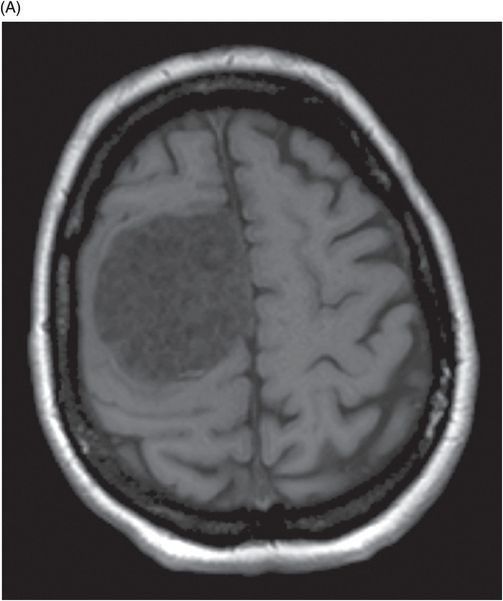
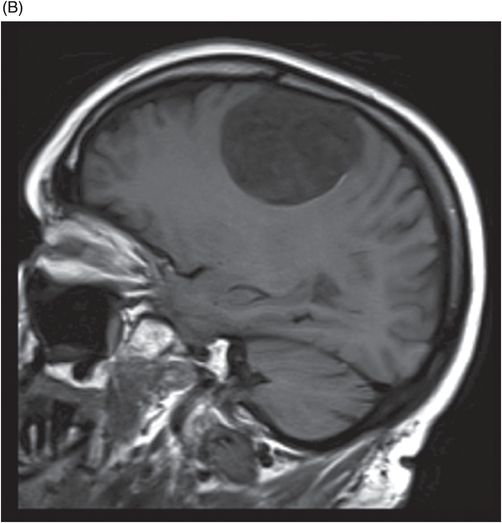
(A) Axial T1WI at the level of frontoparietal convexities and (B) Right parasagittal T1WI.
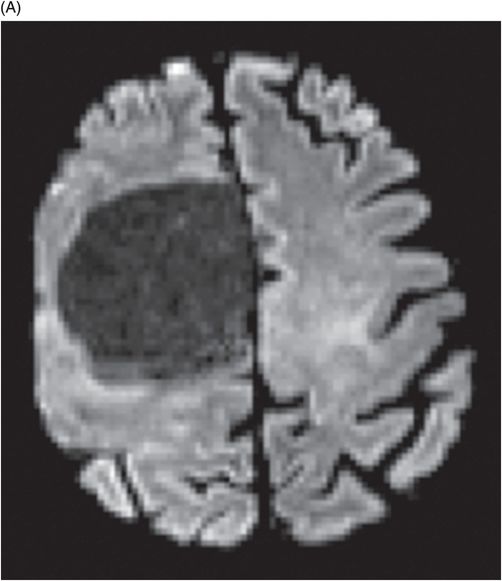
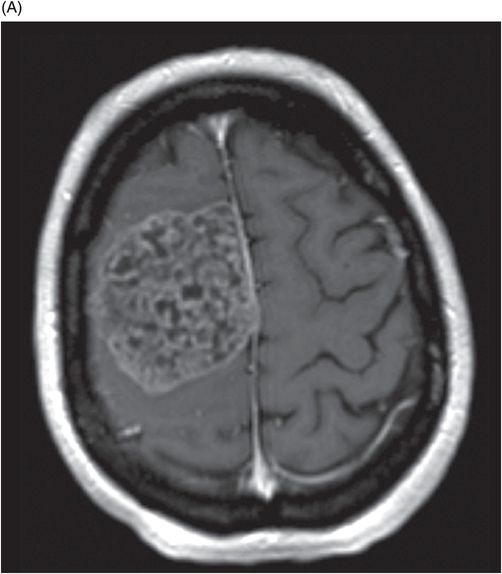
Axial T2WI at the level of frontoparietal convexities.
Axial FLAIR at the level of frontoparietal convexities.
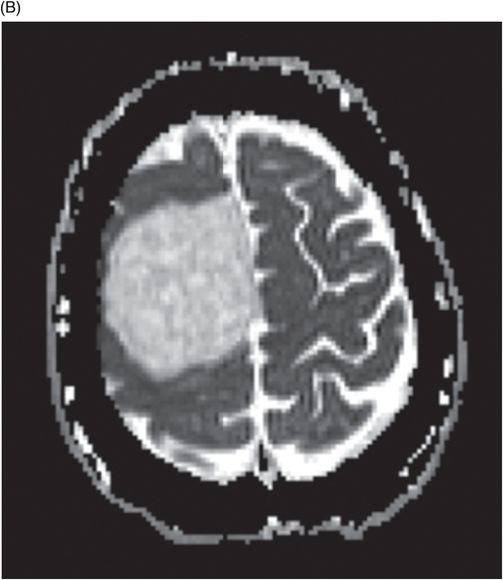
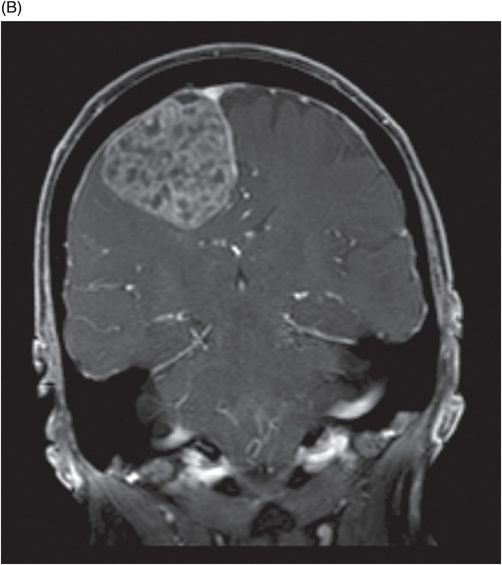
(A) Axial T1WI postgadolinium at the level of frontoparietal convexities and (B) Coronal T1WI fat-suppressed postgadolinium.
Dural Convexity Chondroma
Primary Diagnosis
Dural convexity chondroma
Differential Diagnoses
Meningioma
Chondrosarcoma
Extra-axial metastasis
Calcified hematoma
Extra-axial neurinoma
Imaging Findings
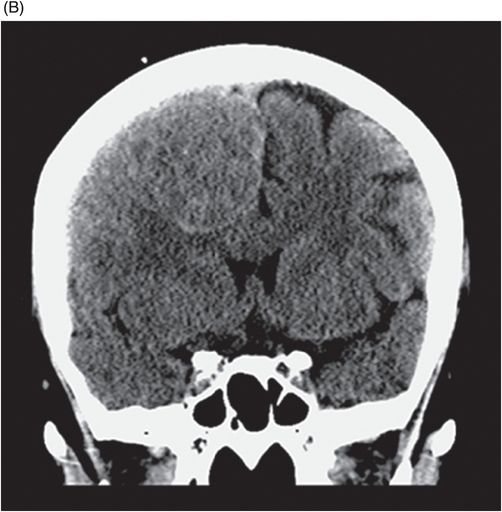
Fig. 98.1: (A) Axial non-contrast CT and (B) Coronal images showed a heterogeneous, spontaneously hyperdense extra-axial mass lesion arising from the right frontal convexity. Fig. 98.2: (A) Axial T1WI and (B) Sagittal T1WI showed a hypointense lesion. Fig. 98.3: Axial T2WI and Fig. 98.4: Axial FLAIR sequences showed that the lesion is hyperintense with mass effect. Fig. 98.5: (A) DWI and (B) ADC sequences demonstrated facilitated diffusion. Fig. 98.6: (A) Axial T1WI postgadolinium and (B) Coronal T1WI showed moderate and heterogeneous enhancement.
Discussion
Differential diagnosis of a well-defined, hyperdense extra-axial tumor that exhibits moderate enhancement, and lacks perilesional edema, dural tail sign, and diffusion restriction should include chondroma, or other extra-axial lesions.
Chondromas are rare benign tumors that can arise at sites in the body containing cartilaginous bone. They are predominantly seen in short, tubular bones, especially metacarpals and phalanges; they are known to have an association with Ollier disease, Maffucci syndrome, and Noonan syndrome. In the head and neck region, they are frequently seen at the skull base, arise from the embryonic cartilaginous remnants, and involve the synchondroses of middle cranial fossa. They tend to have a predilection for spheno-ethmoidal, spheno-petrosal, spheno-parietal, and petro-occipital regions, which account for the majority of all cases. Intracranial chondromas are exceedingly rare and constitute approximately 0.2–0.5% of all tumors. Approximately 15–20% of chondromas originate from the dural lining around the convexity. Isolated case reports describe less common locations including the falx, choroid plexus, and brain parenchyma. These tumors tend to occur between the second and sixth decades of life, with a peak incidence in the third decade but no gender preference. Although uncommon in the pediatric age group, they have been known to occur as early as 15 months of age. The histopathogenesis of intracranial chondromas remains controversial; however, four theories have been proposed: 1) metaplasia of meningeal fibroblasts; 2) metaplasia of perivascular mesenchymal tissue; 3) development from heterotopic chondrocytes; and 4) cartilaginous activation of fibroblasts by trauma or inflammation.
Clinical presentation is location-dependent and often delayed as they are slow-growing tumors. Non-specific symptoms are due to mass effect and raised intracranial pressure, which cause headache, seizures, cranial nerve palsies, deafness, visual impairment, limb weakness, and unsteady gait.
Computed tomography and MRI have key imaging features differentiating chondromas from meningiomas and other extra-axial neoplasms. On CT, the tumor density depends on the extent of calcification. Calcifications are common, occurring in 60% of all intracranial chondromas. Stippled, flocculent, and ring calcifications are often found in convexity chondromas. Falx chondromas, however, typically lack calcifications. Based on their CT imaging features they have been classified into two broad categories. Type I lesions are referred to as classic chondroma, which are isodense and homogeneous; type II tumors have central hypodense areas. Chondromas exhibit mild to moderate degree of enhancement, after intravenous contrast administration, especially on the delayed phase, and often lack the dural tail sign. Peritumoral edema is very rare. These key features are vital in differentiating a chondroma from a meningioma. However, 10–15% of meningiomas have atypical peripheral enhancement with cystic degeneration due to necrosis and lipidization. Cranial chondromas are avascular on angiography, in contrast to meningioma. On MR imaging, the tumor is iso- to hypointense on T1WI and hyperintense on T2WI and FLAIR images. Patchy, honeycomb pattern of enhancement on postgadolinium studies resembling punica granatum seeds sign has been described. Lack of diffusion restriction is another important imaging feature.
Chondrosarcomas are typically hypo- to isointense on T1 and hyperintense on T2 with strong heterogeneous enhancement. Extra-axial metastases have similar imaging features to meningioma in terms of enhancement, perilesional edema, and lack the typical calcification seen in chondroma. Calcified hematoma can have heterogeneous or usually peripheral calcification, enhancement, and exhibit T2 shortening on gradient and susceptibility sequence. Extra-axial neurinomas have a heterogeneous T2 hyperintense signal with significant enhancement and often lack calcification.
Complete surgical resection of the tumor and dural attachment is the treatment of choice with typically favorable outcome. Postsurgical patients have good long-term prognosis and no recurrence in cases with total lesion removal. Cellular atypia in resected specimens is an indicator of malignant transformation. Chondrosarcomas are known to have almost 20% recurrence rates. Chondromas do not respond to radiation; thus, radiation should not be used to treat patients with incomplete resection or non-resectable tumors. On the contrary, radiotherapy can increase the risk of malignant transformation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree