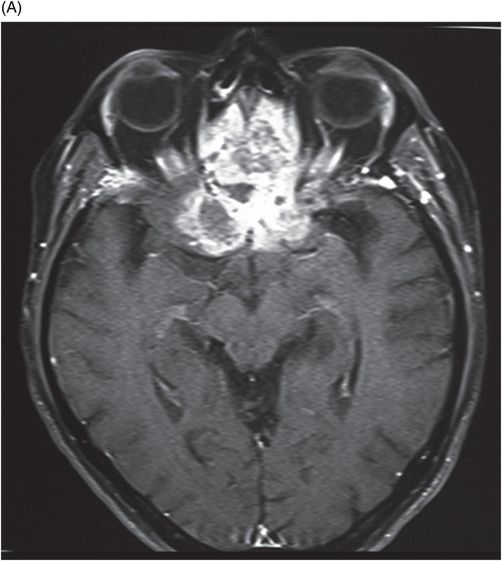
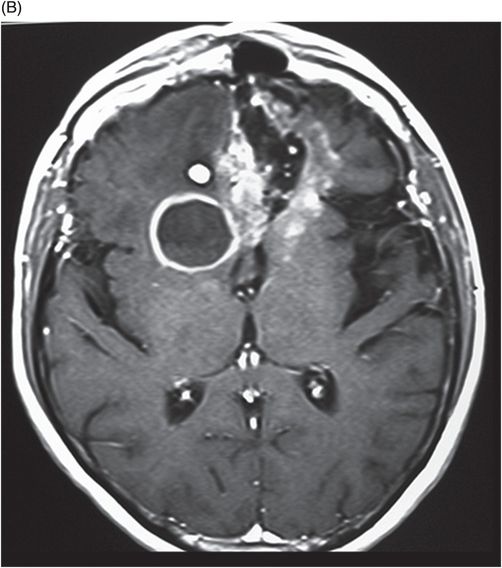
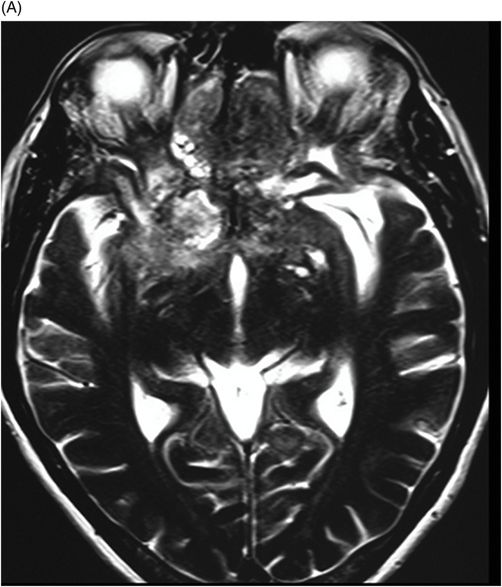
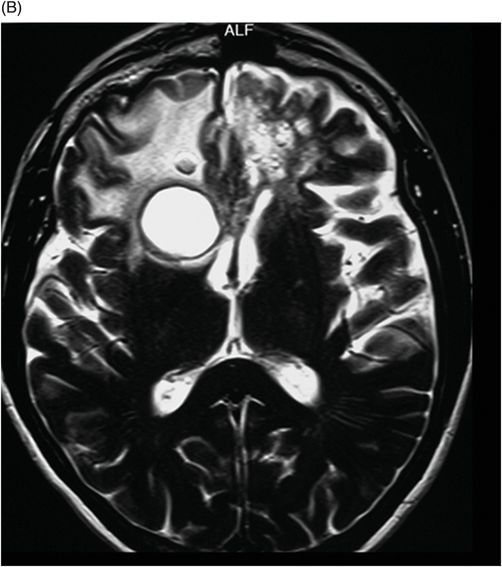
(A–B) Axial T2 through the level of the third and lateral ventricles.
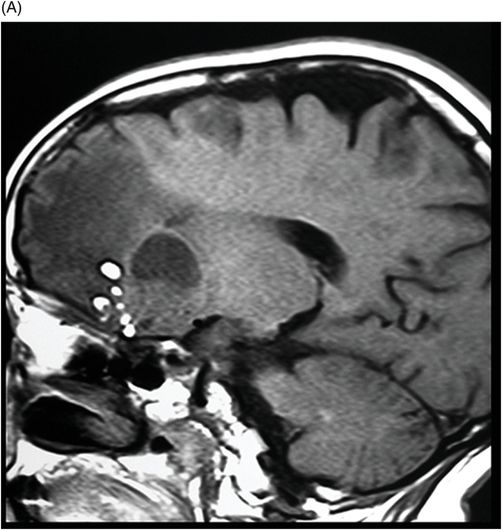
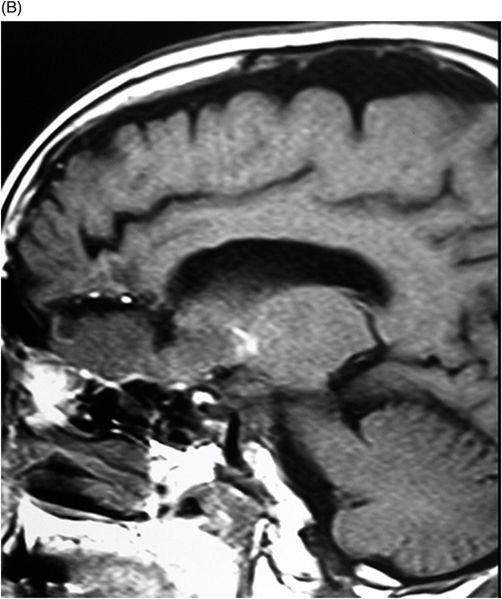
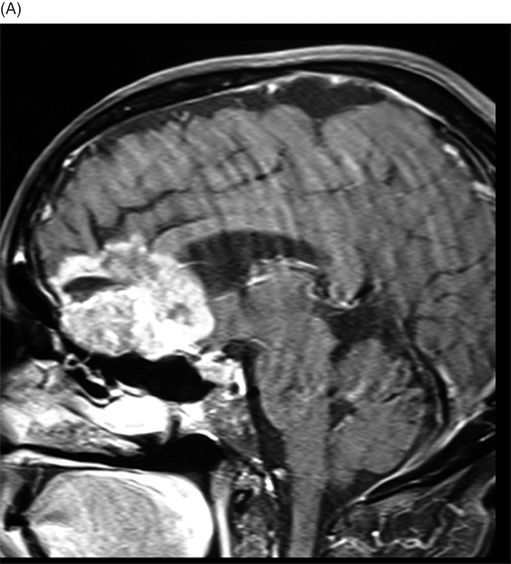
(A–B) Sagittal T1-weighted postcontrast fat-suppressed images through the midline and parasagittal.
Malignant Transformation of Dermoid Cyst
Primary Diagnosis
Malignant transformation of dermoid cyst
Differential Diagnoses
Lipoblastic meningioma
Liposarcoma
Imaging Findings
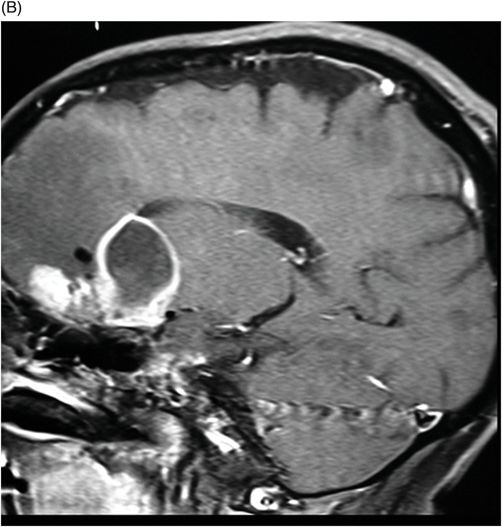
Fig. 89.1 (A) Sagittal T1WI and (B) Sagittal T1WI fat-suppression images showed a T1 hyperintense lesion in the midline of the skull base that suppressed on T1-weighted fat suppression, suggestive of dermoid cyst. Fig. 89.2 (A–B) Sagittal T1WI showed an expansive process centered in the skull base that invaded the basal surface of both frontal lobes, more importantly in the right side, with some foci of fat inside the lesion and vasogenic edema in the adjacent brain parenchyma. Fig. 89.3 (A–B) Axial T2 confirmed the extensive lesion in both frontal lobes, larger on the right side, with central hyperintense area in the center, surrounded by vasogenic edema. Fig. 89.4 (A–B) Axial T1WI postcontrast fat suppression showed an extensive and heterogeneous enhancing lesion in both basal frontal lobes that invaded the rostrum of corpus callosum, with central necrosis in the right side. Fig. 89.5 (A–B) Sagittal T1WI postcontrast fat suppression showed an extensive basal frontal lesion that invaded the frontal lobes, with central necrosis in the right side. Note the suppression of the foci on fat inside the lesion.
Discussion
The history of a known dermoid cyst, demonstrated on prior imaging and visible on current images, in the presence of an intratumoral fat signal is suggestive of malignant degeneration of the dermoid cyst. The presence of an abnormal T2 signal in the peritumoral bed in addition to significant lesion enhancement is typical of malignant transformation, as seen in this patient.
Intracranial dermoid cysts account for approximately 0.5% of brain tumors. They develop during the fourth or fifth week of fetal development from aberrant ectodermal embryonic tissue in the neural groove that typically contains mature squamous epithelium, keratin, and adnexal elements such as hair follicles and sebaceous glands. Dermoid cysts are usually extra-axial and occur near the midline (parasellar/frontobasal) and third and fourth ventricles. The suprasellar cistern is the most common site: other common locations for dermoid cysts include the posterior fossa and the anterior skull base/frontonasal region.
Imaging findings of lipoblastic meningioma, a WHO grade I tumor, can demonstrate intratumoral fat signal. However, intense enhancement and abnormal peritumoral T2 signal is uncommon in this tumor. The presence of fat signal is also seen in liposarcoma, but they are not known to develop in the central skull base-frontal lobe region.
Dermoid cysts can be complicated if they rupture (please see Part VI: Case 113), with consequential development of meningitis and hydrocephalus. Another extremely rare complication is malignant transformation of dermoid cyst into a squamous cell cancer. Although this is extremely rare, malignant transformation of a benign cyst is the third most common cause of intracranial squamous cell cancer, after metastasis and direct extension of the tumor. Epidermoid cysts, not dermoid cysts, more commonly degenerate into squamous cell cancer. The underlying etiology of the transformation is unknown; however, it is thought that persistent chronic inflammatory changes lead to the development of squamous cell cancer, which can be further complicated by leptomeningeal spread.
On CT images, dermoid cysts present as circumscribed, very-low-density (−20 to −140 HU) lesions, without any contrast enhancement. Calcification may be seen in up to 20% of cysts. They are associated with vasogenic edema and rarely cause hydrocephalus. As these tumors have adnexal elements including fat, they are hyperintense on T1WI as well as fast spin echo T2WI sequences. Typically, these tumors do not enhance with contrast.
Image-based diagnosis of malignant degeneration in dermoid cysts can be challenging. A sudden increase in size, development of nodular intratumoral enhancement, and development of new abnormal T2 signal in the peritumoral areas are some of the documented imaging findings of malignant degeneration. Once malignant degeneration occurs, there is a rapid change of the patient’s clinical course with an extremely poor prognosis. Surgical resection is the treatment of choice whenever possible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree