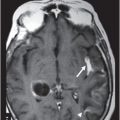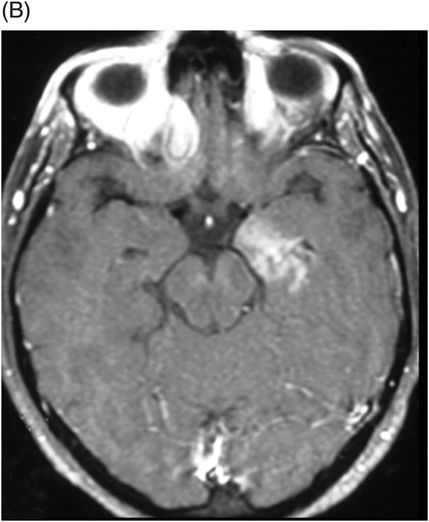
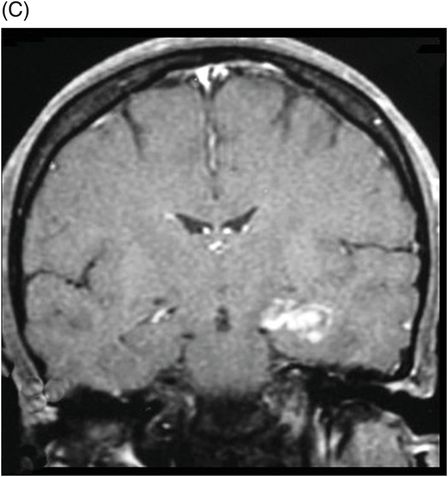
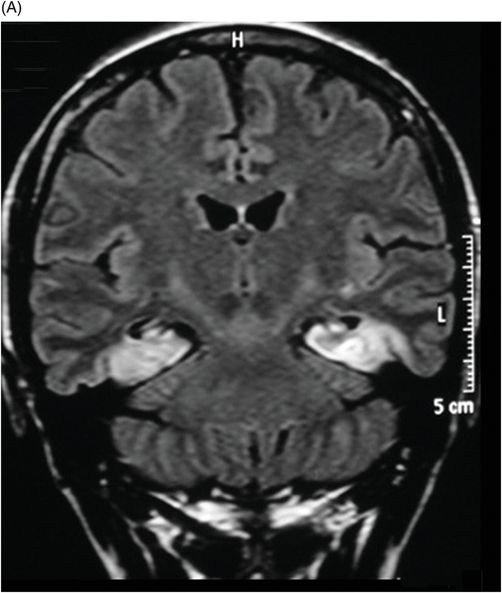
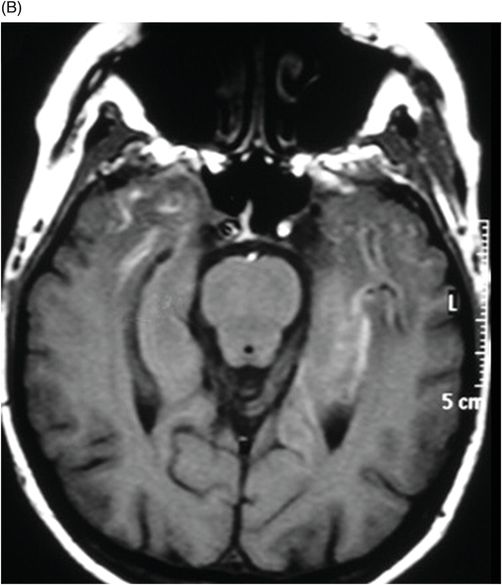
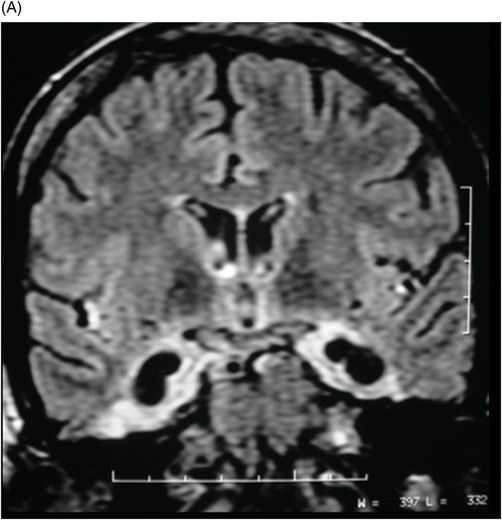
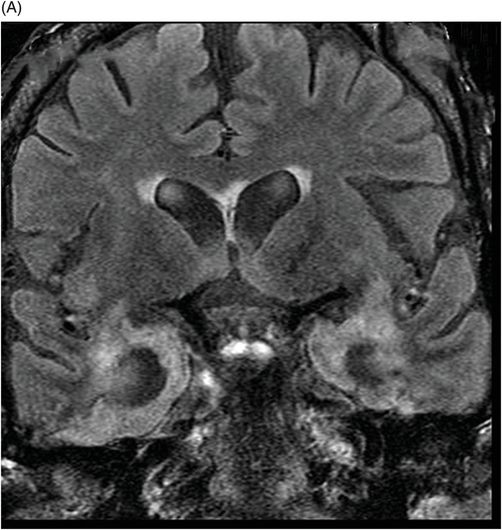
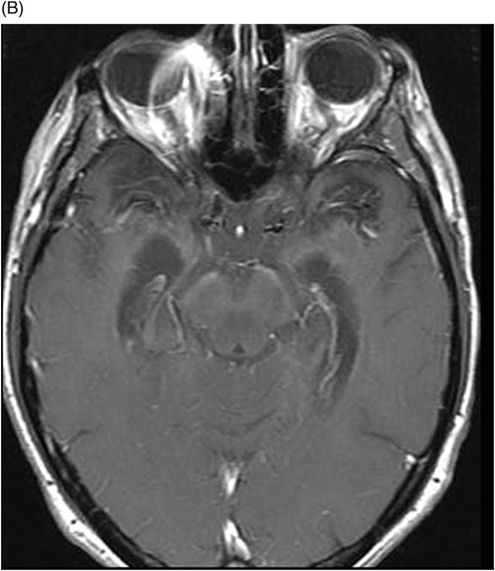
(A) Coronal FLAIR, (B) Axial T1WI MR postcontrast, and (C) Coronal T1WI postcontrast through the temporal lobes (10-day follow-up).
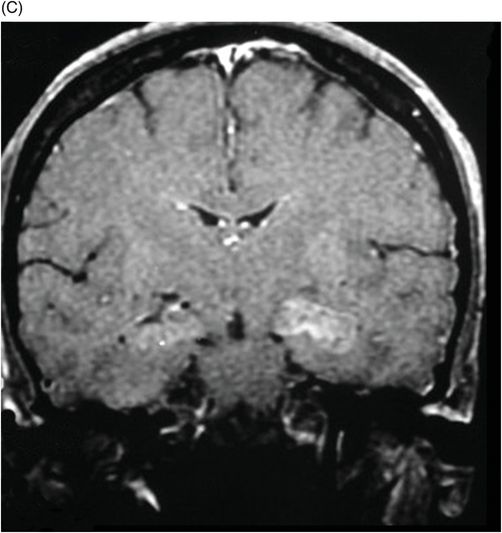
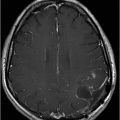
(A) Coronal FLAIR and (B) Axial T1WI postcontrast through the temporal lobes (2-month follow-up).
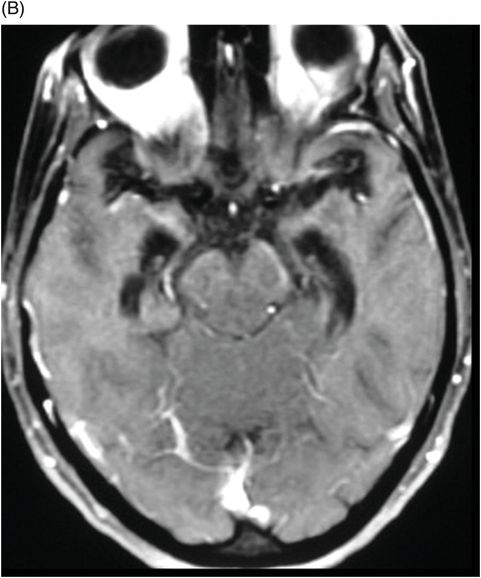
(A) Coronal FLAIR and (B) Axial T1WI postcontrast through the temporal lobes (5-month follow-up).
Anti-N-Methyl-D-Aspartate Receptor (NMDAR) Encephalitis
Primary Diagnosis
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis
Differential Diagnoses
Cerebrovascular event
Metastatic disease
Subacute or chronic inflammatory disorders
Imaging Findings
Fig. 52.1: (A) Coronal FLAIR images through the level of the hippocampus demonstrated swelling and hyperintense signal of the left hippocampus associated with hyperintense signal of the right hippocampus. (B) Contrast-enhanced axial T1WI and (C) Coronal T1WI postcontrast showed abnormal enhancement of the left hippocampus. Fig. 52.2: (A) Coronal FLAIR, (B) Axial, and (C) Coronal T1 postgadolinium images (10-day follow-up) showed consistent left hippocampus findings, demonstrating swelling and hyperintense signal of the right hippocampus.
Fig. 52.3: (A) Coronal FLAIR, and (B) Axial T1WI postgadolinium images (two-month follow-up) showed hippocampal atrophy associated with hyperintensity signal on the mesial aspect of the temporal lobes. Fig. 52.4: (A) Coronal FLAIR, and (B) Axial contrast-enhanced T1WI demonstrated progression, with increased atrophy of the hippocampus (five-month follow-up).
Discussion
Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis usually presents with psychiatric symptoms, most frequently anxiety, agitation, and visual or auditory hallucinations. It is a newly identified paraneoplastic disorder targeting NR1 and NR2 subunits of NMDARs, causing severe neurologic and psychiatric symptoms. Neurologic features such as movement disorders, seizures, and cognitive problems are also characteristic findings. Literature findings indicate that most patients experience autonomic dysfunction and persistent cognitive deficits following disease onset, predominantly executive function, and memory impairments. Positive findings for antibodies to the NR1 subunit in sera and/or CSF confirmed the diagnosis.
Magnetic resonance imaging of the brain will be normal in 45% of patients. The other 55% may show non-specific T2 or FLAIR signal hyperintensity, most frequently at the hippocampus, as seen in our patient. Faint or transient contrast enhancement of the cerebral cortex, overlaying meninges, or basal ganglia may be seen, although not a predominant finding. Follow-up brain MR imaging either remains normal or shows minimal change. Magnetic resonance spectroscopy has not yet been documented to be of any proven diagnostic value.
In most patients, electroencephalograms are consistently abnormal; however, findings by Schmitt et al. indicate that 30% of affected individuals show an extreme delta brush pattern. Since this has not been described in other neurologic conditions, it may suggest that it is a unique finding in some patients with this disorder.
Although NMDAR encephalitis has been reported to be more common in females with ovarian teratoma, it has become increasingly clear that the syndrome is not restricted to adult females but can also be seen in adult males and children of either sex, in the absence of an associated systemic neoplasm. In those patients with tumor, surgical resection may resolve symptoms. For non-surgical candidates, first-line immunotherapy consisting of corticosteroids plus intravenous immunoglobulin (IVIG) or plasma exchange has been proposed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree