tc-99m sulfur colloid studies in two cases of focal nodular hyperplasia. While both case a and case b show increased early arterial flow (arrow, arrowhead), colloid uptake is increased in case a and decreased in case b on delayed views (reprinted from Kim et al. [261] with permission)
Thirty to seventy percent of FNHs have either normal or increased Tc-99m-colloid uptake (Fig. 17.5a) [32, 53, 54], reflecting the variable quantity of Kupffer’s cells. Decreased Tc-99m-colloid uptake may be seen in approximately one-third of cases (Fig. 17.5b) [53, 54]. Because of the presence of hepatocytes in FNH, Tc-99m-IDA scintigraphy has also been evaluated for the diagnosis of FNH. Of 25 FNHs in a study, 19 (76 %) showed hyperperfusion during the flow phase and 23 (92 %) appeared as focal regions of increased uptake during the clearance phase of hepatobiliary imaging. Normal sulfur colloid uptake was seen in 16 (64 %) [29]. The detectability of FNH by Tc-99m-IDA scintigraphy was 92 %, greater than that of CT (84 %) or MRI (84 %).
17.4.2.4 Hepatocellular Adenoma
Hepatocellular adenomas typically appear as photopenic defects on Tc-99m-colloid scintigraphy. In the past, this was attributed to the absence of Kupffer’s cells [55]. However, a pathological study demonstrated that all hepatic adenomas studied contained Kupffer’s cells [56]. Yet most of these lesions (77 %) did not demonstrate Tc-99m-colloid uptake for unknown reasons. The authors found no significant histological difference between those lesions that accumulate colloids and those that do not. They also suggested that adenoma should be added to the differential diagnosis of a hepatic lesion with Tc-99m-colloid uptake because of the presence of uptake in 23 % of their cases.
17.5 Evaluation of Biliary Tract Diseases
Bile flowing through the common hepatic duct may flow either into the gallbladder or through the common bile duct (CBD) into the duodenum. The quantity of bile flowing in either direction is determined to a major degree by the pressure developed by the sphincter of Oddi. In normal individuals, bile flows into the gallbladder when the sphincter of Oddi is contracted. Foods containing lipids and amino acids enter the duodenum and cause release of endogenous cholecystokinin (CCK) from the duodenum to the upper jejunum, which in turn contracts the gallbladder, dilates the sphincter of Oddi, and increases bile secretion from the hepatocytes. All of these enhance the flow of bile into the duodenum.
On a typical normal cholescintigram performed with Tc-99m-IDA agents, the CBD and gallbladder are visualized 10–20 min following the intravenous administration of Tc-99m-IDA (Fig. 17.6). Visualization of the small bowel varies depending on the sphincter tone and the degree of gallbladder filling.
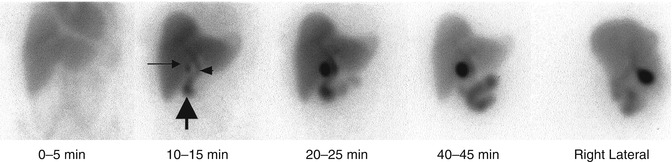
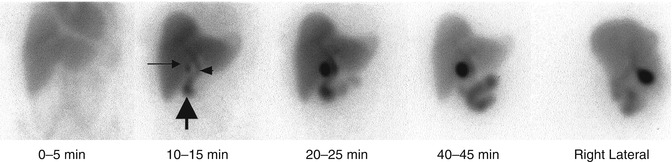
Fig. 17.6
Normal hepatobiliary scan. Hepatic uptake is prompt. The CBD (short arrow), gallbladder (long arrow), and duodenum (thick arrow) are visualized within 15 min following intravenous administration of Tc-99m-IDA
Several drugs, including cholecystokinin (CCK), morphine, and phenobarbital, have been used to alter biliary kinetics at different levels (i.e., hepatocytes, gallbladder, and/or sphincter of Oddi) in an effort to increase the efficacy of hepatobiliary imaging. Sincalide, a synthetic C-terminal octapeptide of CCK, has been used in the diagnosis of acute cholecystitis in order to empty the gallbladder before cholescintigraphy, so that gallbladder filling can be enhanced during the study if the cystic duct is patent. These agents are also used to evaluate gallbladder ejection fraction (GBEF) and/or sphincter of Oddi response in patients with suspected chronic, acalculous biliary tract diseases to determine who might benefit from cholecystectomy or sphincterotomy.
17.5.1 Acute Cholecystitis
Although it is generally known that acute cholecystitis in 90–95 % of cases begins with obstruction of the neck of the gallbladder or the cystic duct by a gallstone, some authors feel that obstruction does not necessarily lead to acute cholecystitis [57]. Nevertheless, obstruction is present in almost all cases of acute cholecystitis. There are other important factors in the pathogenesis of acute cholecystitis, including chemical factors such as prostaglandins [58] and bacterial growth [59]. Injury to the gallbladder mucosa by a mechanical or chemical factor stimulates the epithelial cells to secrete fluid. Active fluid secretion in the obstructed gallbladder lumen increases the intraluminal pressure, which may cause impairment of circulation and ischemia of the gallbladder mucosa and wall. Distention of the gallbladder further enhances formation of prostaglandin, establishing a vicious cycle [60]. Active fluid secretion in the gallbladder wall is markedly reduced by morphine. The acceleration of the process can be reduced by morphine [61].
Approximately 60–70 % of patients report prior attacks that resolved spontaneously. The factors regulating the intraluminal pressure may determine the course of an attack of acute cholecystitis. Of the 75 % of patients with acute cholecystitis who experience remission of symptoms, approximately one quarter will experience a recurrence of cholecystitis within 1 year, and 60 % will have at least one recurrent attack within 6 years [62]. Therefore, the histological pattern of acute cholecystitis is superimposed upon chronic inflammatory changes in at least 90 % of cholecystectomy specimens [63].
Acalculous acute cholecystitis is less common (5–10 %). Despite the absence of gallstones, the cystic duct is frequently obstructed, though the mechanism remains unclear. Precipitating factors include severe trauma or burns, the postpartum period following prolonged labor, a major operation, prolonged parenteral hyperalimentation, vasculitis, obstructing tumor of the gallbladder, and parasitic infestation of the gallbladder. It also may be seen with a variety of other systemic diseases (sarcoidosis, cardiovascular disease, tuberculosis, syphilis, actinomycosis, etc.) [62]. Save for the absence of stones, the pathology of acalculous and calculous cholecystitis is essentially identical [64].
Acute cholecystitis is the most common indication for cholescintigraphy, which is considered the procedure of choice for its diagnosis [65]. Generally, nonvisualization of the gallbladder up to 4 h after radiotracer administration or within 30 min after the administration of morphine sulfate is interpreted as consistent with cystic duct obstruction, provided that there is normal hepatic uptake and excretion. Gallbladder visualization anytime during imaging virtually excludes the presence of acute cholecystitis.
Meta-analysis of 2,466 patients showed a sensitivity of 97 % and specificity of 90 % [65]. Conventional imaging protocols frequently require delayed imaging for up to 4-h postinjection [66] or even up to 24 h in patients with severe intercurrent disease [67] to achieve a sufficiently high level of accuracy. Delayed imaging is logistically inconvenient. It can be potentially disadvantageous to the patient, and it may not be feasible in some clinical settings. Efforts to increase the specificity of the test and/or to shorten the total imaging time were made using pharmacological interventions, which include morphine augmentation [68] and CCK pretreatment [69].
Despite the superiority of cholescintigraphy over ultrasonography for evaluation of acute cholecystitis that has been known since almost 30 years ago [70] and confirmed repeatedly even after the turn of this century [71, 72], the latter is still often the first diagnostic test being ordered in many institutions. A most recent (and seemingly largest) meta-analysis report, including 57 studies and 5,859 patients, published in 2012 confirmed that cholescintigraphy has the highest diagnostic accuracy of all imaging modalities in the detection of acute cholecystitis [73]. The authors reported that diagnostic accuracy of US has a substantial margin of error.
17.5.1.1 Morphine Augmentation Versus Delayed Imaging
Bile is secreted continuously from the liver into the biliary system. The proportion of bile flowing into the gallbladder or the duodenum depends on the relative resistance to flow determined mainly by the contractile state of the gallbladder and the sphincter of Oddi. The resistance of the sphincter of Oddi is considered the principal factor in the regulation of the intracholedochal pressure and of the common bile duct-gallbladder pressure gradient [74]. The administration of morphine sulfate (morphine) results in contraction of the sphincter of Oddi. This, in turn, causes an increase in the intraductal pressure and forces the bile to flow into the gallbladder if the cystic duct is patent [75, 76]. A widely used protocol involves the administration of 0.04 mg/kg morphine intravenously over 3 min at 1 h after the injection of radiotracer, provided that activity is seen in the bowel. Generally, morphine is not administered during the first hour because (1) the gallbladder is visualized within 1 h in the majority of patients undergoing cholescintigraphy and (2) delayed filling of the gallbladder or delayed excretion into the bowel, suggesting the presence of chronic cholecystitis or other biliary tract disease, could be missed by administering morphine early. After morphine administration, imaging is continued for an additional 30 min. Typically, the gallbladder is visualized within 30 min if the cystic duct is patent (Fig. 17.7). If visualization does not occur within 30 min, the findings are interpreted as consistent with acute cholecystitis. Therefore, the entire study can be terminated at 90 min in contrast to 4 h or more with conventional delayed imaging without morphine augmentation.
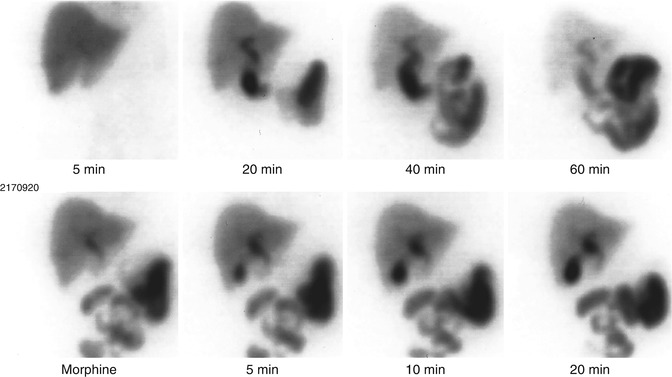
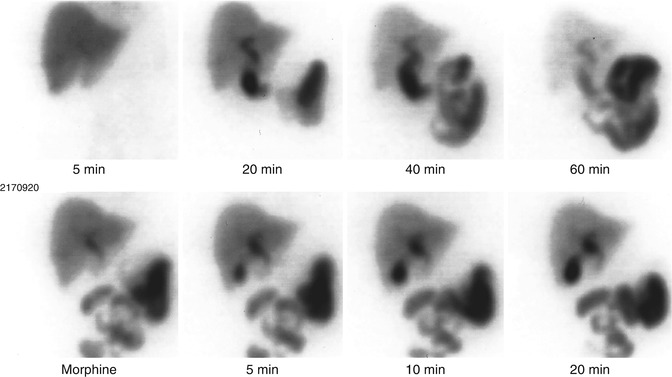
Fig. 17.7
The CBD and small bowel are promptly visualized in this study with Tc-99m-IDA, but the gallbladder is not visualized up to 60 min. Following morphine administration, the gallbladder filled promptly, excluding cystic duct obstruction
Following the introduction in 1984 of morphine-augmented cholescintigraphy by Choy et al. [68], as an alternative to delayed imaging, a number of reports were published on this subject [77–87]. The general conclusion in most early reports, in terms of efficacy, was that the two tests were diagnostically equivalent [77–81]. Morphine augmentation was recommended primarily because of its logistic advantage (a short imaging time). However, the reported efficacy of morphine augmentation was based primarily on data excluding cases of early GB visualization without morphine. In contrast, patients with early GB visualization (<1 h) were included in those early reports evaluating the efficacy of conventional cholescintigraphy with which the efficacy of morphine augmentation was compared. A reanalysis of published data (after excluding the cases with early gallbladder visualization from previous reports) indicated that delayed imaging has a significantly lower specificity (53 % average: 33–94 %) for acute cholecystitis than morphine augmentation (85 % average: 69–100 %) [86]. The sensitivity is still excellent at 98 % (98–100 %). Another meta-analysis using a different statistical approach yielded nearly identical results and confirmed the higher specificity of the morphine-augmented technique than that of delayed imaging (84 % vs. 68 %) [87].
A number of potential shortcomings associated with morphine augmentation were reported [80], including false-positive studies occurring in patients with chronic cholecystitis or hepatocellular disease or in other severely ill patients [77, 86, 88]. However, this problem is not unique to morphine augmentation. It also occurs with delayed imaging [67, 89, 90] and can be even more serious. Whereas some investigators [80] have suggested more delayed imaging in addition to the 30 min after morphine administration to reduce false-positive examinations, others [77] found no additional benefit in imaging up to 1 h instead of 30 min. Secondly, in patients with acute acalculous cholecystitis or with the “dilated cystic duct sign,” increased intraluminal pressure following morphine administration may potentially result in more false-negative studies than delayed imaging [78]. However, there is no significant difference in the sensitivity or the negative predictive value between delayed imaging and morphine augmentation [86, 87]. This indicates that the occurrence of false-negative studies associated with acute acalculous cholecystitis or the dilated cystic duct sign is not frequent enough.
17.5.1.2 Sincalide Preadministration for the Diagnosis of Acute Cholecystitis
Administration of CCK prior to injection of Tc-99mIDA will induce gallbladder emptying with a reduction of intraluminal pressure. It was introduced as a means of reducing potential false-positive results for acute cholecystitis and of shortening the total imaging time [69, 91]. Eikman et al. [92] attributed the improved efficacy of cholescintigraphy in their series to CCK pretreatment. The rationale of this approach is that gallbladder emptying before initiating the study is generally followed by more reliable gallbladder filling during the cholescintigraphy. In a series reported by Kim et al., approximately 50 % of volunteers who had paired studies showed greater gallbladder filling after sincalide pretreatment [93]. Although sincalide pretreatment of all patients may not be necessary, it is often used in conditions such as alcoholism and total parenteral nutrition and during a prolonged fasting state [94, 95], because functional resistance to tracer inflow may result from distention of the gallbladder with viscous contents. Fasting for 24 h or longer is a routine indication for the preadministration of sincalide in many laboratories.
It should be noted that a meticulous sincalide infusion technique is important to ensure good gallbladder emptying, not only for the gallbladder ejection fraction measurement (which will be discussed later) but also for the pretreatment. For the latter, it appears that less attention has been paid to the administration technique, perhaps because imaging is not performed during sincalide infusion and gallbladder emptying. A 30- to 45-min infusion is logistically inconvenient for pretreatment, unlike that for the measurement of gallbladder ejection fraction. A 3-min infusion at the physiological rate of 3.3 ng/kg/min [3], or an infusion for up to 10 min at the same or slightly lower rate approximately 30 min before injection of Tc-99m-IDA, is probably adequate for this application.
Some investigators believe that CCK preadministration decreases specificity and suggest that CCK not be given or, if given, that a minimum of 4 h should pass before a Tc-99m-IDA study is begun [96]. Further studies seem to be warranted to resolve this issue.
17.5.1.3 Sincalide Pretreatment Versus Morphine Augmentation
Reports by Chen et al. and Kim et al. [97, 98] show that morphine administration helps to visualize the gallbladder in 32–42 % of patients with gallbladder nonvisualization at up to 60–90 min despite sincalide pretreatment. These results suggest that sincalide pretreatment alone is not sufficient to detect all patent cystic ducts.
17.5.1.4 Potential Causes of False-Positive Results
Insufficient fasting will result in gallbladder contraction induced by circulating endogenous CCK, thereby inhibiting bile flow into the gallbladder. Therefore, the gallbladder may not visualize even in normal subjects (up to 64 %) in the nonfasting state [99]. A minimum of 2–4-h fasting is required before cholescintigraphy is performed for the evaluation of acute cholecystitis.
As discussed earlier, false-positive results can occur in conditions such as a prolonged fasting state, alcoholism, and total parenteral nutrition [94, 95].
Activity retained in the duodenum or dilated right renal pelvis may cause confusion. Conversely, activity in the gallbladder may not be clearly separated from that in the duodenum. In either situation, a right lateral view can be helpful: The gallbladder appears as an anteriorly positioned structure. If the right lateral view does not resolve the situation, a left anterior oblique view can clarify the question. Alternatively, water ingestion often clears duodenal activity [100, 101].
With normal hepatic function and normal clearance of Tc-99m-IDA, there is generally decreased tracer activity in the liver parenchyma at the time of morphine administration or delayed imaging, i.e., generally 1 hour after administration of the tracer. With this in mind, it has been reported that since little activity is available for gallbladder visualization, there is the potential of a false-positive result. Therefore, past authors recommended injection of an additional 2–3 mCi of radiotracer, a “booster dose,” when minimal residual hepatic activity was noted before morphine-augmented or delayed imaging [69]. This recommendation was probably legitimate in the analog era with hard-copy imaging on film. Back then, the image intensity was preset and optimized to look at entire structures, including the liver during the early phase, biliary system, and often intense uptake in the gallbladder and intestine. As a consequence, it was quite common to see little remaining activity in the liver parenchyma during the late phase on these analog hard-copy images. However, now with the advent of digital imaging on the computer screen, the intensity of the organ or region of interest can be freely adjusted and optimized. Hence, we believe that gallbladder filling can readily be identified, presuming the cystic duct is patent, without administering a booster dose.
Radioactivity may be seen in a dilated cystic duct proximal to the site of obstruction in patients with acute cholecystitis [102]. This should not be mistaken for a small gallbladder.
In case the study shows findings compatible with CBD obstruction or severe hepatocellular dysfunction with no or little bile excretion, nonvisualization of the gallbladder should be interpreted with caution as the presence of acute cholecystitis cannot be reliably determined.
Holbrook et al. [103] and Chandramouli et al. [104] reported that the gallbladder was not visualized in 18 of 62 patients (30 %) and nine of 12 patients (75 %), respectively, after sphincterotomy. These results indicate a significant alteration of bile flow due to sphincterotomy, which can affect the specificity of hepatobiliary scintigraphy for the diagnosis of acute cholecystitis.
Jacobson et al. reported that a considerable proportion of patients who had normal IDA scans developed abnormalities such as impaired liver uptake, gallbladder nonvisualization, etc., following bone marrow transplantation [105]. Nevertheless, no patient developed clinical or laboratory evidence of acute cholecystitis. These cholescintigraphic abnormalities may be due to the combined effects of hepatotoxic chemoradiation therapy, graft-versus-host disease, and prolonged parenteral alimentation.
17.5.1.5 Variants Associated with CCK Preadministration and Morphine
Significantly delayed tracer excretion into the bowel associated with prompt and progressive gallbladder filling can be a normal variant seen in the fasting state [106]. Morphine administered to the patient prior to the study can have the same result. This finding is well known and is now actually used in a positive way to enhance gallbladder visualization during cholescintigraphy.
In a series by Kim et al., approximately 40–50 % of subjects with prompt gallbladder filling showed a markedly delayed biliary-to-bowel transit after sincalide pretreatment (Fig. 17.8) compared with only 4 % of patients who did not receive sincalide [93]. Delayed biliary-to-bowel transit, when present, should not necessarily be read as abnormal, i.e., as hyperacute or partial CBD obstruction. However, a hyperacute or partial CBD obstruction may not be totally excluded in certain clinical settings, although this pattern, with intact gallbladder visualization, is not typical of CBD obstruction. In such a situation, CCK administration can help to exclude CBD obstruction by inducing gallbladder contraction and demonstrating bowel activity [93, 107]. We [108] assessed the frequency of the need for sincalide administration in this situation to exclude CBD obstruction. Delayed or no excretion into the bowel after sincalide administration was seen only in patients with delayed clearance of liver parenchymal activity but never in patients with prompt clearance. It appears that if both gallbladder filling and clearance of liver parenchymal activity are prompt, then the study can be terminated without giving CCK, despite the absence of bowel activity.
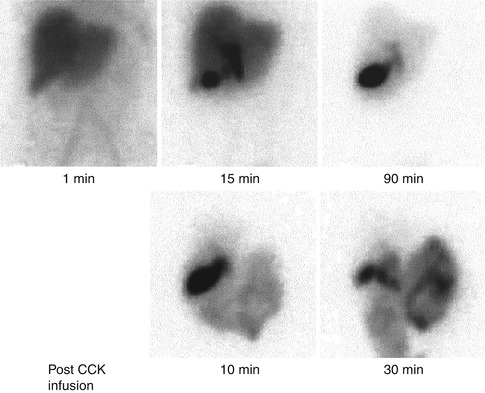
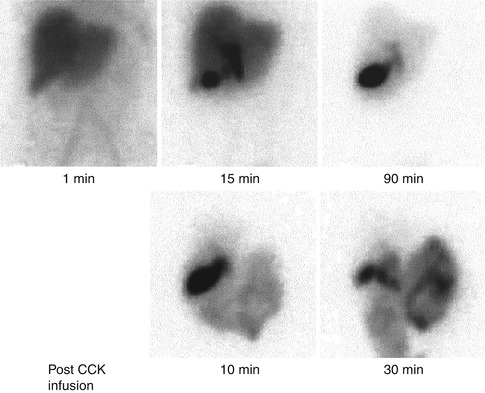
Fig. 17.8
The patient was pretreated with sincalide before receiving an injection of Tc-99m-IDA. The gallbladder filling is prompt but bowel activity is not identified until 90-min postinjection. Following administration of a second dose of sincalide, there is prompt tracer excretion into the bowel, which excludes common duct obstruction
Oates et al. [109] and Shih et al. [110] reported that morphine administration increases the frequency and the degree of duodenogastric reflux.
Kim et al. [111] reported variable bile retention on cholescintigraphy following morphine administration for the evaluation of acute cholecystitis. No significant effect of 2 mg of intravenous morphine on biliary kinetics was detected scintigraphically in a considerable proportion of patients. Also, there was considerable variation in the duration of the effect of morphine, when present. Preliminary data indicate that GB nonvisualization after morphine administration with the pattern of continually decreasing CBD activity is not as reliable for the diagnosis of acute cholecystitis as is nonvisualization of the GB with a pattern of increasing CBD activity [112].
17.5.1.6 Ancillary Findings
Increased IDA activity in the liver parenchyma around the gallbladder fossa is called a “rim sign” (Fig. 17.9). The presence of this sign is frequently associated with acute cholecystitis, which is often complicated, i.e., gangrenous gallbladder [113–118]. This pericholecystic activity appears to be caused by increased blood flow to [113] and/or delayed bile excretion from inflamed liver parenchyma adjacent to an inflamed gallbladder [118]. At times, a rim sign with marked tracer retention may mimic the gallbladder appearance (patient 3 in Fig. 17.9), in which case the presence of such activity on the early images before the appearance of bile duct activity can help to exclude the possibility of gallbladder filling. The rim sign, though suggestive of acute cholecystitis, is not sufficiently specific to obviate morphine augmentation or delayed imaging [63, 119].
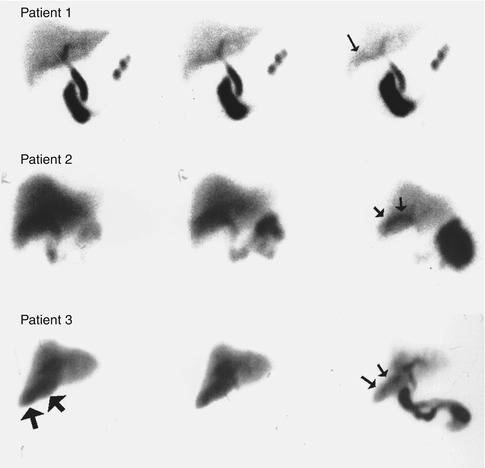
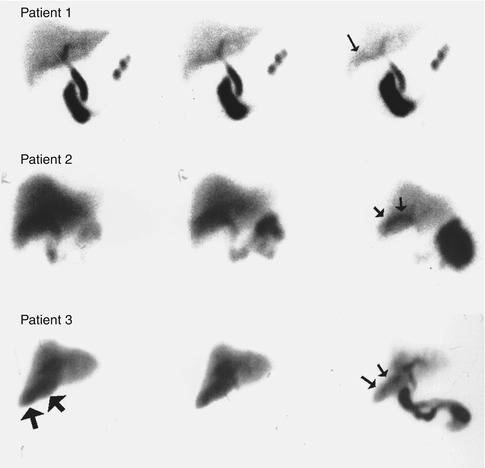
Fig. 17.9
A spectrum of rim signs. A mild rim sign is seen in the Tc-99m-IDA study of patient 1 (arrow). The rim sign in patient 2 is quite prominent and clearly seen as a rim. The rim sign in patient 3 is more diffuse and may be confused with the gallbladder. However, this activity is present on the early image (large arrows) even before the tracer activity appears in the bile ducts (reprinted from Kim [46] with permission)
In summary, in addition to its logistic advantage (shortening the imaging time), morphine augmentation provides more specific diagnosis for acute cholecystitis than does delayed imaging. Sincalide pretreatment, when administered at the physiological rate, will be helpful in conditions in which functional resistance to tracer flow into the gallbladder may be present. However, morphine augmentation will further improve the efficacy of the test even after sincalide pretreatment. The technique is therefore recommended for routine clinical use when the gallbladder is not visualized at 1 h.
17.5.2 Chronic Acalculous Biliary Diseases
Approximately 98 % of patients with symptomatic gallbladder disease have gallstones. Occasionally, patients have signs and symptoms of gallbladder disease, but no stone can be demonstrated by repeated ultrasound or oral cholecystography [120]. Chronic biliary-type pain in patients with no stones may be due to chronic acalculous biliary disorders, including chronic acalculous cholecystitis, cystic duct syndrome, a functional disorder such as gallbladder dyskinesia, and sphincter of Oddi dysfunction. Nonbiliary disease such as the irritable bowel syndrome may cause the same symptoms. Sincalide has been used for the evaluation of gallbladder ejection fraction (GBEF) or sphincter of Oddi response in this patient group to determine who might benefit from cholecystectomy, sphincterotomy, or smooth muscle relaxants.
The technique for administration of sincalide is of the utmost importance. The degree of gallbladder emptying is dependent on the CCK dose and rate of administration, as well as on the total number of receptors in the gallbladder wall smooth muscle. Spasm of the neck of the gallbladder and decreased GBEF may occur due to unphysiologically high serum levels of sincalide following a bolus injection [121]. This paradoxical response is attributable to the different threshold level of the CCK receptors in the body and fundus of the GB and cystic duct [122]. The cystic duct does not contract when the dose of CCK is physiological. Therefore, this agent should not be given as a bolus. Although infusion of 20 ng/kg sincalide over 2–4 min (an average dose rate of 6.6 ng/kg/min) was once a popular technique [123–127], this dosage protocol has also been demonstrated to be unphysiological [3, 128]. Aside from frequent incomplete gallbladder emptying, infusion of 20 ng/kg over 3 min or less is often associated with such side effects as abdominal discomfort, pain, and nausea.
Comparison of various sincalide doses for a 3-min infusion technique demonstrated that 10 ng/kg (the rate of 3.3 ng/kg/min) produces maximal gallbladder emptying [3]. With further increase of the dose rate, i.e., 20 ng/kg/3 min, the GBEF actually decreases. The normal GBEF value using 10 ng/kg/3 min was established as greater than 35 %. Falsely reduced GB emptying associated with a 3-min infusion of 20 ng/kg of sincalide is illustrated well in Fig. 17.10 [129]. However, Ziessman et al. showed that even the infusion at a so-called physiological rate (10 ng/kg infused over 3 min) produces an excessively variable GBEF response to establish a clinically useful normal range compared with the same dose infused over a longer period, i.e., 10 ng/kg infused for 60 min [130]. Normal and low GBEF values were reported to be reproducible in long-term studies [131]. Various dose rates, durations, and normal GBEF values were employed by other investigators [132–134]. Although the optimal dose and duration of infusion is the subject of some controversy, a long infusion seems to produce more complete gallbladder emptying and less severe side effects than a short infusion, probably due to the 2.5-min plasma half-life of sincalide. When performing and interpreting sincalide-augmented hepatobiliary imaging, it is important to adhere to a specific sincalide infusion technique and to use normal GBEF values that have been validated for that particular method. Recently, an interdisciplinary panel suggested that the optimal sincalide infusion method is 20 ng/kg/60 min with 38 % as the lower limit of normal GBEF [135].
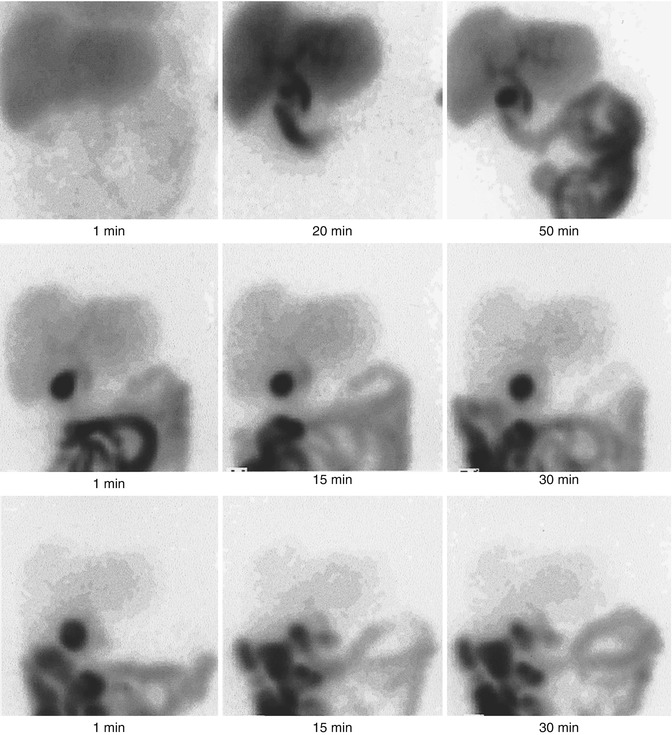
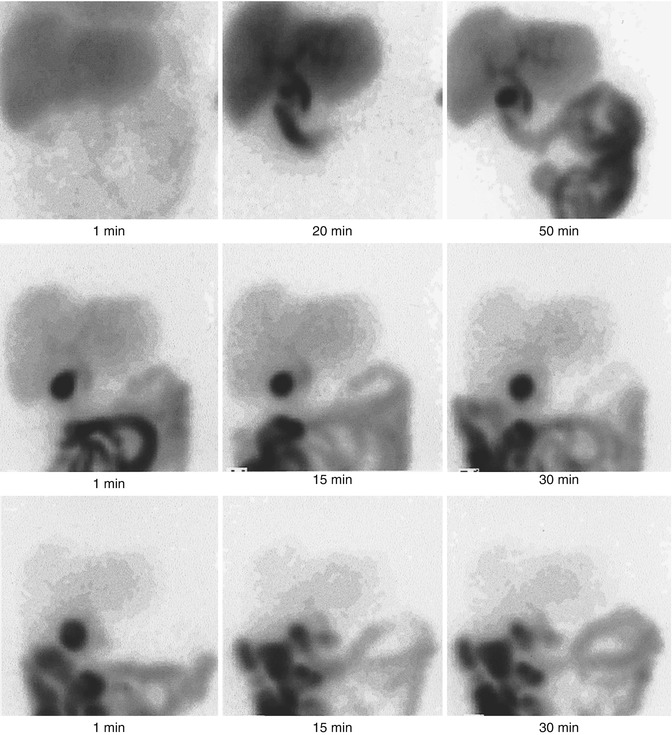
Fig. 17.10
A hepatobiliary scan using Tc-99m-IDA performed in a patient with suspected chronic acalculous biliary disease. The scan shows prompt visualization of the GB and small bowel (top row). Following a 3-min infusion of 20 ng/kg sincalide, the GB is poorly contracted, with an EF of approximately 10 % (middle row). Immediately after this, a 10-min infusion of the same dose produced a GBEF of 80 %
Various fatty meals have been evaluated as an alternative to sincalide [136–139]. However, controversy exists over the use of fatty meals versus sincalide. The major disadvantage of meal stimulation is that an abnormal GB response may result from factors other than the GB, such as poor gastric emptying, pancreatic insufficiency, celiac disease, or abnormal bowel transit [140–143]. The onset of meal-induced GB emptying can also vary during different phases of the migrating motor complex at the time of ingestion [144]. The choice between fatty meal and sincalide can probably be made on the basis of the population being studied. Meal stimulation would be preferable when GB function in relation to the rest of the GI tract needs to be evaluated. However, evaluation of GB function independent of the digestive process may be better achieved with sincalide when different patient populations are studied [145]. Nonetheless, a fatty meal can serve as an alternative in the case that sincalide is not available for clinical use. However, when used, careful attention should be paid to the fat content, texture, taste, manner of administration, and measurement time sequence, all of which need to be standardized [146]. Normal values for each center must be established when choosing a meal.
17.5.2.1 Chronic Acalculous Gallbladder and Cystic Duct Diseases
The pathological findings of chronic acalculous cholecystitis are nearly identical to those of chronic calculous cholecystitis, except for the absence of stones [147]. Intermittent acalculous cystic duct obstruction and chronic ischemia with active inflammatory changes have both been postulated as possible pathogenic mechanisms. The cystic duct syndrome results from a partial acalculous obstruction or narrowing of the cystic duct [148], which may be due to fibrosis, kinking, or adhesion [69]. A sphincter-like mechanism in the cystic duct may explain the possibility of cystic duct occlusion in the absence of mechanical obstruction [74]. The cystic duct syndrome and chronic acalculous cholecystitis often coexist [123, 132, 149], but they may also occur independently.
In functional disorders, or gallbladder dyskinesia, the gallbladder is histologically normal. The mechanisms have not been fully elucidated. Abnormal and/or inhomogeneous CCK receptors within the gallbladder, which cause a paradoxical or inhomogeneous response to cholecystokinetic agents, were suggested as a possible mechanism [123, 150]. In this condition, right upper quadrant pain occurs following meals as a result of increased intraluminal gallbladder pressure. Other possible mechanisms of impaired gallbladder motility include a primary smooth muscle disorder and altered release of endogenous CCK [74].
In cholesterosis, the mucosa of the gallbladder is studded with minute yellow lipid flecks, producing the strawberry appearance [151]. In some patients suspected of having chronic acalculous biliary disease, cholesterosis has occasionally been the only histological finding, without evidence of other diseases [124, 152, 153]. Although cholesterosis is not often of clinical significance [151], cholecystectomy is indicated when the condition is symptomatic [62].
There is controversy regarding the value of GBEF for the diagnosis of these diseases and its correlation with histopathology. While some investigators found abnormal pathology in most patients with a low EF [123, 127, 132], others did not [133, 154, 155]. However, some investigators have found no correlation even between histopathological findings and symptomatic relief following surgery [126, 153, 154, 156]. Whether or not the GBEF is a good predictor of symptomatic relief after surgery should be more clinically relevant than the correlation between GBEF and histopathology. Although there was a report of a poor correlation in this regard [154], the vast majority of other reports have demonstrated a good symptomatic response after surgery in most patients with a low GBEF [123–126, 132, 134, 153, 156–159]. Among these reports, there was a randomized trial by Yap et al. [119], which is reassuring. As in adults, children with chronic abdominal pain and delayed gallbladder emptying on CCK-stimulated cholescintigraphy were also reported likely to benefit from cholecystectomy [160].
On the other hand, the effectiveness of a normal GBEF as a predictor of clinical outcome is more difficult to assess, because only highly selected patients (those with higher clinical suspicion) with a normal EF were sent for surgery. The majority of patients with a normal EF who are placed on medical treatment for nonbiliary gastrointestinal diseases do well [123, 127, 154, 157]. However, at the same time, the majority of patients who had surgery despite a normal EF also had symptomatic relief [123, 126, 132, 134]. These results are not surprising, as a 70–75 % cure rate is associated with cholecystectomy even when based on symptoms alone [161]. We have been reporting a GBEF of 40–60 % as indicating an intermediate probability of symptomatic relief following cholecystectomy. Similarly, Majeski suggested that cholecystectomy may be considered for patients with a GBEF between 35 and 60 % if the patient’s symptoms were classic for biliary disease and have been present for 1 year [159].
Several earlier reports suggested that pain reproduction induced by sincalide infusion is another useful positive sign of pathology [126, 162]. A brief infusion (i.e., 20–40 ng/kg over 3 min) was employed by these investigators. However, Kloiber et al. [145] and Yap et al. [132] did not detect pain reproduction in patients who benefited from surgery when a slow infusion (over 45–60 min) technique was used.
Conditions that may affect gallbladder contractility should be borne in mind when using CCK. Atropine significantly reduces the gallbladder ejection period and EF [163]. Gallbladder contractility can be decreased after or during octreotide therapy [164, 165]. An association between gastroesophageal reflux disease and gallbladder function was reported [166]. These authors found abnormal GB function in 58 % of patients with gastroesophageal reflux disease, with improved GB function in most of those patients after fundoplication. A markedly lower GBEF was found in seven of ten patients with achalasia compared with controls [167]. The mechanism and clinical significance of this finding are uncertain. Other reported causes of reduced gallbladder ejection fraction are antiulcer gastric surgery particularly when truncal vagotomy is performed [168] and opioid intake immediately before the study [131].
It was reported that normal and low GBEF values are reproducible in long-term studies [131].
In summary, the overall data favor the use of this test for the diagnosis of chronic acalculous gallbladder and cystic duct disease. A low GBEF can probably be interpreted as indicating a high probability for symptomatic relief after surgery, and vice versa. Bayes’ theorem should then be applied, especially for the group with a normal EF, to make a clinical decision according to the posttest probability from a clinical suspicion (pretest probability) and the GBEF (test probability).
17.5.2.2 Sphincter of Oddi Dysfunction
Sphincter of Oddi dysfunction (SOD) can be responsible for approximately 14 % of all postcholecystectomy pain [169, 170]. It is much more common in female patients. SOD can be classified into two broad categories: stenosis (a fixed structural narrowing) and dyskinesia (functional disorder: a primary disorder of tonic/phasic motor activity) [171, 172].
Measurement of the sphincter of Oddi pressure using sphincter manometry is considered the gold standard for the diagnosis of SOD. In patients with sphincter of Oddi dyskinesia, manometry may reveal tachyoddia, retrograde contractions, or a paradoxical response (sphincter of Oddi spasm) to sphincter relaxants such as CCK [173]. When the basal sphincter pressure is elevated, a distinction between stenosis and dyskinesia can be made based upon the response to smooth muscle relaxants [174]. Relaxation after smooth muscle relaxant suggests dyskinesia rather than stenosis. To date, an elevated basal pressure (>40 mmHg) is considered the only consistent manometric criterion which is correlated with patients’ symptoms and also with relief of symptoms with therapy [175].
The treatment of choice for patients with sphincter of Oddi stenosis is endoscopic sphincterotomy. Surgical sphincteroplasty or balloon dilatation of the sphincter of Oddi is less favorable in terms of both complication rate and success in long-term relief of symptoms [175]. In patients with sphincter of Oddi dyskinesia, a pharmacological treatment with calcium channel blocker or long-acting nitrate could be used. Endoscopic sphincterotomy is indicated for patients with elevated basal pressure who do not respond to pharmacological treatment [176].
Depending on the results of laboratory tests and endoscopic retrograde cholangiopancreatography (ERCP), SODs were classified as biliary type I, II, and III [172]. Patients with biliary type I SOD have typical biliary pain, elevated liver enzymes on two or more occasions during episodes of pain, and an abnormal ERCP demonstrating a dilated CBD and delayed emptying of contrast into the small intestines (>45 min). Patients with type II SOD have biliary-type pain and one or two of the other abnormalities mentioned for type I. Patients with type III SOD have only biliary-type pain and none of the other criteria. Manometry is optional in patients with type I, necessary in type II patients, and mandatory in type III patients [172]. Generally, the greater the number of abnormalities (type I), the more likely it is that a structural disorder is present, e.g., stenosis, and vice versa.
Although the accurate diagnosis of SOD is important, ERCP may not detect many patients with functional SOD. Also, a concern was raised about the validity of the 45-min delayed drainage criterion for sphincter of Oddi dysfunction [177]. Sphincter manometry, while being the gold standard, is invasive, difficult to perform, difficult to interpret, and associated with potential complications such as pancreatitis [178].
Hepatobiliary imaging with or without pharmacological intervention has also been shown to be useful in patients with SOD, and investigations have focused primarily on patients after cholecystectomy. A number of parameters have been derived from the time-activity curves of the liver parenchyma, hilum, CBD, entire hepatobiliary tract (liver and bile ducts), and bowel. These include the time of peak activity (Tmax), excretion half-time (T1/2), percentage of excretion at a certain time (i.e., 45, 60 min), excretion rate, and mean transit time. Visual parameters such as the time of first appearance of the intrahepatic biliary tree, and the bowel, CBD emptying, and CBD-to-liver ratio (comparison of CBD activity at 60 min with liver activity at 15 and 60 min) have been added to the above semiquantitative parameters [179].
The experience of most authors has been satisfactory [179–187]. It was reported that choledochoscintigraphy is useful for diagnosing SOD as well as predicting sphincterotomy outcome in biliary type I and II patients, irrespective of clinical classification and manometric findings [188]. Although some investigators did not find cholescintigraphy useful [189, 190], others believe that the discrepancy in the reported efficacies is due to differences in the technique [191]. An especially excellent separation between patients with and without SOD was achieved in three reports, using a single parameter: the Tmax of the entire liver and extrahepatic bile ducts, the T½ of the right hepatic lobe [185, 186], and a combination of the scores from six parameters [179]. Although these authors did not agree on which parameters were the best, in essence, all more or less reflect hepatic parenchymal and biliary-to-bowel transit of bile. These parameters have also been found useful in assessing the benefit of endoscopic sphincterotomy (Figs. 17.11 and 17.12) [180, 186, 189, 192].
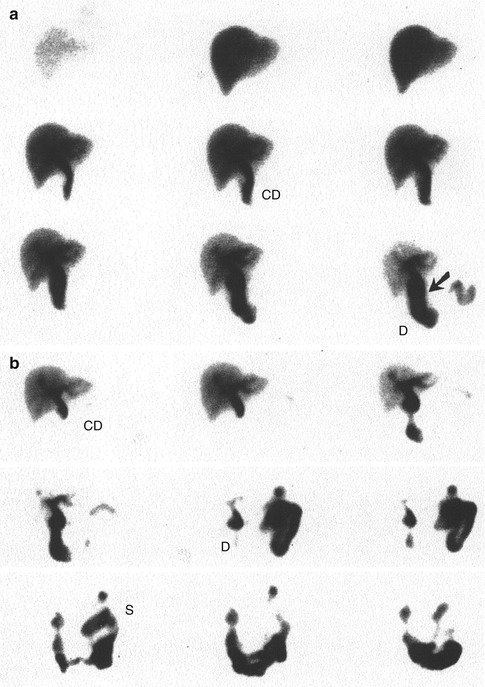
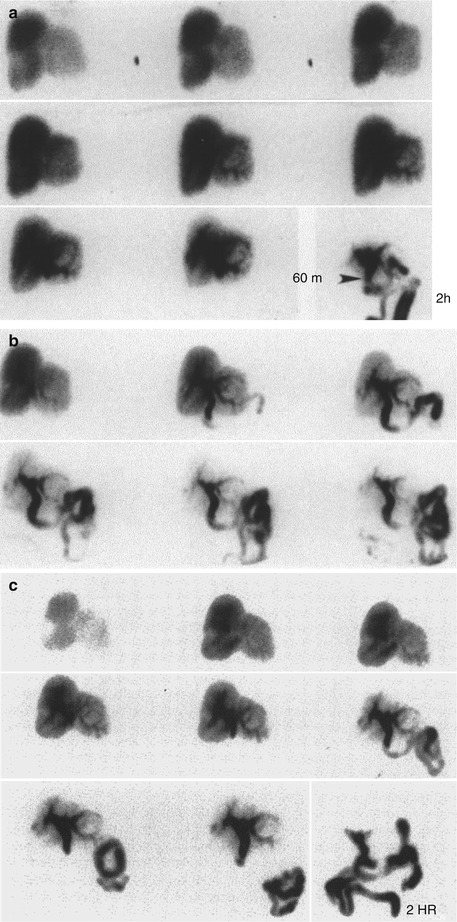
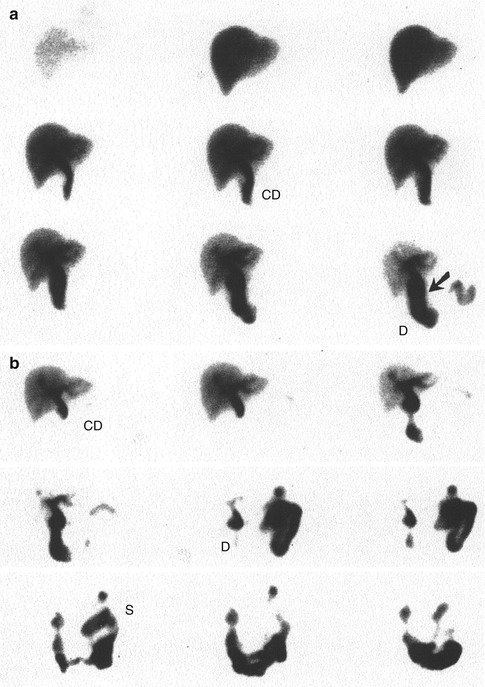
Fig. 17.11
(a, b) SOD: stenosis. This 50-year-old woman was seen at 3 years’ postcholecystectomy with chronic recurrent pain. ERCP showed no mechanical obstruction, but the basal sphincter of Oddi pressure was elevated (45 mmHg). (a) Preoperative cholescintigraphy shows delayed hepatobiliary clearance with retention of activity in the common bile duct (CD) at 60 min (arrow). Increasing activity within the duodenum (D) is noted. A second preoperative study (not shown here) with constant CCK infusion (40 ng/kg/60 min) was not significantly different (i.e., there was a fixed papillary stenosis). (b) Postsphincterotomy study in the same patient shows significant improvement with rapid hepatobiliary and common duct clearance compared with the preoperative study. S, stomach (reprinted from Ziessman [192] with permission)
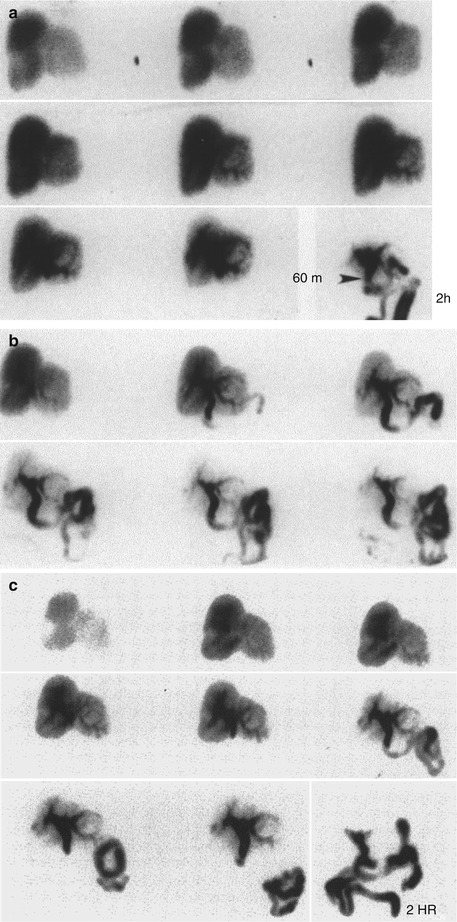
Fig. 17.12
(a–c) SOD: dyskinesia. Postcholecystectomy pain syndrome. An ERCP showed no mechanical obstruction. The sphincter of Oddi pressure was 48 mmHg. A sphincterotomy was performed. a Preoperative study. Sequential analog images over 60 min show a prominent intrahepatic collection system with dilatation in the region of the common hepatic duct at 60 min. A delayed image at 2 h shows that the obstruction is really at the level of the sphincter of Oddi (arrowhead). (b) Preoperative study with a continuous infusion of sincalide, 40 ng/kg/60 min. Hepatobiliary clearance is more rapid than the study without CCK. However, at the end of 60 min, there is retained activity in a prominent common duct. This is an obstructed dyskinetic sphincter of Oddi. (c) Postsphincterotomy study. There is still prominent retention in the common duct, but hepatobiliary clearance has significantly improved since the baseline study (a) and, interestingly, looks similar to the preoperative CCK study (b) (reprinted from Ziessman [192] with permission)
Whereas most of the investigations with scintigraphic studies on this subject have focused primarily on the differentiation between the presence and absence of SOD, Madacsy et al. [193] reported excellent results in discriminating between stenosis and functional dyskinesia. Patients in their series inhaled amyl nitrite, a potent sphincter relaxant, during the washout phase of CBD activity. The rate of CBD washout was slow in both the stenosis and dyskinesia groups before amyl nitrite inhalation and normal in controls. Amyl nitrite inhalation resulted in prompt washout of CBD activity in patients with functional dyskinesia, whereas no change occurred in controls or in patients with organic stenosis (Fig. 17.12). Since the augmentation is started in the middle of CBD washout, this approach clearly cannot be used in conjunction with such parameters as Tmax of liver parenchymal or CBD activity. If such parameters were to be used, then the augmented study would have to be performed on a separate day.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree