Fig. 17.1
Normal testis. Sagittal (a) and transverse (b) views of normal testes demonstrating homogeneous parenchyma. The markers take measurements of testicular size in both dimensions. Spectral Doppler tracing of a normal testis measured from a vessel noted in color Doppler (c). The mediastinum testis is seen as a hyperechoic stripe in the mid-testis (d)
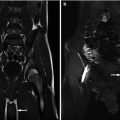
Normal testes are homogeneous in appearance on MR imaging. There is intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images relative to skeletal muscle (Fig. 17.2). The epididymis is similar to testicular parenchyma on T1-weighted images, but low signal intensity on T2-weighted images. The tunica albuginea is low signal intensity on both T1- and T2-weighted images. The mediastinum testis will be a low-signal band posterior in the testicle on T2-weighted images. Normal testis parenchyma is homogenous in attenuation and enhancement on CT examinations. CT is not typically used to image testicle pathology, but rather to image the chest, abdomen, and pelvis for testicular cancer staging.


Fig. 17.2
Normal testis. MR images demonstrating the normal testes from a young teen imaged for osteomyelitis of the hip. The T1 images (a) demonstrate the hypointense testes in the scrotum. The T2 image (b) demonstrates the hyperintense ovoid structures in the scrotum. The size discrepancy reflects their position within the scrotum
Acute Scrotum
The acute scrotum provides a unique radiological dilemma as interpretation of ultrasound findings relies on the clinical history. A detorsion event may present with similar findings as an epididymitis or epididymal torsion. This underscores the importance of obtaining a good history and maintaining open communication between the radiologist and the clinician.
Testicular Torsion
Testicular torsion is the single most common emergency within the realm of pediatric urology. Torsion can occur at any age but is most common in 12–18-year-old adolescents. Recovery of the testicle is most likely within the first 6 h after the event, after which testicular salvage rates drop precipitously. The etiology in the adolescent population is due to a bell-clapper deformity in which the tunica vaginalis encircles the epididymis, distal spermatic cord, and the testis rather than attaching to the posterolateral aspect of the testis. The deformity leaves the testis free to swing and rotate within the tunica vaginalis, as a clapper inside a bell.
The diagnosis of testicular torsion is primarily reliant on the clinical presentation. A typical history is a sudden onset of extreme and unremitting testicular pain that may or may not be associated with physical activity. Clinically, the patient is in severe pain, has difficulty ambulating, and may experience nausea and vomiting. The testicle is tender and in an abnormal transverse, high-riding lie, while the scrotum is erythematous. The cremasteric reflex is typically absent on the affected side and the Prehn’s maneuver is negative, i.e., there is no pain relief with elevation of the testicle. Attempts at scoring systems have been made but are not yet widely used [13].
Ultrasonography has been shown as highly reliable in diagnosis of the acute scrotum in the emergency department, with a sensitivity of 94 %, specificity of 96 %, and accuracy of 95.5 % [2]. Radiographically, the appearance of the testicle changes according to the degree of torsion and the time since the onset of the event. In complete torsion (540–720° twisting), the testis may have normal echotexture with absent blood flow very early in the process. After 4–6 h, the testis is enlarged, the parenchyma may appear normal or have some patchy hypoechoic areas present, and the blood flow is still absent (Fig. 17.3). Additional findings include enlargement of the epididymis, thickening of the scrotal skin, as well as the presence of a reactive hydrocele. Sonographic examination of the cord may demonstrate a whirlpool sign, representing the twisted congested vessels of the cord [14]. Kalfa et al. determined that sonography of the spermatic cord is highly sensitive and specific for the diagnosis of acute torsion [15]. Decreased blood flow may be seen with a partial torsion of 180–360°, where there is a longer window of viability to the testicle.


Fig. 17.3
Left testicular torsion for 5 h. Transverse images of the scrotum demonstrate the absence of flow and enlargement consistent with engorgement and edema
Torsion longer than 24 h may clinically present with diminished pain due to the presence of a completely infarcted and unsalvageable testicle. Sonographically the testicle appears to have heterogeneous echotexture and absent blood flow, and it is surrounded by reactive hyperemia [16]. It may be enlarged in size and contain areas of decreased echogenicity (Fig. 17.4).


Fig. 17.4
Missed torsion. Sagittal view of the right testis on a 16-year-old male 18 h after the onset of testicular pain demonstrating heterogeneity of the parenchyma. Doppler flow was not demonstrable on the left. The left testis was normal
Flow velocity is evaluated by Doppler ultrasound. In the prepubertal patient, it may be challenging to detect blood flow. The addition of power Doppler increases blood flow detection rate from 80 to 90 % in that age group. The velocity scale should be set to the lowest setting in order to increase the sensitivity to flow detection. Spectral Doppler sonography allows for comparison between the two testicles and findings of asymmetry in blood flow. The diagnostic accuracy of ultrasound is equivalent to that of nuclear scanning; however, the two modalities may be complementary in cases of uncertain diagnosis.
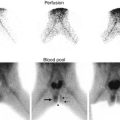
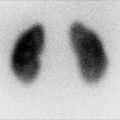
Scintigraphy and sonography show similar high sensitivity for the diagnosis of testicular torsion; however, in equivocal cases these modalities can complement one another to further increase the diagnostic accuracy [17, 18] (Fig. 17.5). In a multi-institutional review of 130 pediatric patients with acute scrotal pain, Baker et al. demonstrated 89 % sensitivity and 99 % specificity for color Doppler ultrasonography for differentiating testicular torsion from other nonsurgical etiologies. The mean age at the time of ultrasonography was 11 years. Seventeen patients were suspected to have testicular torsion and were emergently explored. The remainder of outcomes was obtained by clinical follow-up with outpatient sonograms. The mean length of follow-up was 1.3 years, but 23 % of patients were lost to follow-up and could not be evaluated. There were two cases of missed testicular torsion which resulted in delayed testis atrophy and one case that underwent surgical exploration for a torsed epididymal appendage [17].


Fig. 17.5
Nuclear scintigraphy of two boys with acute onset of testicular pain. (a) There is a paucity of uptake of tracer in the right hemiscrotum after pain of 5 h duration (arrow). (b) There is absence of flow but surrounding hyperemia (arrows) on the right hemiscrotum after 24 h of pain consistent with a missed torsion
These limitations were addressed by Lam et al. in a large single institution review of 626 patients who presented with acute scrotal pain. Forty-seven percent were explored immediately, leaving 332 (53 %) who underwent initial color Doppler US at time of presentation. Mean age was 8 years, and all patients had at least 2 weeks follow-up. Nine patients showed no flow on color Doppler US, and all were confirmed as testicular torsion upon exploration. Four of 323 patients who were found to have normal or increased flow on sonogram and explored based on clinical suspicion were found to have testicular torsion. Overall, color Doppler US yielded nine true-positive results and 319 true-negative results out of 332 which computes to a sensitivity of 69 %, specificity of 100 %, and an accuracy of 98.8 % [18].
Other authors have demonstrated better sensitivity for Doppler US in older patients. Yagil et al. report their results using Doppler US as a screening tool in the ED for triage of patients with acute scrotum. The patients studied were slightly older than in prior series, with a mean age of 16 years. In this review of over 620 patients, testicular torsion was suspected by Doppler US in 20 patients and confirmed via surgical exploration in 18. There were two false positives and one false negative. The reported study sensitivity, specificity, and accuracy were 94, 96, and 95.5 %. The only false-negative exam occurred in a 3-year-old boy who had present, but slightly diminished flow in the affected testicle. Surgical exploration due to a high index of clinical suspicion revealed torsion. This outstanding diagnostic accuracy may be due in part to an older study population which may have improved the performance of Doppler US in detecting arterial flow [19].
Other authors have noted that Doppler US is often user dependent and that documenting flow in the prepubertal testis can be unreliable [20–23]. An oft-quoted report by Ingram et al. showed that in 50 normal boys ranging in age from 2 months to 13 years, blood flow could be detected by color Doppler in both testes in only 58 % of boys and 34 % had no detectable flow [21]. Albrecht et al. report similar abilities of color and power Doppler to detect testicular blood flow in normal prepubertal boys (69 % vs. 65 %), with the combination of the two marginally better at 79 % [20]. This was confirmed in a prospective comparison by Blask et al. of scintigraphy and Doppler ultrasonography in 46 children who presented with an acute scrotum in which flow was demonstrated in the asymptomatic testis in only 60 % [24].
Appendix Testis/Epididymis Torsion
Torsion of an appendix is most common in 6–12-year-old patients. The clinical presentation is acute onset of pain, limited to the superior pole of the testicle at the level of the appendix. The occasional finding of a blue dot seen through the scrotal skin is due to ischemia and necrosis of the appendage. Sonographically the epididymis and sometimes the entire testicle are inflamed, and on occasion the enlarged and avascular appendix can be seen and palpated due to swelling and hyperemia. Treatment is symptomatic relief with nonsteroidal anti-inflammatory agents and scrotal elevation.
Epididymitis/Orchitis
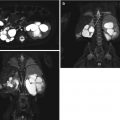
These entities are common causes of an acute scrotum in the pediatric population. The onset is more gradual than that of testicular or appendix torsion, and it may be accompanied by fevers. In prepubertal patients the cause is usually nonbacterial and may be related to dysfunctional voiding. In the postpubescent patient this is usually related to retrograde spread of infection or to chemical irritation of the epididymis secondary to reflux of urine. In sexually active patients, this may be associated with the spread of a sexually transmitted disease. Sonographically, the epididymis and/or testis appear hyperemic and hypervascular, enlarged, and hypoechoic (Fig. 17.6). Reactive hydroceles and scrotal edema are also common findings. Nuclear perfusion scintigraphy studies using technetium 99 rely on flow images showing abnormal increased testicular perfusion, as well as static pictures showing a “cold” defect in the area of hydrocele (Fig. 17.6). Inflammatory conditions are characterized by diffusely increased uptake of radiotracer into the affected testicle. A study by Mueller et al. found that when supplementing scintigraphy with sonography, the interpretation was changed in 14 % of cases, which spared 31 % of patients from a surgical procedure [18].


Fig. 17.6
Ultrasound (a) and nuclear scintigraphy (b) demonstrating the features of epididymo-orchitis. Increased Doppler flow is noted on ultrasound to both the testicle and epididymis when compared to the asymptomatic side. There is increased uptake of nuclear tracer to the left hemiscrotum (arrow)
Trauma
The main objective of a sonographic evaluation is to assess whether there is presence of blood flow to the testicle and to identify whether the tunica albuginea surrounding the testicle is intact, as absence of flow or the presence of testicular rupture are indications for scrotal exploration. Indeterminate findings or high clinical suspicion is also an indication for exploration.
In testicular rupture there is extrusion of seminiferous tubules out of the testicle, and the tunica appears discontinuous. Salvage rate of testicular rupture is upwards of 90 % even after 72 h posttrauma. Buckley and McAninch reported that the finding of heterogeneous parenchyma and irregular contour had 100 % sensitivity and 93.5 % specificity for the diagnosis of testicular rupture [19] (Fig. 17.7).


Fig. 17.7
Trauma. Transverse view of the right testis demonstrating several hematomas within the testis, a surrounding hematocele and thickening of the overlying skin following blunt trauma (a). The same testis several weeks later demonstrating an isolated remnant hypoechoic area and a large hydrocele (b)
Contusions can be seen as a hypoechoic area, but are not indications for scrotal exploration if the tunica albuginea is intact. A testicular fracture is a break in the parenchyma of the testis without a tear in the tunica albuginea. It will appear as a linear hypoechoic band and may be managed nonoperatively if there are no abnormalities in Doppler flow imaging.
Hematomas may occur anywhere within the scrotum following trauma. Acute injury is represented by a hyperechoic dense fluid collection whereas an older bleed will be hypoechoic and without vascularity. The fluid collection of a hematoma is usually complex and heterogeneous.
Hematoceles are complex fluid collections that separate the visceral and parietal layers of the tunica vaginalis. In the acute setting they appear hyperechoic and become hypoechoic with time [20].
Pyocele/Abscess
Pyoceles are rare in the pediatric population [21]. Its presence is suggested by the clinical history, which usually includes prior surgery or a scrotal or perineal skin infection. Acute pain, fevers, and an elevated white blood cell count are present. The physical findings may include a tender and swollen scrotum, erythema, edema, and a tense hydrocele, which may be confused with an acute torsion of the testicle. An abscess may be suggested radiographically by the presence of complex multiloculated scrotal fluid collection containing debris, thickened tunica vaginalis, and heterogeneous echogenic areas. Color Doppler will demonstrate peripheral hypervascularity without internal blood flow [22]; however, blood flow to the testicle should appear preserved.
Vasculitis
Systemic processes such as Henoch-Schonlein purpura (HSP) may affect the testicle in approximately 15 % of cases. In some patients, scrotal symptoms are the initial clinical manifestation of this disease process. The patient with HSP usually has cutaneous symptoms such as lower extremity petechiae, as well as renal and rheumatologic symptoms. The scrotum is painful and enlarged [23]. Ultrasound examination will reveal enlarged epididymis and thickened scrotal skin, as well as reactive hydroceles. Testicular blood flow is usually maintained or increased (Fig. 17.8). Nuclear scintigraphy is also diagnostic in such cases for epididymo-orchitis, which demonstrate increased perfusion to the testis [23, 24].


Fig. 17.8
Vasculitis. An 8-year-old boy presented with scrotal pain and a papular rash on the legs. While the diagnosis of Henoch-Schonlein purpura was made, concurrent testicular torsion could not be excluded by history and physical examination. The constellation of ultrasound findings of thickened scrotal skin (bracket-star) maintained or increased color Doppler flow, and the presence of a hydrocele (H) is all consistent with the diagnosis of HSP
Hydrocele/Hernia
The processus vaginalis is an extension of the parietal peritoneum, which envelops the testicle in two layers as it descends into the scrotum during embryogenesis. The processus vaginalis is normally obliterated in the 7–9 months of gestation, but in approximately 20 % of males the processus vaginalis is patent at birth, resulting in a potential space. In most cases this will resolve by 1 year of age, and many males with a patent processus vaginalis are asymptomatic. Sonographically, the two layers of the tunica vaginalis can appear as isoechoic to hyperechoic linear bands extending from the internal inguinal ring to the scrotum. Pediatric hydroceles are commonly due to an indirect hernia, which is a consequence of a patent processus vaginalis that allows for free communication of peritoneal fluid with the scrotum, and fluid accumulation. Those hydroceles are reducible, and the scrotal sac contents are seen to change in size throughout the day and with different activities. In the noncommunicating variant, the hydrocele sac size is fixed, as it is not in communication with the peritoneal fluid [25]. Hernias may not communicate with the tunica vaginalis, and the fluid may be able to be tracked distally from the groin and seen to end proximal to the testis (Fig. 17.9).


Fig. 17.9
Hydrocele. Anechoic space is seen in the right hemiscrotum that surrounds the testis. The superior margin of this collection was noted
Hydroceles are usually diagnosed clinically, and imaging is not indicated. If imaging is obtained for inconclusive cases, the hernia is sonographically represented by hypoechoic fluid collection within the tunica vaginalis, and the scrotal hydrocele is the peritoneal fluid surrounding the testicle (Fig. 17.10). In the pediatric population these are usually simple fluid collections without septations unless there is a history of infection or trauma. Herniation of bowel via a patent processus vaginalis is more common in the premature infant, in which the inguinal canal is very short as the internal and external rings are almost overlying each other at birth, and the patency of the processus vaginalis is large relative to the abdominal contents. In cases of suspected bowel incarceration, plain radiographs can be use to augment ultrasound findings by detecting bowel gas in the scrotum. Echogenic bowel mucosa or bowel motility can be detected sonographically [26].


Fig. 17.10
Hernia. Sagittal view of an ultrasound performed in a 6-year-old boy with an inguinal swelling. A longitudinal hypoechoic area (H) is noted in the inguinal area superior to the testis (T). This was consistent with a left inguinal hernia which was confirmed at surgery
Hydrocele of the spermatic cord may present as an inguinal swelling, with or without pain (Fig. 17.11). It is a rare finding, present is about 1–5 % of cases with inguinal symptoms. Similar to the scrotal hydrocele, the spermatic cord hydrocele emanates from a patent processus vaginalis. This finding may have several variants: the encysted hydrocele, the reducible or funicular hydrocele, and the mixed variety. The encysted hydrocele does not communicate with the peritoneal cavity and therefore cannot be reduced. The funicular hydrocele appears as a peritoneal diverticulum into the inguinal canal that terminates above the scrotum. Occasionally there may be multiple cysts along the spermatic cord, which may appear as beads along the spermatic cord when studied sonographically [25]. In a study assessing the utility of scrotal ultrasound in the diagnosis of a hydrocele of the cord, 3,486 sonograms in 1,743 pediatric patients were reviewed. All patients presented with a mass or swelling of the inguinal region. Of those, 27 patients were diagnosed sonographically with a hydrocele of the cord after finding of an anechoic, avascular mass along the spermatic cord. Only one of these patients was clinically diagnosed with this entity, reflecting the lack of awareness of this diagnosis as well as its rarity [27, 28].


Fig. 17.11
Hydrocele of the spermatic cord. Sagittal view of the inguinal canal in a child who felt a “lump” in the inguinal canal. This area was limited to the spermatic cord on physical examination. The hypoechoic area (H) was well defined with normal cord superior and inferior to this area. Bladder (UB)
Varicocele
Dilated testicular veins are found in 10–13 % of adolescents and are more common on the left side. Isolated right varicocele or one that does not decompress in the supine position should prompt a workup of an abdominal or pelvic pathology. The association of varicoceles with testicular failure and with infertility is well established; however, the mechanism by which unilateral varicoceles have this bilateral effect remains controversial. This pathology is usually treated in adolescents when hypotrophy of the affected testicle is greater than 20 % as compared to the contralateral testicle. Varicoceles are rarely associated with pain or discomfort, and if severe they may be visible and deform the scrotum. Grade 1 is palpated only on Valsalva; grade 2 is easily palpable, but not visible; grade 3 is visible.
Sonographic evaluation of a varicocele is done both in the supine and standing positions, while performing Valsalva maneuvers. On ultrasound the varicocele appears as an anechoic serpiginous vein greater than 3 mm at rest and retrograde flow with increased vein diameter on Valsalva maneuver (Fig. 17.12). Grading of varicocele depends on sonographic evaluation. Grade 0, subclinical varicocele, is found only on sonogram, but not clinically detectable. High flow rates (>38 cm/s) were strongly associated with testicular volume asymmetry [29].