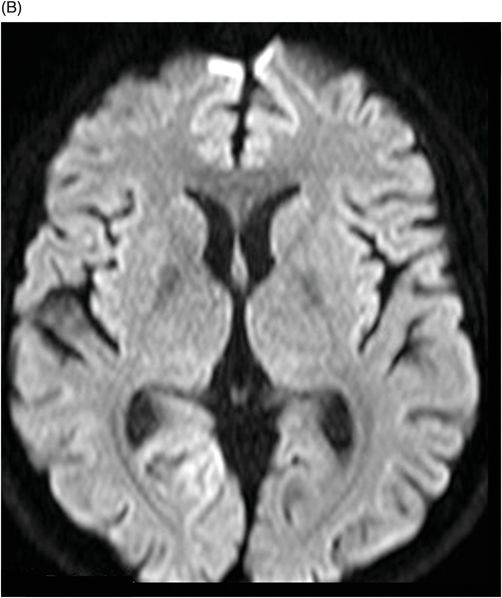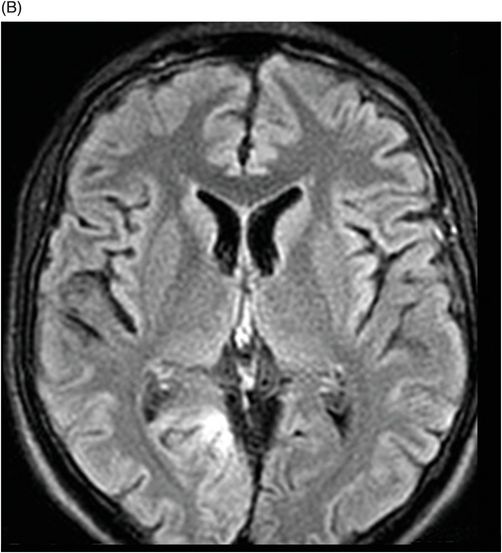
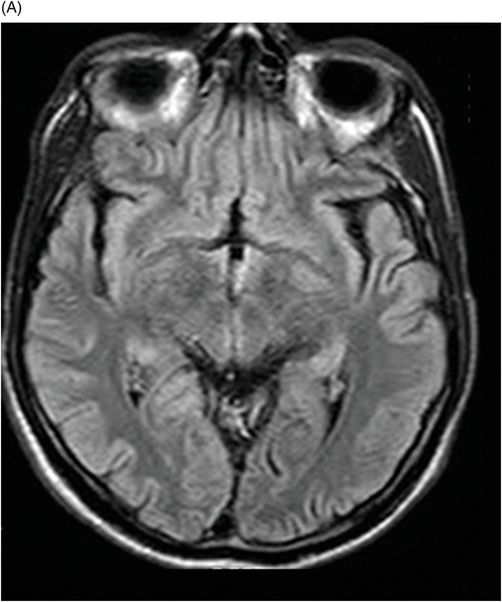
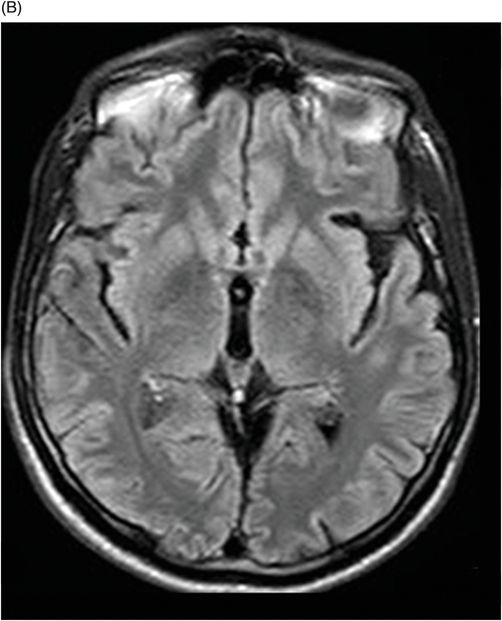
(A–B) Axial FLAIR through the level of the third ventricle.
Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-Like Episodes Syndrome: MELAS Syndrome
Primary Diagnosis
Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes syndrome: MELAS syndrome
Differential Diagnoses
Ischemic stroke
Herpes simplex encephalitis
Viral infection
Vasculitis (Moyamoya disease)
Kawasaki disease
Kearns-Sayre syndrome
Wilson disease
Status epilepticus
Imaging Findings
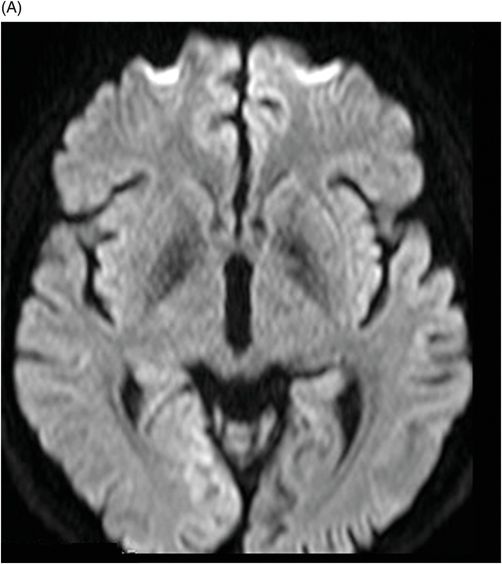
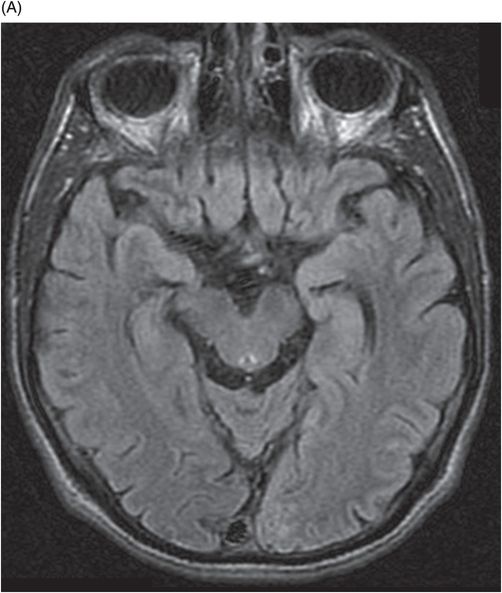
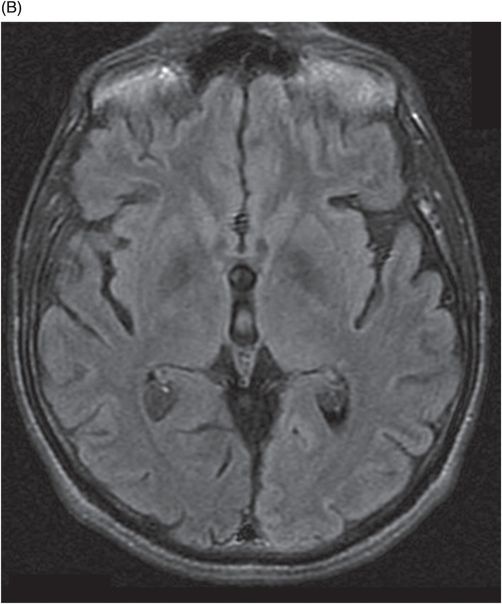
Fig. 74.1: (A–B) Axial FLAIR MR images showed signal abnormality involving cortical and subcortical right lingual gyrus. Fig. 74.2: (A–B) Diffusion-weighted MR images demonstrated a tenuous, hyperintense lesion in the right occipital lobe. Fig. 74.3: (A–B) Axial FLAIR demonstrated complete resolution of the signal abnormality involving the left lingual gyrus (1-week follow-up). Fig. 74.4: (A) Axial FLAIR demonstrated new hyperintensity lesion in the left occipital lobe (2-month follow-up). (B) Axial diffusion confirms the hyperintensity lesion in the left occipital lobe. Fig. 74.5: (A–B) Axial FLAIR showing complete resolution of the lesion (1 week later follow-up).
Discussion
The combination of mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes constitute MELAS syndrome. The constellation of clinical and radiologic findings seen in this patient case is typical of MELAS. MELAS syndrome is a hereditary metabolic disorder and one of the most common multisystem mitochondrial diseases with a special predilection for the nervous system and muscles.
Although the age at onset varies between 3 months and 40 years of age, in most cases the initial signs and symptoms occur before adulthood. Clinical symptoms originating from all organ systems have been described, but tissues with high-energy requirements, such as muscle and brain, are particularly vulnerable. In adults, muscle weakness, exercise intolerance, and ophthalmoplegia dominate, together with slowly progressive cognitive dysfunction. In children, the first manifestations usually belong to encephalomyopathies such as growth disturbance and epileptic seizures, with a progressive symptomatology. Learning disabilities, cognitive regression, exercise intolerance, and limb weakness are the most frequent disease manifestations.
The mitochondrial abnormality found in MELAS is due to point mutations of mitochondrial DNA. The most common mutation is an A>G transition at the tRNA Leu (UUR) 3243, which causes a defect in the mitochondrial protein synthesis, impairing adenosine triphosphate (ATP) production. Pavlakis et al. described the syndrome in 1984, after observing children who were usually normal at birth and during early infancy, but who were subsequently evaluated with delayed growth, episodic vomiting, seizures, and recurrent cerebral injuries resembling strokes.
The stroke-like events occur in almost all patients with MELAS and most frequently give rise to neurologic deficits such as hemiparesis, hemianopia, or cortical blindness. The proposed clinical diagnosis of MELAS is based on three major features: 1) occurrence of stroke-like episodes before 40 years of age; 2) presence of encephalopathy with seizures and/or dementia; and 3) the presence of lactic acidosis, ragged red muscle fibers as well as the presence of additional symptoms such as recurrent headaches and recurrent vomiting.
Clinical features that help distinguish MELAS syndrome from typical herpes simplex encephalitis (HSE) or other viral infection include the absence of fever, lack of prominent alteration in consciousness, and a normal CSF cell count.
Imaging findings have been reported as multiple stroke-like lesions, calcification of the basal ganglia, and diffuse atrophy. On standard MR images, the imaging hallmark of MELAS is the presence of infarct-like, often transient lesions that are not confined to the vascular territories but have a predilection to the posterior part of the cerebral hemispheres. Diffusion-weighted imaging can show variable results; however, during an acute stroke-like episode, ADC maps usually show low values, demonstrating cytotoxic edema. Since ADC values are higher in the non-affected areas than the controls, it can be inferred that MELAS involves the entire brain. Proton MR spectroscopy classically shows an increased lactate peak at 1.3 ppm, better seen at an intermediate echo time when it inverts, which can also be seen over the ventricles.
Invasive procedures may help to diagnose this condition including the quantification of the lactic acid in the serum and CSF, presence of ragged red fibers on muscle biopsy, and an increased number of mitochondria in endothelial cells of small cerebral arteries.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree