Chapter 83 Pathology of the aorta can be categorized into aortic aneurysm, aortic dissection, and aortic stenosis.1 Although each aortic disease may present one or more of these manifestations, it is the clinical consequences of aneurysm, dissection, or stenosis that determine mortality and morbidity (Table 83-1). Table 83-1 Principal Etiologies of Acquired Aortic Diseases Normally, the caliber of the aorta gradually decreases in size from the sinotubular junction to the aortic hiatus. An aortic aneurysm is defined as an abnormal dilation of the aorta, which may undergo progressive expansion. An aortic aneurysm may form if wall stress increases, as in the case of systemic hypertension, or if the aortic wall weakens, as in the case of Marfan syndrome (see Chapter 79). The expansion rate of an aneurysm is determined by the wall stress, which increases with diameter. Thus a large aneurysm is more likely to expand than a small aneurysm, and the expansion is an accelerating process until rupture occurs. Overview: Trauma is a major cause of death in children and results primarily from motor vehicle accidents, although firearm injury (Fig. 83-1) and child abuse are other important causes of traumatic death. Survival of a child with a traumatic aortic injury until arrival at the emergency department is rare, accounting for one to two cases per year at large metropolitan level I pediatric trauma centers. Operative treatment involves fewer than 0.14% of all trauma patients, and only 6% of all traumatic ruptures of the aorta occur in patients younger than 16 years.2,3 The outcome of traumatic aortic injury in the pediatric population is directly related to timely diagnosis, proper treatment, and hemodynamic status at the time of presentation. Figure 83-1 An aortic false aneurysm from a gunshot wound in an 18-year-old man. Imaging: Chest radiographic findings such as pleural capping at the left lung apex, obscuration of the aortic arch, mediastinal widening, pleural effusion, pneumothorax, pulmonary contusion, tracheal and nasogastric tube deviation, and upper rib and clavicle fracture in the setting of blunt trauma should raise clinical suspicion for an aortic injury (Fig. 83-2). Historically, the definitive diagnosis of traumatic aortic injury was made by conventional catheter angiography. Today, computed tomographic angiography (CTA) has supplanted catheter angiography as the diagnostic method of choice.4,5 CTA allows speedy and precise visualization of the traumatic aortic injury. Care should be taken to identify the location of aortic rupture, active extravasation of arterial contrast, a dissection flap extending to major aortic branches, hemothorax and hemopericardium, and other organ and musculoskeletal injuries. Figure 83-2 Aortic rupture in a 16-year-old boy as a result of a motor vehicle accident. Treatment and Imaging Follow-up: The goals of treatment of pediatric traumatic aortic rupture are identical to those in adults. The mainstay of treatment is operative repair of the aorta.6 Patients for whom surgery poses a high risk have been treated successfully with endovascular stent grafts, with deployment during adenosine-induced cardiac arrest. CTA should be performed immediately after stent placement, with a follow-up study in 48 hours to document the stability of the repair. Rarely, observational management for an intimal tear has been utilized in patients with comorbidities too severe to allow intervention. Overview: Pulmonary embolism (PE) is an uncommon but potentially fatal disease in children.7 In pediatric patients with deep venous thrombosis and PE, the mortality rate from all causes has been reported to be as high as 16%, whereas the mortality rate directly attributable to deep venous thrombosis or PE was 2.2%.8 The most common risk factor for PE in children is catheter thrombosis, which develops in as many as 50% of patients with central venous catheters.9 Other risk factors are peripartum asphyxia, dehydration, septicemia, trauma and burns, surgery, hemolysis, malignancy, and renal disease such as nephrotic syndrome. Rarely, PE can be seen in the setting of intracranial venous sinus thrombosis and Klippel-Trénaunay syndrome. Abnormal coagulation factors associated with adult PE that also have been reported in children are antiphospholipid antibodies, factor V Leiden mutation, and deficiencies in protein S, protein C, and antithrombin III.10 Imaging: Traditionally, catheter pulmonary angiography was considered the diagnostic gold standard.11 In current clinical practice, catheter pulmonary angiography has been replaced by noninvasive CT pulmonary angiography (CTPA) performed with high-speed multidetector CT. The accuracy of the detection of PE by CTPA in an adult population has been studied in the Prospective Investigation of Pulmonary Embolism Diagnosis II trial.12
Acquired Diseases of the Thoracic Great Vessels
Acquired Diseases of the Thoracic Aorta
Manifestation
Causes
Aortic aneurysm
Infectious aortitis
Inflammatory aortitis
Takayasu syndrome (acute, chronic)
Systemic lupus erythematosus
Sarcoid
Connective tissue disease
Marfan syndrome
Ehlers-Danlos syndrome (vascular type)
Loeys-Dietz syndrome
Arterial tortuosity syndrome
Neurocutaneous disease
Tuberous sclerosis
Trauma or postsurgical (pseudoaneurysm)
Aortic dissection
Connective tissue disease
Marfan syndrome
Ehlers-Danlos syndrome (vascular type)
Trauma
Aortic stenosis
Inflammatory aortitis
Takayasu syndrome (chronic)
Congenital rubella syndrome
Radiation
Neurocutaneous disease
Neurofibromatosis (type I)
PHACES syndrome
Postsurgical
Coarctation repair
Aortopulmonary shunts
Trauma
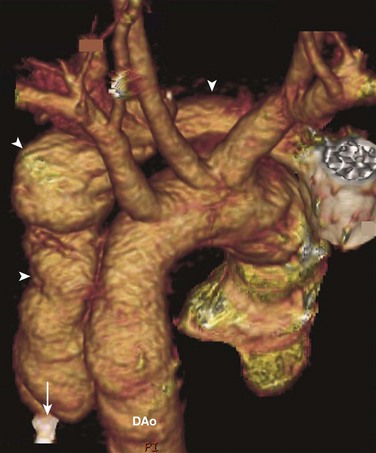
Volume rendering of a computed tomography angiogram shows a false aneurysm (arrowheads) that follows the track of a bullet. The bullet first entered the chest horizontally, parallel to the aortic arch, rupturing the aorta. Then it was deflected downward and came to rest (arrow) adjacent to the descending aorta (DAo).
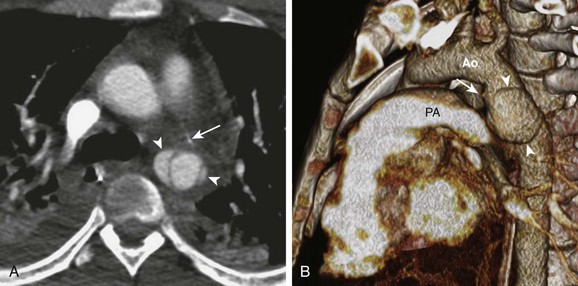
A, An axial image from a computed tomography (CT) angiogram shows a ruptured descending aorta at the level of the ligamentum arteriosum (arrow) and two pseudoaneurysms (arrowheads) extending beyond the aortic wall. B, A volume-rendered image of the CT angiogram shows the relationship between one of the pseudoaneurysms (arrowheads) and the ligamentum arteriosum (arrow) between the aorta (Ao) and the pulmonary trunk (PA).
Acquired Diseases of the Pulmonary Artery
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree