Coronal reconstruction contrast-enhanced CT scan through the abdomen.
Renal Cell Carcinoma Metastasis to Posterior Fossa
Primary Diagnosis
Renal cell carcinoma metastasis to posterior fossa
Differential Diagnoses
Hemangioblastoma
Arteriovenous malformation
Highly vascular glioblastoma
Imaging Findings
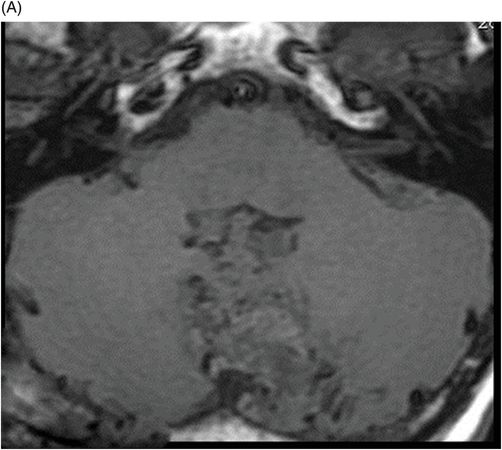
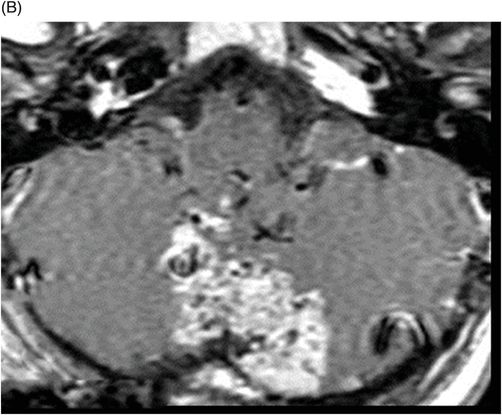
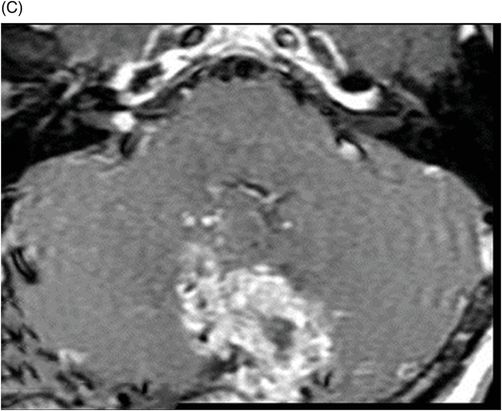
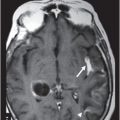
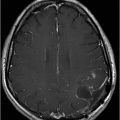
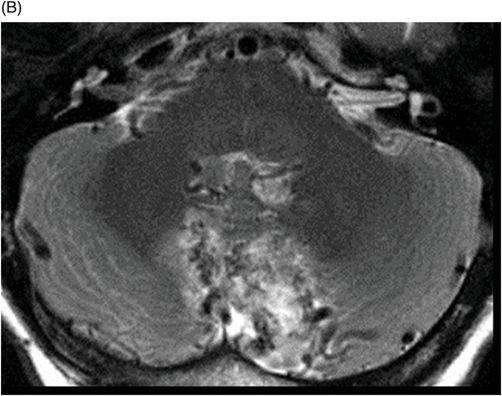
Fig. 107.1: (A) Axial FLAIR and (B) Axial T2W images showed a mixed signal intensity, intra-axial, and lobulated lesion with a predominantly hyperintense signal, relative to the cerebellar white matter. Prominent flow voids in and around the lesion were noted with no significant peritumoral edema. (C) Axial DWI showed no restricted diffusion. Fig. 107.2: (A) Axial T1WI showed mixed signal intensity lesion with associated flow voids. (B) Axial T1WI postgadolinium showed intense contrast enhancement of the lesion with a central non-enhancing area, suggestive of necrosis. (C) Axial T1WI also showing a small enhancement nodule inside the right internal auditory canal. Fig. 107.3: (A–C) Sagittal contrast-enhanced T1WI of the cervical, thoracic, and lumbar spines with fat suppression showed multiple intradural extramedullary enhancing nodular lesions, compatible with drop metastases. Fig. 107.4: Coronal reconstruction, contrast-enhanced CT scan of the abdomen showed a large heterogeneously enhancing mass at the upper pole of the left kidney, compatible with renal cell carcinoma.
Discussion
Imaging findings demonstrating a vascular, posterior fossa mass with flow voids, which lacks a cystic component, in the absence of diffusion restriction, in a patient with known renal cell carcinoma are suggestive of renal cell cancer metastases.
Hemangioblastomas (HGBLs) are the second most common infratentorial parenchymal mass in adults (after metastases) and 25–40% of cases of HGBL occur in association with von Hippel-Lindau syndrome. Although HGBLs often demonstrate presence of multiple lesions on imaging, they are more common in a younger age group. A vascular tumor may be purely cystic, or a purely solid, large cyst with a mural nodule (most common pattern, seen in 60% of cases), or solid mass with internal cysts. Symptoms are non-specific and the most common presenting complaint is headache.
The typical imaging finding of a HGBL is an intra-axial cystic mass with an intensely enhancing mural nodule (with the cystic component larger, compared to the solid nodule) that demonstrates flow voids from vascular structure and abuts the pia. Although presence of a nodule abutting the pia is considered a classic imaging finding of HGBL, this finding is also present in other tumors as well. The cystic component of an HGBL lesion does not usually enhance, owing to its high protein fluid component, and may demonstrate associated presence of hemorrhage. Generally, if hemorrhage is associated with the cystic component, the lesion appears hyperintense in comparison to CSF on T1-weighted MR sequences. The solid component is isodense on CT, isointense on T1-weighted sequence, and hyperintense on T2-weighted sequence, with or without associated internal flow voids on MR images.
Glioblastoma subtypes can occur in adults and generally appear as an irregular, ring-enhancing mass; however, they rarely develop in the posterior fossa.
Arteriovenous malformations (AVMs) are much more common supratentorial lesions than infratentorial. They can appear as iso- to hyperdense serpentine vessels with or without associated calcification on CT and typically present with a bag of worms (tangle of serpentine flow voids) that corresponds to the nidus, associated with arterial feeders and draining veins, better demonstrated in postcontrast, angiographic studies. Hemorrhage and gliosis in the brain parenchyma around the lesion is also found in AVM images. In summary, they can have similar imaging findings as seen in our case, especially because of the marked contrast enhancement of the lesion and the prominent flow voids previously described. However, unlike the imaging seen in our case, AVMs typically show minimal or no mass effect and do not show necrosis.
Although 85% of metastatic lesions are supratentorial, metastases are still the most common intra-axial neoplasm of the adult posterior fossa. Up to 30% of all intracranial metastases occur in the posterior fossa. Usually they present as multiple lesions, but in the posterior fossa, there is a high incidence of solitary lesions (25–50%), which typically occur near the brain surface at the corticomedullary junction. The primary site of origin for metastases most commonly includes the lungs, breast, gastrointestinal sites, melanoma, and rarely genitourinary, as in our case.
At imaging, metastatic intra-axial lesions usually present as round and well-circumscribed lesions with a large area of peritumoral cerebral edema, although edema may be absent in small cortical lesions. On MR, most metastases are iso- to hypointense on T1-weighted images. However, they can demonstrate T1 hyperintensity if hemorrhage has occurred, or if the lesion has high melanin content. Frequently, metastatic lesions appear hyperintense on T2-weighted images, but may appear iso- to hypointense as well. Metastases can be solitary and very large with a necrotic central portion, as in our case, and can be very small and numerous. The pattern of contrast enhancement can be homogeneous, nodular, inhomogeneous, or ring-like.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree