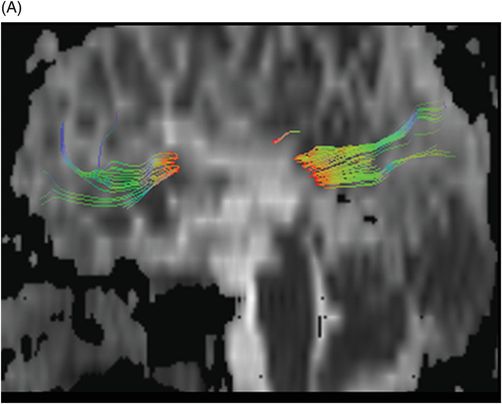
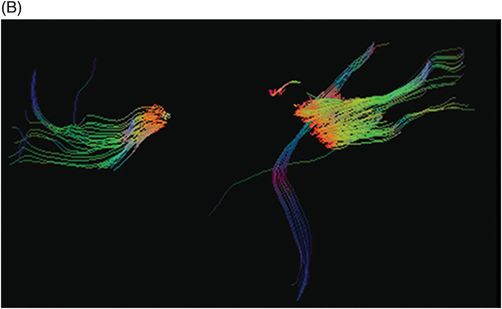
(A) Sagittal tractography and (B) Sagittal fiber-tracking images through the level of the corpus callosum.
Hereditary Spastic Paraplegia with Hypoplastic Corpus Callosum
Primary Diagnosis
Hereditary spastic paraplegia with hypoplastic corpus callosum
Differential Diagnoses
Other types of hereditary spastic paraplegia
Amyotrophic lateral sclerosis
Primary lateral sclerosis
Levodopa-responsive dystonia
Adrenomyeloneuropathy
Imaging Findings
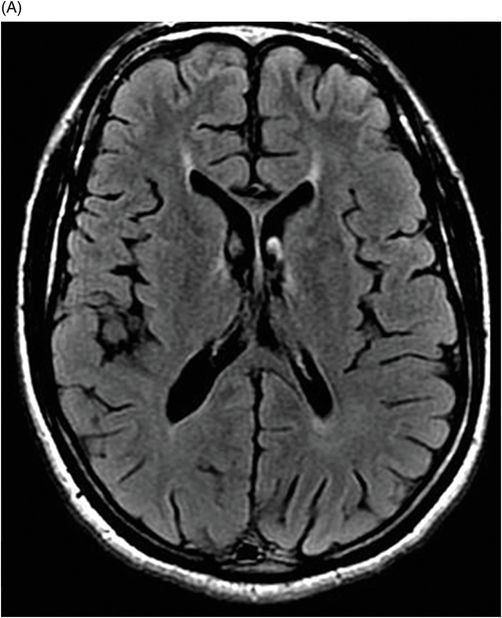
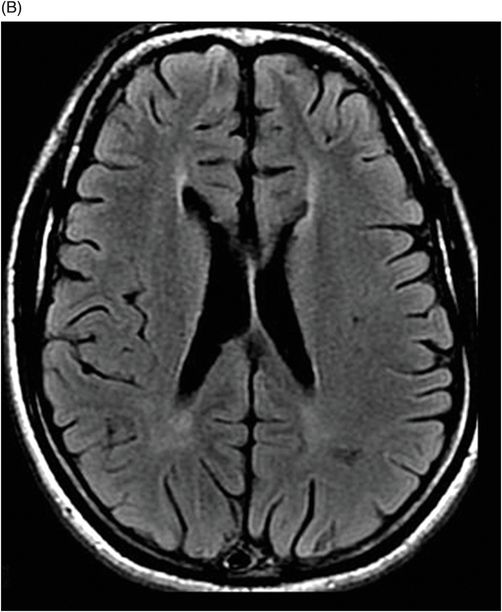
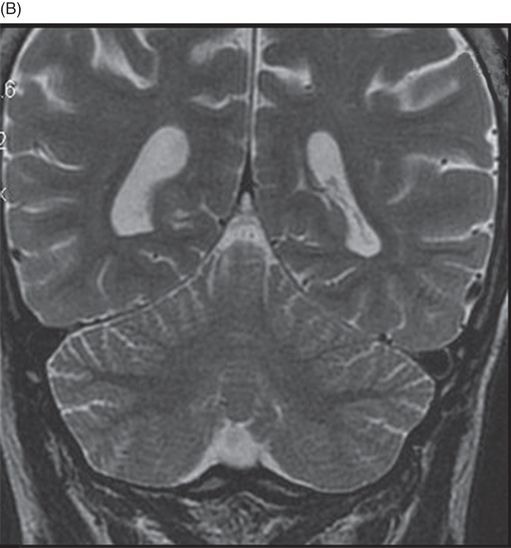
Fig. 118.1: (A) Sagittal T1WI through the midline showed significant thinning of the corpus callosum. (B) Coronal T2WI through the level of the cerebellar hemispheres revealed absence of cerebellar atrophy. Fig. 118.2: (A–B) Axial FLAIR images through the level of the lateral ventricles revealed mild ventricular enlargement and linear hyperintensity in the white matter adjacent to the frontal horns of the lateral ventricles (ear of the lynx sign). Fig. 118.3: (A–B) Sagittal T2WI through the midline of the cervical and thoracic spine confirmed absence of any lesions in the spinal cord. Fig. 118.4: (A) Sagittal tractography through the midline demonstrated significant changes including mean diffusion increase and fractional anisotropy reduction in the corpus callosum. (B) Diffusion tensor imaging fiber tractography through the level of the corpus callosum demonstrated marked reduction of the white matter fibers (tracts) in the central part of the corpus callosum.
Discussion
In our patient, adult symptom onset eliminates all pediatric onset spastic paraplegias. Prominent imaging findings demonstrating corpus callosum atrophy are the key to diagnosing this rare form of autosomal recessive hereditary spastic paraplegia (HSP).
Motor neuron diseases such as amyotrophic lateral sclerosis (ALS) and primary lateral sclerosis (PLS) can have similar presentations and may be extremely difficult to differentiate from HSP. In fact, motor neuron disease and HSP may be considered as components of a single disease spectrum. Imaging studies from patients with ALS demonstrate specific, typical imaging features that are similar to levodopa-responsive dystonia, which may present with similar clinical features. However, although these pathologies share imaging features, none of these demonstrates atrophy of the corpus callosum. Adrenomyeloneuropathy typically demonstrates spinal cord atrophy on imaging, which was not present in this case.
Hereditary spastic paraplegias comprise a genetically and clinically heterogeneous group of neurodegenerative disorders. Characterized by progressive spasticity and lower limb hyperreflexia, this family of disorders is classified as pure/uncomplicated (non-syndromic) or complicated (syndromic) based on their clinical variability. Fifty-six different genetic mutations have been described in the SPG gene (spastic paraplegia), the genetic loci responsible for HSP, that can be transmitted as autosomal dominant, autosomal recessive, or X-linked patterns of inheritance.
Hereditary spastic paraplegia with hypoplastic corpus callosum (HSP-HCC) is a rare, complicated form of HSP. It is transmitted in an autosomal recessive manner and mainly described in the Japanese population. In this form, a patient who exhibited normal motor and mental development as a young child usually presents in the second decade of life with cognitive impairment, sensory disturbances, and ataxia. It has been genetically linked to mutation of the spastin protein encoded by the SPG11 locus 15q13–15, although there is heterogeneity. However, HSP-HCC has also been described in patients without this locus mutation. Thus, the exact mechanism of mutation-based development of HSP-HCC is not known.
Magnetic resonance imaging findings in patients diagnosed with HSP-HCC include presence of a thin corpus callosum that predominantly involves the anterior aspect of the body and the knee of the corpus callosum. Although not a specific finding, it is distinctive. Other associated imaging findings include frontoparietal atrophy and enlargement of lateral ventricles, reduced size of thalamus, and symmetric white matter lesions. A thin corpus callosum is not specific to this syndrome and whether it represents a congenital hypoplasia or a progressive atrophy remains unknown. The symmetric periventricular white matter lesions adjacent to the frontal horn of the lateral ventricles give a flame or ear of the lynx appearance on axial FLAIR images.
The diagnostic criteria of autosomal recessive HSP with a thin corpus callosum include onset of a slowly progressive spastic paraparesis, autosomal recessive inheritance pattern, cognitive impairment, thinning of the corpus callosum revealed by CT/MR imaging, and the exclusion of other disorders by laboratory tests and MR images of the spine and brain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree