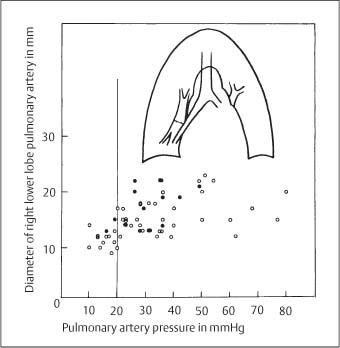
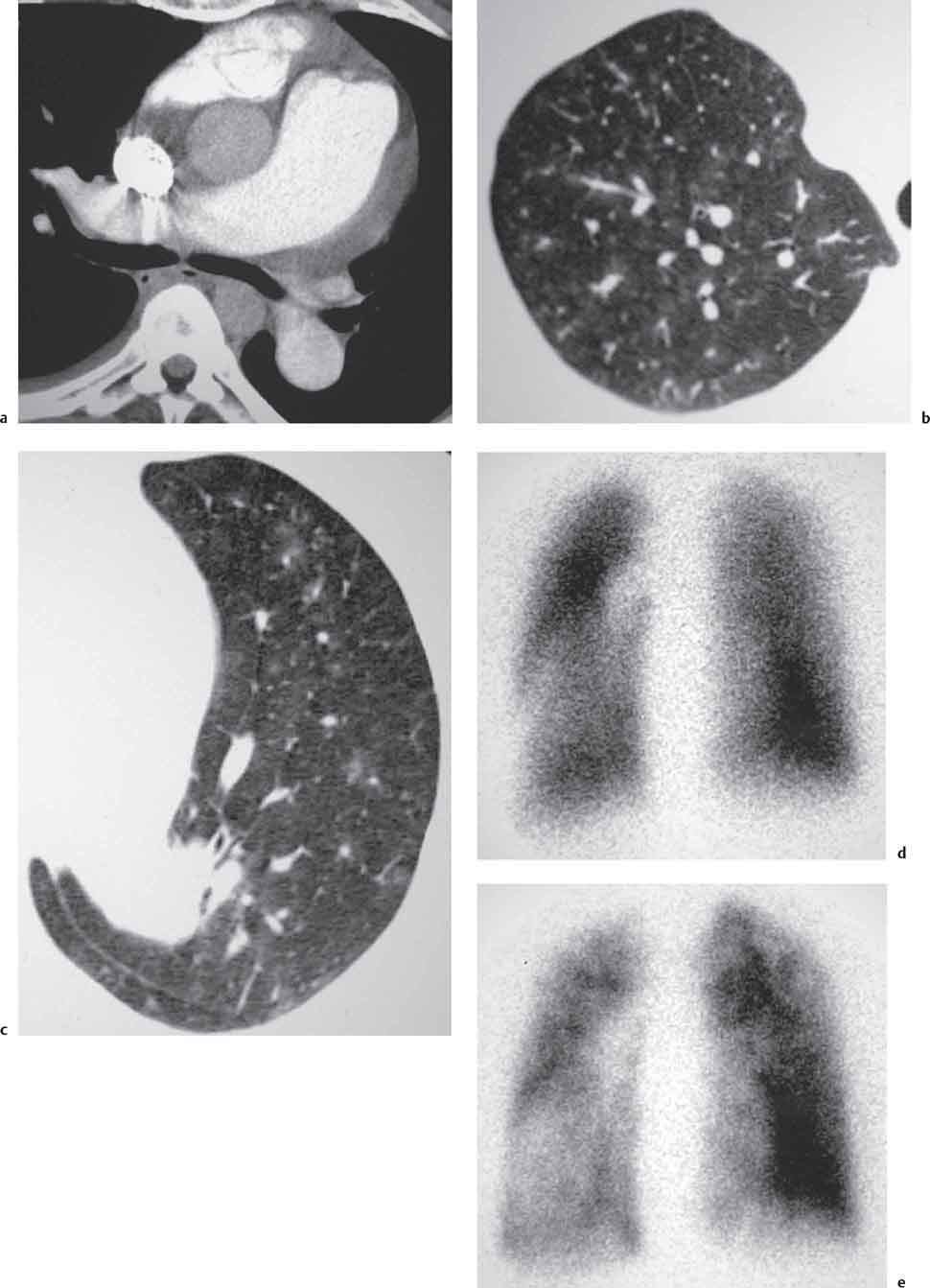
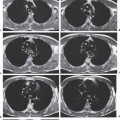
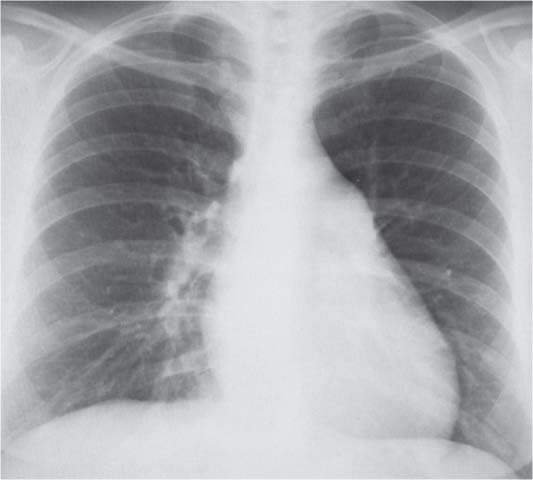
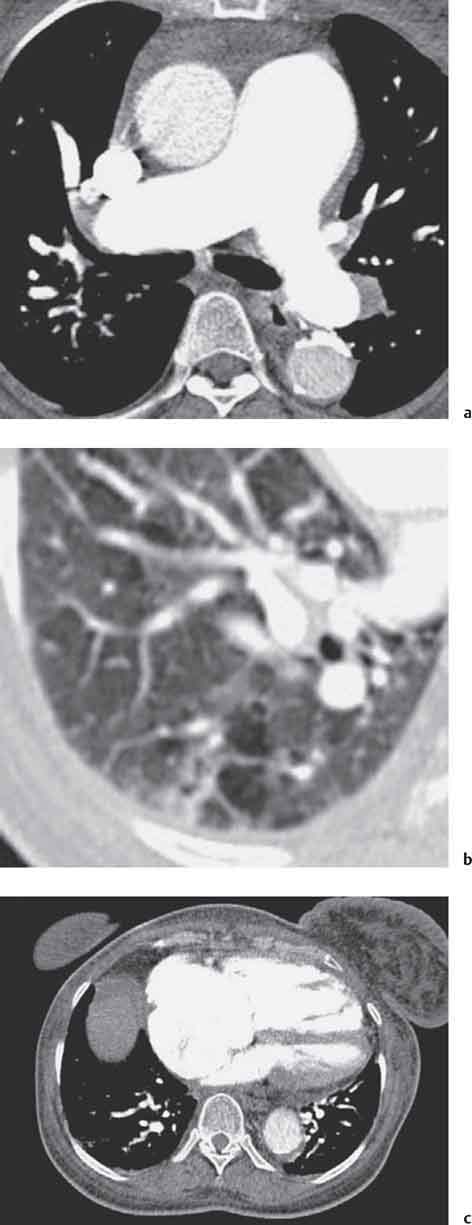
7 Pulmonary Hypertension and Edema Pulmonary arterial hypertension is defined as a mean pulmonary artery pressure of greater than 25 mmHg at rest or greater than 30 mmHg during exercise with increased pulmonary vascular resistance (Burke et al. 1991). Pulmonary artery pressures greater than 70 mmHg are consistent with severe hypertension. Ohm’s Law (Ppa−Ppv = R × I) indicates that chronic elevation of pulmonary arterial pressure (Ppa) may result from increased blood flow (I), increased resistance (R), or an increase in pulmonary venous pressure (Ppv). Pulmonary hypertension may therefore be due to (Table 7.1): • Increased pulmonary vascular resistance (precapillary pulmonary hypertension) in longstanding cardiac left-to-right shunt, chronic thromboembolic disease, pulmonary parenchymal diseases including chronic obstructive pulmonary disease (COPD) and diffuse interstitial pulmonary fibrosis, vasospasm secondary to alveolar hypoventilation, and may be idiopathic in primary pulmonary hypertension (PPH). 60–70% of the pulmonary vascular bed must be occluded before there is an appreciable increase in pressure. • Increased pulmonary venous pressure (postcapillary pulmonary hypertension) is usually secondary to elevated left atrial pressure and may be seen in left ventricular failure, mitral valve stenosis, longstanding left atrial myxoma, or may be idiopathic in pulmonary veno-occlusive disease (PVOD) (Table. 7.1). Table 7.1 Classification of pulmonary hypertension Changes seen in all forms of precapillary pulmonary hypertension include intimal cellular proliferation and medial smooth muscle hypertrophy. These changes are characteristically seen in the muscular arteries. In addition, plexiform lesions and necrotizing arteritis are seen in primary pulmonary hypertension and in pulmonary hypertension secondary to a cardiac shunt. A plexiform lesion is defined as a focal disruption in the internal elastic lamina of a muscular artery by a “glomeruloid” plexus of endothelial channels which proceed to ramify into alveolar septal capillaries. Postcapillary hypertension is characterized by venous medial hypertrophy and intimal proliferation with marked prominence of the venous internal elastic lamina (Frazier et al. 2000). All forms of pulmonary hypertension are associated with progressive dyspnea, which in advanced disease may be severe and associated with cyanosis. Clinical manifestations of right heart failure include peripheral edema, elevated jugular venous pressure, hepatomegaly, and ascites. PPH is relatively rare. Its existence as a separate entity has on occasion been queried by those who suggest that it may result from clinically latent microemboli (Shinnick et al. 1974 a, b). Nevertheless, the following appear to justify its recognition: It shows a familial incidence and primarily affects young to middle-aged adults with a 3–5:1 female to male ratio. Acetylcholine infusion has been shown to reduce the pulmonary arterial pressure (Fishman and Pietra 1980). In the 1960s, clusters of cases were reported in Germany, Austria, and Switzerland; this was subsequently attributed to use of the appetite suppressant Menocil (Fig. 7.1). Evidence suggests that endothelial injury to small pulmonary arteries and arterioles with resulting vasoconstriction may act as an inciting mechanism for PPH (Frazier et al. 2000). Clinical features include dyspnea, chest pain, syncope, cyanosis, and right ventricular (RV) failure. Electrocardiographic (ECG) changes in advanced disease are those of cor pulmonale. The pulmonary circulation is a low-pressure system. This results in part from the high compliance of the pulmonary vessels. An increase in pressure is associated with a radiologically appreciable increase in vessel caliber (Fig. 7.2). The frontal chest radiograph shows central pulmonary artery dilatation. Apparent prominence of the pulmonary segment of the left heart contour results from vascular dilatation and from a degree of cardiac rotation associated with right ventricular hypertrophy. Chronically elevated pulmonary arterial pressure leads to right ventricular overload. Initial adaptation is with ventricular muscular hypertrophy, but eventually the right ventricle becomes dilated and right ventricular failure supervenes. On the lateral view, right ventricular dilatation may be associated with narrowing or obliteration of the retrosternal space. Pulmonary vascularity is variable. Fig. 7.1 Primary pulmonary hypertension in a patient who had used appetite suppressants. Fig. 7.2 Correlation of pulmonary arterial pressure with the diameter of the right lower lobe pulmonary artery (from Meschan: Analyse der Röntgenbilder, vol. II. Stuttgart: Enke; 1981). CT demonstrates central pulmonary artery dilatation (Figs. 7.3a, 7.4a). The diameter of the main pulmonary artery is measured at the level of the bifurcation perpendicular to the long axis of the vessel (Naidich et al. 1999). A diameter of > 29 mm demonstrates a sensitivity of 87% and specificity of 89% for prediction of pulmonary hypertension. When a main pulmonary artery diameter of > 29 mm is associated with an elevated segmental arterial/ bronchial ratio (i. e., > 1) in three of four lobes, the specificity for pulmonary hypertension increases to 100% (Fig. 7.3b) (Tan et al. 1998). A main pulmonary artery to ascending aortic diameter ratio of > 1 also has a strong correlation with pulmonary hypertension (PH) particularly in patients who are less than 50 years of age (Ng et al. 1999). There may be dilatation of right heart chambers and paradoxical bowing of the interventricular septum towards the left ventricle may be seen in severe PH (Fig. 7.3c, and see Fig. 7.17b). High-resolution images through the lungs in severe pulmonary hypertension sometimes show small centrilobular nodules that may reflect the presence of cholesterol granulomata (Nolan et al. 1999, Fig. 7.4b, c). Fig. 7.3a-c Pulmonary hypertension: Axial CT image shows dilatation of the main pulmonary artery (a). Arterial-bronchial diameter ratio is increased in the right lower lobe (b). There is marked dilatation of the right heart chambers (c). Subcutaneous edema and ascites are consistent with right ventricular decompensation (cor pulmonale). Fig. 7.4a-e Primary pulmonary hypertension. CT shows dilated main pulmonary artery (a). CT images at lung windows show no evidence of mosaic perfusion but some small nodular areas of ground-glass density are seen perhaps reflecting cholesterol granulomata (b, c). Ventilation/perfusion scintigraphy shows no evidence of unmatched filling defects (d, e). MRI shows features of pulmonary hypertension including central pulmonary artery dilatation, right heart chamber dilatation, and paradoxical bowing of the interventricular septum. Abnormal intravascular signal related to slow flow within pulmonary arteries may be seen on ECG-gated spin echo sequences. Velocity-encoded gradient echo sequences provide a two-dimensional velocity map of a cross-sectional area of a vessel and allow calculation of aortic and pulmonary artery flow as well as flow volumes to the right and left lungs. The role of combined magnetic resonance (MR) perfusion and magnetic resonance angiography (MRA) has recently been evaluated by Nikolaou et al. who report a sensitivity of 90% for this technique in differentiating patients with PPH from those with chronic thromboembolic disease (Nikolaou et al. 2005). Ventilation-perfusion scintigraphy is characteristically normal or of low probability in PPH (Fig. 7.4d, e). Right heart catheterization reveals elevated pulmonary vascular resistance with normal capillary wedge and left atrial pressures. Pulmonary angiography shows dilated central vessels and a diffuse pattern of abruptly tapering and pruned subsegmental vessels (Frazier et al. 2000). Pulmonary thromboembolism may be found in up to 65% of autopsies, making it the most common pathologic finding in hospitalized patients. However, pulmonary emboli remain clinically silent in up to 80% of cases. An embolus within a pulmonary artery results in either a reduction or a cessation in distal perfusion. Collateral flow from the bronchial arterial system is usually sufficient to maintain lung viability. Pulmonary infarction develops in 10 to 15% of cases usually when there is associated pulmonary venous hypertension. It results from local hypoxia leading to capillary damage, exudation, hemorrhage, and coagulation necrosis. Macroscopic examination of the hemorrhagic infarct shows a firm, airless, livid dark-red segment of lung. Pulmonary infarcts are revascularized gradually from the periphery. Subsequent organization of smaller infarcts leads to complete resolution or contracted scar formation. Pulmonary infarcts very occasionally may become infected leading to abscess formation. Clinical diagnosis of acute pulmonary embolism may be difficult as the classic triad of sudden onset of chest pain, dyspnea, and hemoptysis is present in only a minority of cases. Hypoxia may be found on arterial blood gas analysis. Studies have reported both a high sensitivity and negative predictive value of D-dimer assay in investigation of acute PE in ambulant patients (Hogg et al. 2006, Hlavac et al. 2005). This test is less reliable in immobile hospitalized and pregnant patients. It is estimated that 1–5% of patients with acute PE progress to CTEPH (Frazier et al. 2000). The incidence of CTEPH is higher in females and lupus anticoagulant and anticardiolipin antibody may be positive. The chest radiograph in acute PE may be normal or findings may be nonspecific, even in severely symptomatic patients (Fig. 7.5). The posterobasal segments are sites of predilection for pulmonary thromboembolism because of the relatively high proportion of pulmonary blood flow which they receive. Conversely, only 10% of emboli involve the upper lobes. Features of acute pulmonary embolism without infarction include:
Pulmonary Hypertension
Precapillary Causes
Postcapillary Causes
Pathology
Clinical Features
Precapillary Pulmonary Hypertension
Primary Pulmonary Hypertension
Radiologic Findings
Computed Tomography
Magnetic Resonance Imaging
Ventilation-Perfusion Scintigraphy (VQS)
Pulmonary Angiography/Right Heart Catheterization
Acute Pulmonary Embolism (PE) and Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
Pathology
Clinical Features
Radiologic Findings
Chest Radiograph
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree