Sagittal T1WI of the brain
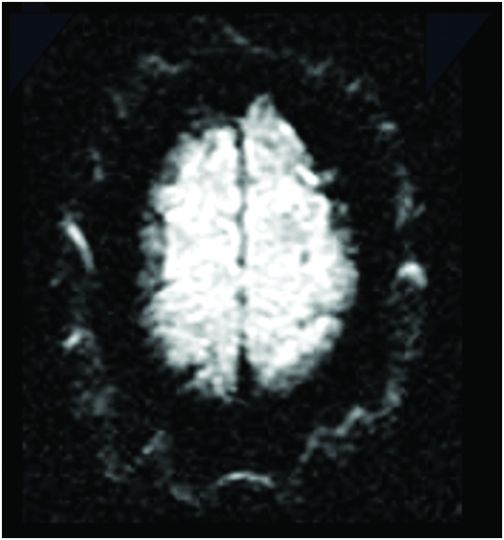
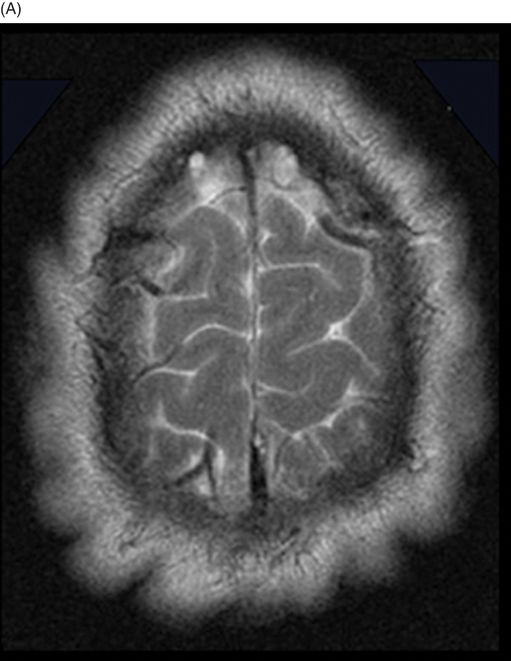
Axial DWI of the brain at the level of frontoparietal convexities.
Cutis Verticis Gyrata
Primary Diagnosis
Cutis verticis gyrata
Differential Diagnoses
Associated cutis verticis gyrata entities include:
myxedema, leukemia, acanthosis nigricans, amyloidosis diabetes mellitus, syphilis, tuberous sclerosis, and acromegaly
Additional pathologic entities associated with cutis verticis gyrata include:
Ehlers-Danlos, Noonan, Turner, and fragile X syndromes
Imaging Findings
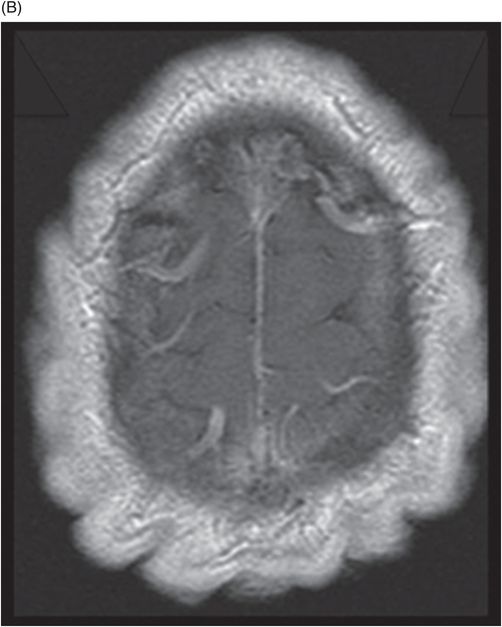
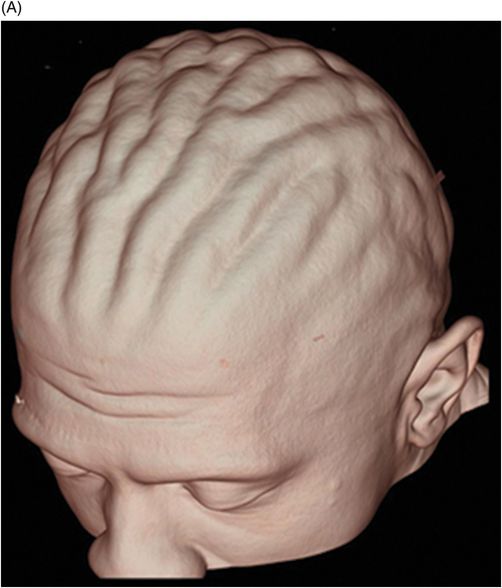
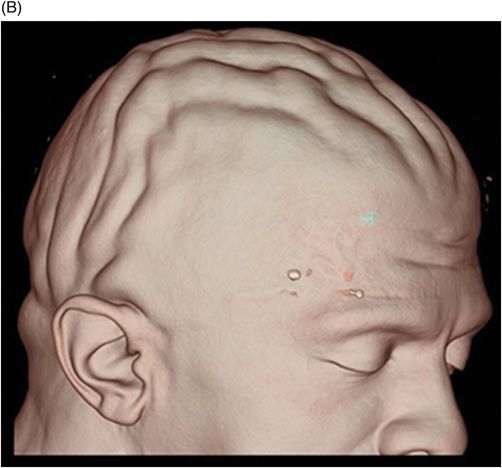
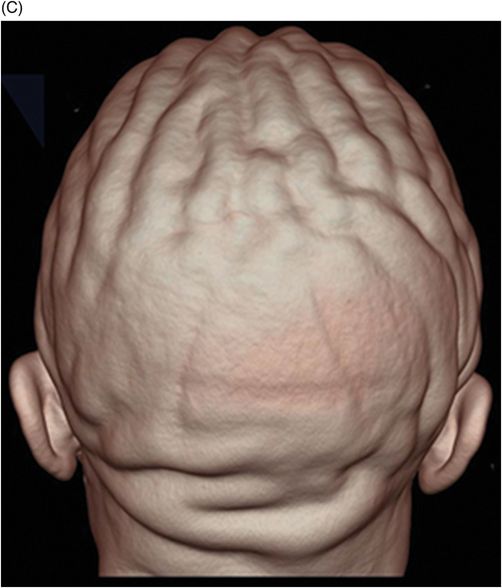
Fig. 135.1: Sagittal T1WI showed diffuse thickening of the scalp soft tissues. Fig. 135.2: (A) Axial T2WI and (B) Postcontrast T1WI also showed thickening of the scalp. Thickening of the underlying subcutaneous fat was noted. Fig. 135.3: Diffusion weighted imaging appeared normal. Fig. 135.4: (A–C) Three-dimensional surface rendering MRI demonstrates anteroposterior orientation of the furrows and ridges.
Discussion
Cutis verticis gyrata (CVG) is a term used to describe a rare scalp disorder identified by excessive thickening of the soft tissues of the scalp and characterized by ridges and furrows, which give the scalp a cerebriform appearance. Clinically, the ridges are hard and cannot be flattened on applying pressure. First described in 1837 by Jean-Louis-Marc Alibert, CVG has been called paquidermia verticis gyrata, cutis verticis plicata, and bulldog scalp syndrome. The term cutis verticis gyrata was proposed by Unna in 1907. It was later categorized into primary and secondary forms by Polan E. Butterworth in 1953.
The primary type of this condition often occurs after puberty and is demonstrated by the appearance of symmetric ridges in the scalp. The primary type is further classified to essential and non-essential forms. The essential form of primary CVG is usually solitary and is not associated with any additional pathology. On the other hand, the non-essential form is usually associated with neurologic abnormalities, which include microcephaly, mental retardation, strabismus, retinitis pigmentosa, and blindness in some cases. The primary type of CVG is often seen in males. The secondary type of CVG can occur at any age, and unlike the primary type, features an asymmetric ridge pattern. The secondary type is associated with dermatologic diseases such as eczema, psoriasis, and impetigo, as well as systemic diseases such as amyloidosis, acromegaly, leukemia, type II diabetes mellitus, and tuberous sclerosis. Anabolic steroid use is a common cause of the secondary form.
The secondary form has been associated with acromegaly, pachydermoperiostosis, pituitary tumors, amyloidosis, myxedema, intracerebral aneurysm, dermatofibroma, cerebriform intradermal nevus, acne conglobata, cutaneous focal mucinosis, acanthosis nigricans, and syphilis. Several syndromic associations are noted with the secondary form of CVG especially Ehlers-Danlos syndrome, Beare-Stevenson syndrome, Noonan syndrome, Michelin tire baby syndrome, fragile X syndrome, and Turner syndrome.
The diagnosis of CVG is primarily based on clinical examination and can be incidentally diagnosed when patients are undergoing head CT or MR imaging. Multiplanar imaging depicts the symmetric or asymmetric ridges and the furrows of the scalp depending on the type of the CVG. The ridges and furrows will be oriented in an anterior‑posterior pattern and will extend to involve the occipital regions obliquely. The coronal plane is best to evaluate the longitudinal ridges, while the sagittal plane is best to evaluate the transverse ridges. Magnetic resonance imaging also aids in the better assessment of the scalp layers compared to CT. High-resolution MR imaging can help in evaluating the scalp layers, especially the dermis and epidermis, subcutaneous fat, and the galeal/subgaleal/periosteum complex. The scalp thickening is attributed to hyperplasia of fat and connective tissue in the subcutaneous tissue layer, with or without dermal layer abnormalities. Three-dimensional MRI with surface rendering technique is an excellent tool to demonstrate and assess the symmetry and orientation of the thickened scalp folds.
Treatment in most cases is aimed at maintaining hygiene to avoid associative unpleasant odor. Plastic surgery is usually performed for cosmetic purposes with excision and healthy skin grafting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree