Chapter 72 Overview: Partial anomalous pulmonary venous connection (PAPVC) is present when one or more pulmonary veins drain into a systemic vein. Because a single anomalous connection may be unrecognized, the incidence is difficult to establish, but it has been reported to be present in one in 200 postmortem examinations.1,2 Etiology, Pathophysiology, and Clinical Presentation: All pulmonary veins from one lung may have anomalous drainage, or parts of the lung may have anomalous drainage to the same or different systemic veins. Anomalous drainage of the left pulmonary veins is most often to the brachiocephalic vein or coronary sinus.3 On the right, anomalous drainage is most often to the superior vena cava (SVC), right atrium, and inferior vena cava (IVC).4 When there is anomalous pulmonary venous drainage of all the right pulmonary veins, or just the middle and lower lobe veins to the IVC, scimitar syndrome is present. Other anomalies associated with scimitar syndrome include hypoplasia of the right lung and bronchial system, hypoplasia of the right pulmonary artery, systemic arterial supply to the right lower lung, and pulmonary sequestration.5–8 Approximately 67% of patients with partial anomalous pulmonary venous return also have atrial-level defects, most commonly a sinus venosus defect (see Chapter 73).9 Sinus venosus defects are not true atrial septal defects (ASDs) but occur as a result of deficiency of the wall between the SVC and the right upper pulmonary veins or of the wall between the right atrium and the right upper and lower pulmonary veins. Thus although a sinus venosus defect does not represent an abnormal pulmonary venous connection with a systemic vein, a superior sinus venosus defect often is associated with anomalous drainage of the right pulmonary veins to the SVC or to the right atrium. With an intact atrial septum, the amount of blood draining through anomalous veins depends on the number of anomalous draining veins, the compliance of the atria, and the resistance of the pulmonary vascular beds. Anomalous connection of one pulmonary vein usually is not clinically apparent in childhood, but these patients may present in the third and fourth decades with cyanosis resulting from increased pulmonary vascular resistance.10 If all but one of the pulmonary veins drains anomalously, the clinical manifestations may be similar to total anomalous pulmonary venous connection. If they are associated with a sinus venosus septal defect, signs and symptoms usually are related to the amount of shunting through the defect. Patients with scimitar syndrome may present in infancy with pulmonary hypertension from the arterial supply to the right lower lung, stenosis of the anomalous pulmonary veins, or pulmonary infections. Otherwise, this syndrome may be detected in adulthood in persons who do not have significant symptoms.11 Imaging: With anomalous drainage of multiple veins, cardiomegaly with right heart enlargement and increased pulmonary flow are seen on chest radiography. Findings with scimitar syndrome include a crescent-shaped anomalous pulmonary vein (resembling a Turkish sword or scimitar) paralleling the lower right heart border (Fig. 72-1). Patients generally have associated hypoplasia of the right lung, a small right pulmonary artery, and varying degrees of cardiac dextroposition. Figure 72-1 Scimitar syndrome. Cross-sectional imaging goals include identifying the anomalous pulmonary to systemic venous connection, locating each pulmonary vein and its drainage relative to the left atrium, and determining the location of venous obstruction, if present (e-Fig. 72-2). Evaluation for the presence and size of either an ASD or sinus venosus defect, is necessary (e-Figs. 72-3 and 72-4). The heart and great vessels are evaluated for other abnormalities, and when scimitar syndrome is present, the upper abdomen should be assessed for anomalous venous drainage and systemic supply to the lung (Fig. 72-5). Both computed tomography (CT) and magnetic resonance imaging (MRI) are highly sensitive and specific for evaluation of anomalous pulmonary venous drainage, and three-dimensional CT or magnetic resonance angiography is very useful for identifying the relationship between the anomalous pulmonary veins and the left atrium.12,13 MRI also is useful for ASD evaluation and for quantification of systemic to pulmonary shunting. CT and MRI are accurate in assessing for postoperative pulmonary vein obstruction or narrowing (e-Fig. 72-6).13–15 Figure 72-5 Scimitar syndrome. e-Figure 72-2 Partial anomalous pulmonary venous connection (PAPVC). e-Figure 72-3 Partial anomalous pulmonary venous return in the setting of a superior sinus venosus defect. e-Figure 72-4 Sinus venosus defect with partial anomalous pulmonary venous return. e-Figure 72-6 Severe right pulmonary vein stenosis. Treatment: Surgical correction is indicated when the ratio of pulmonary to systemic arterial flow is greater than 1.5 : 1; outcomes generally are excellent.4 In patients with scimitar syndrome, pulmonary resection or catheter occlusion of the anomalous arterial blood supply may be necessary. The anomalous vein in patients with scimitar syndrome may be anastomosed directly to the left atrium. Superior sinus venosus defects may be closed with a patch at the junction of the SVC and right atrium, with baffling of the pulmonary venous return to the left atrium. Alternatively, the SVC is divided above the pulmonary veins, with implantation of the SVC to the right atrial appendage and baffling of the SVC orifice with the right pulmonary venous return to the left atrium. The incidence of postoperative SVC or pulmonary vein stenosis is less than 10%.16 Overview: Total anomalous pulmonary venous connection (TAPVC) is a congenital anomaly in which all of the pulmonary veins connect to the systemic venous circulation rather than to the left atrium. TAPVC accounts for approximately 1% to 5% of all congenital heart disease,17,18 with a male predominance when the anomalous connection is to the portal vein.19 TAPVC often is present in patients with visceral heterotaxy and asplenia and single-ventricle physiology.18 Etiology, Pathophysiology, and Clinical Presentation: The cause of TAPVC is thought to be lack of incorporation of the common pulmonary vein into the left atrium. In type I or supracardiac TAPVC (49% of cases), all four pulmonary veins join to form a confluent pulmonary vein posterior to the left atrium and then most commonly connect to a persistent left vertical vein, which drains to the left brachiocephalic vein and to the right SVC or via the right ascending vein to the right SVC. In type II or cardiac TAPVC (16% of cases), the pulmonary veins form a confluence that drains either directly into the right atrium or to the coronary sinus, which then drains normally into the right atrium. In type III or infracardiac TAPVC (26% of cases), the pulmonary veins converge as a common pulmonary vein that extends below the diaphragm and drains to the portal vein, ductus venosus, hepatic vein, or IVC. Type IV TAPVC (9% of cases) is a mixed type in which the pulmonary veins drain separately to at least two different systemic sites, most commonly supracardiac and cardiac sites (e-Fig. 72-7 and Fig. 72-8).20 Figure 72-8 Three-dimensional computed tomography angiogram posterior views of different types of total anomalous pulmonary venous connection (TAPVC). e-Figure 72-7 Darling classification of total anomalous pulmonary venous connection (TAPVC).
Abnormal Pulmonary and Systemic Venous Connections
Partial Anomalous Pulmonary Venous Connection and Scimitar Syndrome
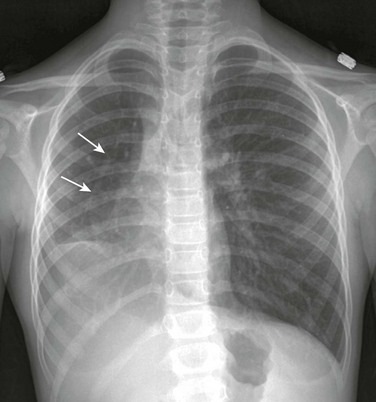
A frontal chest radiograph shows the rightward shift of the mediastinum as a result of right lung hypoplasia. In the right side of the chest, a linear density indicative of the anomalous draining “scimitar” vein is seen (arrows).
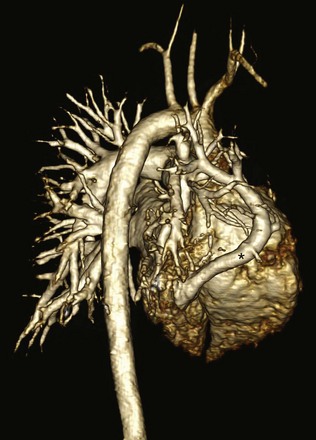
A three-dimensional magnetic resonance angiogram viewed from right posterior oblique shows the anomalously draining right pulmonary “scimitar” vein (asterisk) extending to the inferior vena cava.
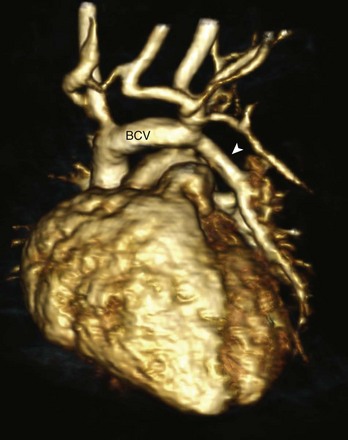
A three-dimensional magnetic resonance angiogram viewed from the left anterior oblique projection shows the PAPVC (arrow head) from the left upper lobe with drainage to the left brachiocephalic vein (BCV).
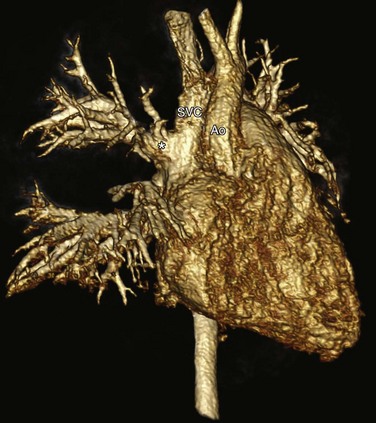
A right anterior oblique three-dimensional magnetic resonance angiogram shows the right upper pulmonary veins (asterisk) draining to the SVC. SVC, Superior vena cava; Ao, aorta.
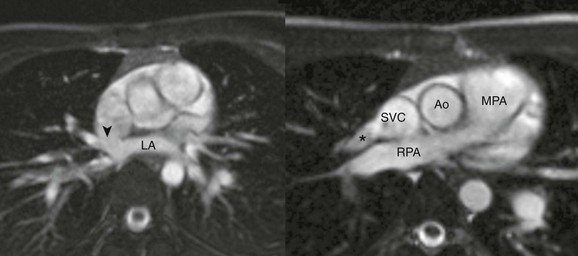
A, An axial cine steady-state free-precession (SSFP) image shows the sinus venosus defect (arrowhead) located superior to the expected location of the oval fossa, consistent with a superior sinus venosus defect. B, Oblique axial SSFP located superior to (A) showing the right upper pulmonary vein (asterisk) draining to the superior vena cava. Ao, Aorta; LA, Left atrium; MPA, main pulmonary artery; RPA, right pulmonary artery; SVC, superior vena cava.
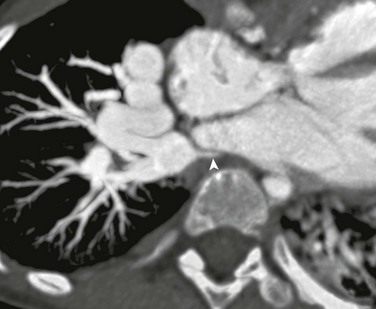
A computed tomography axial oblique reformat 5 years after repair of obstructed supracardiac total anomalous pulmonary venous connection with separate anastomoses of the right and left pulmonary veins to the left atrium. Severe right pulmonary vein stenosis (arrowhead) is present at the anastomotic site.
Total Anomalous Pulmonary Venous Connection
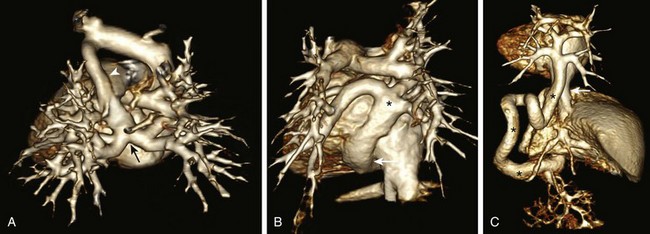
A, Supracardiac TAPVC. The pulmonary venous confluence (arrow) connects to the ascending vertical vein (arrowhead), the brachiocephalic vein, and the enlarged superior vena cava. B, Cardiac TAPVC. The pulmonary venous confluence (asterisk) connects to the coronary sinus (arrow). C, Infracardiac TAPVC. The pulmonary venous confluence extends below the diaphragm via a tortuous descending vertical vein (asterisks) to connect with the portal vein (arrow) inferior vena cava.
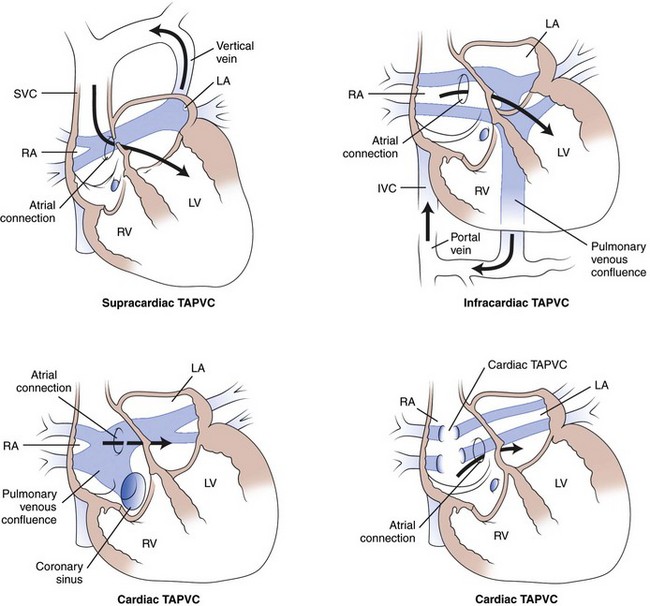
With supracardiac TAPVC, pulmonary venous connection is to a vertical vein, draining to the left brachiocephalic vein and superior vena cava (SVC). With infracardiac TAPVC, the pulmonary veins connect to a systemic venous vessel below the diaphragm (the portal vein in this diagram). With cardiac TAPVC, the pulmonary veins connect either to the coronary sinus or directly to the right atrium (RA). The direction of systemic blood flow (dark arrows) is shown. Note that blood must flow through an atrial connection to reach the left side of the heart. IVC, Inferior vena cava; LA, left atrium; LV, left ventricle; RV, right ventricle. (From Wilson A. Total anomalous pulmonary venous connection, E-Medicine, March 28, 2006.)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







