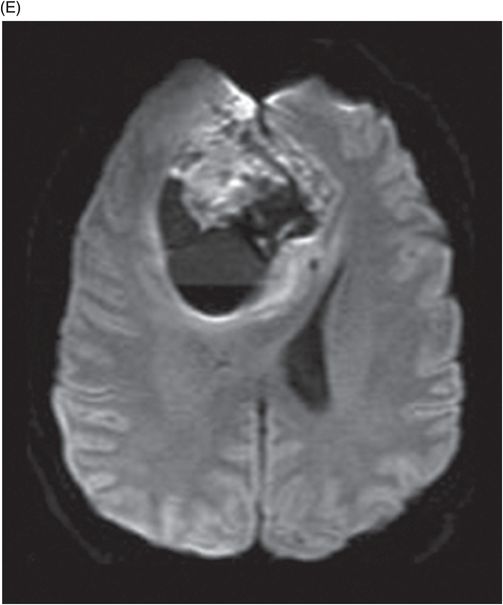
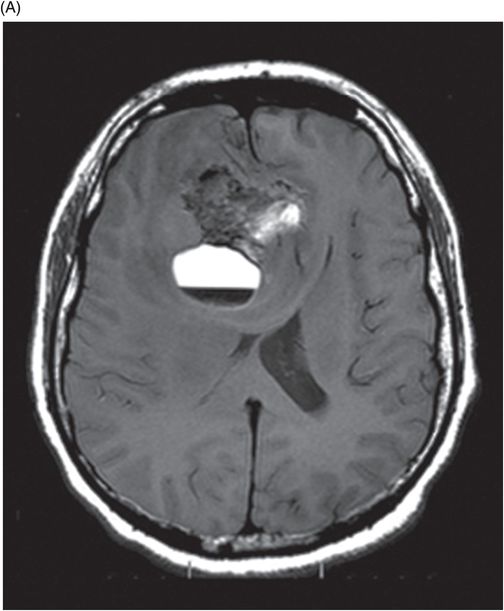
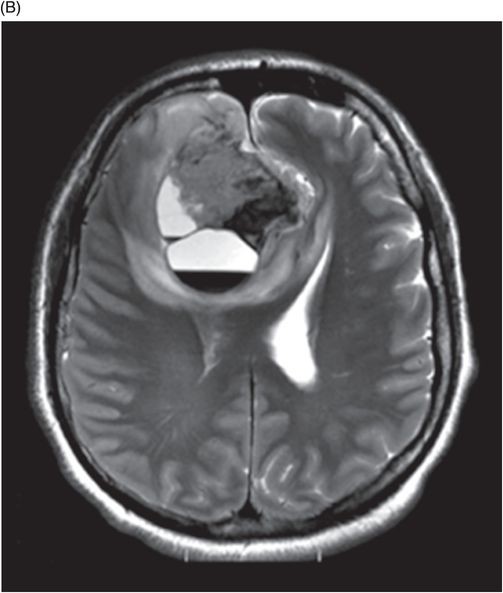
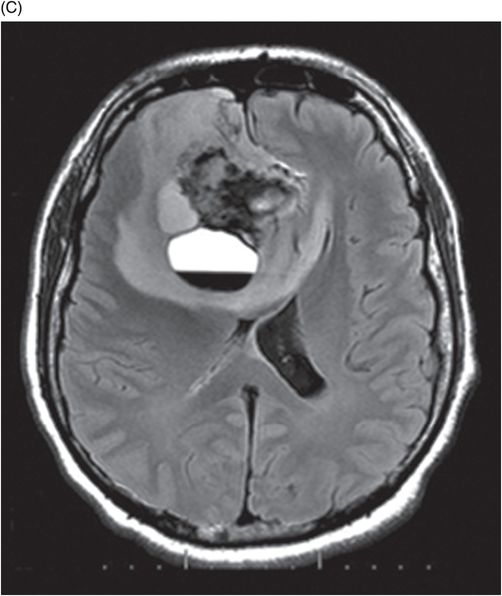
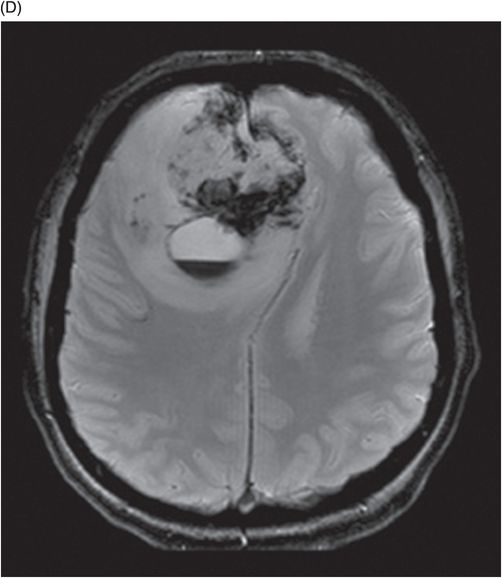
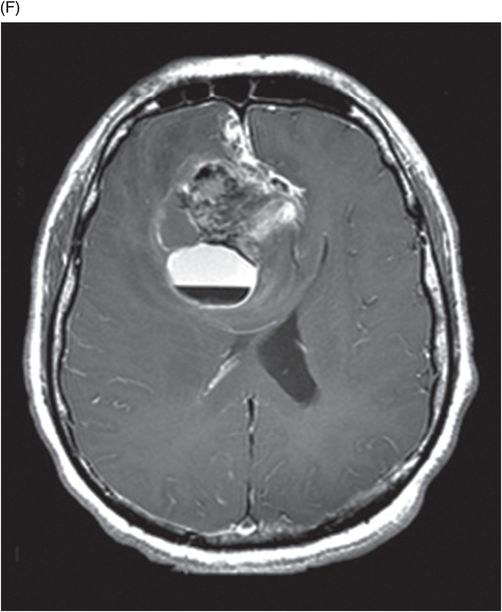
(A) Axial T1W, (B) Axial T2W, (C) Axial FLAIR, (D) Axial GRE, (E) Axial DWI, and (F) Axial postgadolinium T1W images at the level of lateral ventricles.
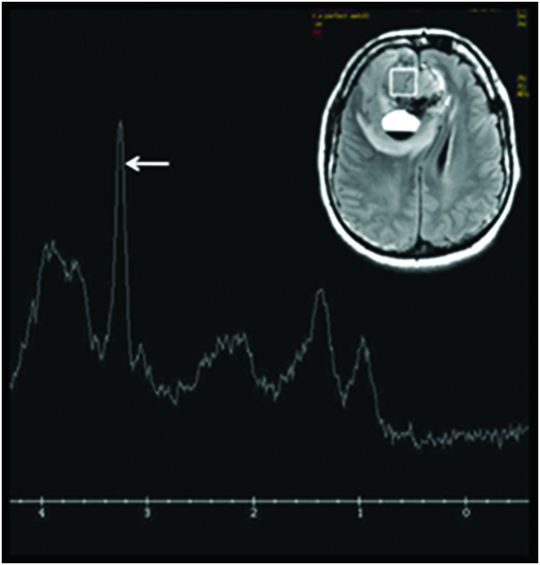
Single voxel MR spectroscopy through the solid component of the right frontal lobe mass lesion.
Extraventricular Neurocytoma
Primary Diagnoses
Extraventricular neurocytoma
Differential Diagnoses
Glioblastoma
Ependymoma
Oligodendroglioma
Ganglioglioma
Primitive neuroectodermal tumor
Hemorrhagic metastases
Imaging Findings
Fig. 90.1: Axial postcontrast CT image at the level of lateral ventricles showed a right frontal, parafalcine heterogeneously enhancing mass with moderate vasogenic edema and mass effect, with a focal cystic component that revealed a blood-fluid level. Fig. 90.2: (A) Axial pre-gadolinium T1W, (B) T2W, and (C) FLAIR images demonstrated a mixed signal intensity, cortical-based, right parafalcine frontal mass lesion with a cystic component that showed mixed hypo-isointense areas and a hyperintense blood-fluid level. (D) Axial GRE sequence depicted multiple foci of blooming/T2 shortening, representing areas of hemorrhage. (E) Axial DWI sequence showed minimal diffusion restriction in the solid component of the mass lesion. (F) Axial postgadolinium T1W image showed heterogeneous enhancement in the solid part of the lesion. Fig. 90.3: Single voxel MR spectroscopy at TE 135 showed elevated choline peak at 3.2 ppm (arrow).
Discussion
A predominantly cortical-based, heterogeneously enhancing, right frontal lobe mass/lesion with a cystic component containing blood-fluid levels, demonstrating mild to moderate associated perilesional edema and considerable mass effect is suggestive of an aggressive, high-grade tumor. For example, glioblastoma, ependymoma, or hemorrhagic metastasis may demonstrate similar imaging findings. However, the age of the patient, tumor location, and cystic component, in the presence of mild to moderate edema, is suggestive of an extraventricular neurocytoma. Radical tumor excision and histopathologic evaluation including immunohistochemical staining confirmed the diagnosis of extraventricular neurocytoma.
In contrast to neurocytomas, oligodendrogliomas are usually less well demarcated and tend to have larger, coarse calcification (seen in about 20–90%). Focal calvarial remodeling is also often noted. High-grade gliomas also have obscured and infiltrating margins, but calcification is very uncommon. Ependymomas are often seen adjacent to the ventricles with relatively mild edema; the parietal lobes are the favored sites for cystic ependymomas. Hemorrhagic metastatic lesions have similar imaging features. However, the presence of calcification and negative systemic imaging evaluation for a primary malignancy do not favor this diagnosis. The most favoured location for ganglioglioma is the temporal lobes. The cystic component is often central with a peripheral solid component; hemorrhage is an unusual feature of ganglioglioma. Occurrence of calcification in gangliogliomas has been estimated to occur in 25–28%. Primitive neuroectodermal tumor has a predilection for the frontoparietal lobes and is seen in the pediatric population (less than five years of age).
Extraventricular neurocytomas are rare parenchymal tumors that seem to exhibit neuronal differentiation, similar to central neurocytoma, occurring remote from the ventricular system but with wide variability. Owing to its variable presentation, the most recent WHO classification of CNS tumors (2007) categorizes extraventricular neurocytoma as a new entity. These tumors show wide inconsistency with regard to their morphologic features, cellularity, and proliferation rate. Thus, they pose a diagnostic challenge because of the significant imaging and histopathologic overlap noted among other brain tumors, especially oligodendroglioma.
Extraventricular neurocytomas are tumors of young adults and adolescents with no gender predilection. They can occur at a variety of locations but are most frequently seen in the cerebral hemispheres, especially in the frontoparietal regions, with usual manifestations of headache, seizure, and hemiparesis. Extraventricular neurocytomas are often large, well-demarcated, cortical-based lesions with hemorrhage, calcification, cystic necrosis, and intense enhancement, and should be included in the differential diagnoses for cerebral masses. Though a prospective diagnosis of this lesion is difficult, because of the rare incidence of this entity it should be considered, especially in a young individual. These masses can also be purely cystic, a cyst with a mural nodule, or purely solid. They closely resemble an oligodendroglioma, which are cortical-based tumors with calcification.
Histopathologic evaluation of extraventricular neurocytoma reveals uniform round cells with regular nuclei and a diagnostic immunohistochemical staining, which are strongly synatophysin positive (Syn) (+++); glial fibrillary acid protein negative (GFAP) (−); Vimetin (Vim) (−), S-100 (+++); and IDH1 gene mutation negative. It also appears that atypical histologic features correlate with aggressiveness and higher recurrence rates.
Surgery plays a central role for management of these tumors with favorable response seen in most patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree