Chapter 99 The esophagus is a muscular tube that transports food and oral secretions from the mouth to the stomach via coordinated peristalsis of striated and smooth muscle.1 A number of acquired disorders prevent the esophagus from functioning normally. These disorders generally present with symptoms such as dysphagia, food sticking, or food bolus impaction. In addition, a number of self-inflicted, accidental, or iatrogenic injuries are common in the pediatric esophagus. An esophagram or an upper gastrointestinal (UGI) series is the most common method used to image the esophagus directly. The two fluoroscopic studies differ in that an UGI provides a more complete evaluation of the upper gastrointestinal tract, extending from the mouth through the proximal jejunum, whereas an esophagram typically focuses on the upper gastrointestinal tract between the mouth and body of the stomach. Both studies allow the radiologist to evaluate the anatomy and function of the esophagus by watching a contrast bolus move through the esophageal lumen (see Chapter 98 for a more complete description of the technique). Computed tomography (CT) and magnetic resonance imaging (MRI) are rarely used as primary methods of imaging the esophagus; however, both CT and MRI have the advantage of allowing the radiologist to visualize the esophageal wall and lesions extrinsic to the esophagus.2 Use of cross-sectional imaging to evaluate the esophagus has several major limitations that prevent their use as a primary imaging modality: first, neither CT nor MRI provides functional information of esophageal motility; second, the esophagus is not able to be distended reliably to evaluate wall thickness accurately; third, and neither study is able to provide mucosal detail. Overview: GER is defined as the retrograde passage of gastric contents into the esophagus.3 When symptoms or lesions occur as a result of GER, it is referred to as gastroesophageal reflux disease (GERD).4 The primary mechanism of GER is transient relaxation of the lower esophageal sphincter. This relaxation can be triggered by vasovagal reflex initiated by gastric distension or cardiopulmonary receptors or by a swallow that does not trigger esophageal peristalsis.3 In children, severe GERD has several known risk factors, including neurologic disorders such as spastic quadriplegia and cerebral palsy, esophageal atresia, chronic lung disease such as cystic fibrosis, and hiatal hernia.5,6 Clinical Presentation: GER is ubiquitous in infants, occurring in 100% of 3-month-olds, 40% of 6-month-olds, and 5% to 20% of 1-year-olds.4,6 In children and adolescents, GERD increases in incidence with age. Symptoms of GERD are reported to occur on a weekly basis in 2% of 3- to 9-year-olds and 5% to 8.2% of children aged 10-17 years.7 The symptoms of GERD depend on age. In infants, symptoms include irritability, feeding difficulty, poor weight gain, and sleep disturbance. In older children, symptoms include heartburn, abdominal pain, regurgitation or vomiting, and dysphagia.3 Extraesophageal symptoms of GERD also can occur and include chronic cough, asthma, apnea, bradycardia, sore throat, dental erosions, and recurrent otitis or sinusitis.3 When compared with adults, children report fewer episodes of heartburn, dysphagia, and chest pain and more episodes of vomiting and regurgitation.4 GERD often is diagnosed on the basis of symptoms and a trial of acid-reduction therapy. When symptoms are not specific or are atypical, confirmatory testing can be performed. Intraesophageal pH monitoring traditionally has been thought of as the gold standard because of its ability to measure the pH in the esophagus over a long period. The main limitation of this technique is that patients may have abnormal esophageal acid exposure without symptoms of GERD or retrograde bolus movement in the esophagus.3,8 To evaluate for the retrograde passage of gastric contents and esophageal acidity, combined pH/impedance probes are used.8 Imaging: UGI imaging often is performed in the setting of GER to evaluate for an anatomic abnormality; however, it should not be used as the primary method of diagnosing GER or GERD. UGI has multiple limitations in diagnosing GER, including its nonstandard technique, lack of correlation with symptoms, and use of ionizing radiation. Methods used to provoke reflux such as the Valsalva maneuver, positional changes, abdominal compression, or leg lifting may increase the sensitivity of detecting GER but lower the specificity.3 Because more sensitive diagnostic tests are available and the radiologic findings do not correlate with symptoms, the collaborative practice guideline set forth by the American College of Radiology and the Society for Pediatric Radiology do not recommend provocative maneuvers or prolonged fluoroscopy for the detection of GER.9 Even though UGI imaging should not be prolonged to identify GER, GER often is present (Fig. 99-1). The percentage of patients who have GER on UGI imaging decreases with age from 80% of infants <18 months to 30% of adolescents between 12 and 18 years.3 It should be noted that although the height of reflux often is reported as a surrogate for its severity, no correlation exists between the height of GER on UGI imaging and symptoms of GERD.3 Figure 99-1 Gastroesophageal reflux. Esophageal complications of GERD include esophageal strictures and Barrett esophagitis. Esophageal strictures, also known as peptic strictures when they are caused by GERD, typically occur in the lower third of the esophagus and are a result of acidic injury. They are cited as being present in up to 15% of children with GERD and can occur at any age.10 Many patients who experience strictures have an associated comorbidity, with 25% having a neurologic impairment.10 Barrett esophagus is defined as metaplasia of cells in the distal esophagus from squamous to columnar epithelium. Its prevalence in children with GERD ranges from 0.25% to 4.8%.6,11 Risk factors for the development of Barrett esophagus in children include severe chronic GERD, congenital abnormalities, neurologic impairment, hiatal hernia, and family history.6 Although it is associated with a thirtyfold increase in esophageal adenocarcinoma in adults, the risk of developing adenocarcinoma is not defined in children.6 Treatment: Multiple options exist for treating GERD, depending on the patient’s age, comorbidities, and severity of symptoms. Generally, lifestyle changes and pharmacotherapy are first-line options. Lifestyle changes include avoidance of overfeeding, thickening feeds, upright positioning during sleep, and avoidance of second-hand smoke.3 A goal of medical therapy is to decrease the acidity of the refluxed gastric contents, which is generally performed by using proton pump inhibitors and histamine receptor antagonists.3 In patients with continued severe GERD after pharmacotherapy or other comorbidities such as neurologic impairment, antireflux surgery such as Nissen fundoplication is performed. Strictures are treated with esophageal dilation and fundoplication. In a small percentage of patients, severe and recurrent strictures will require extensive and repeated dilatations and may require surgical resection or replacement of the esophagus.10 Ingested foreign bodies are common in children, with most occurring in children younger than 3 years.12 The American Association of Poison Control Centers reported approximately 125,000 foreign body ingestions in pediatric patients in 2009.13 This number is only a fraction of the actual number of foreign bodies ingested because it represents only the ingestions that are reported to poison control centers. Overview: In the United States and Europe, coins are the most commonly ingested foreign body.12 It is estimated that 4% of all children swallow a coin.14 Although most coins spontaneously pass through the gastrointestinal tract, they can lodge in the esophagus. Coins typically lodge in one of three locations: the thoracic inlet (60% to 70%), the mid esophagus at the level of the aortic arch (10% to 20%), and just above the lower esophageal sphincter (20%).12 Clinical Presentation: Symptoms of chronic foreign body impaction include respiratory distress, asthma symptoms, cough, nausea, vomiting, and dysphagia. Respiratory symptoms are a result of local inflammation surrounding the foreign body.14 Patients with chronic foreign body impaction are at risk of esophageal perforation. Imaging: Radiographs are useful to identify the location of the coin and to look for signs of chronic impaction. Coins generally are described as oriented in the coronal plane when they are located in the esophagus on the frontal radiograph, although reports have been made of sagittally oriented coins in the esophagus.15 Inflammatory changes that develop in patients with chronic foreign body impaction can be visualized as thickening of the space between the esophagus and trachea on lateral chest radiographs (e-Fig. 99-2, A and B); these changes therefore are useful in patients in whom the episode was not witnessed and the time course is not known. An esophagram often is performed in patients with a chronic foreign body impaction to evaluate for perforation or development of a tracheoesophageal fistula. e-Figure 99-2 A swallowed coin. Treatment: Coins, like other esophageal foreign bodies, can be removed via Foley catheter balloon extraction or endoscopy. Foley catheter extraction has been used as a safe and effective method of coin removal in children older than 1.5 years before esophageal edema has developed.16 Despite its history of safe extractions and lower cost, Foley balloon extraction has fallen from favor because of concerns about patient safety related to airway compromise or esophageal injury.17 Endoscopy is now the preferred method for extraction at most centers. Overview: Button battery ingestion by children is increasing in frequency.18 Button batteries often are found in objects such as watches, calculators, toys, and hearing aids. Management of battery ingestion is different than that of coins, because batteries lodged in the esophagus can cause severe damage in as little as 2 hours.18 Tissue damage is caused by one of three mechanisms: leak of alkaline contents, pressure necrosis, and generation of a current causing electrolysis of tissue fluids at the battery’s negative pole.18 Clinical Presentation: If ingestion is witnessed, extraction should occur before the development of symptoms. If symptoms develop, they include drooling, chest discomfort, choking, gagging, and airway obstruction. Damage can include esophageal perforation or creation of a fistula to the trachea or to a major blood vessel, leading to exsanguination.18 Imaging: Batteries can be distinguished on radiographs by their characteristic halo appearance with a circle of lucency just within the outer border (Fig. 99-3 and e-Fig. 99-4). An esophagram with water-soluble iso-osmolal contrast can be performed after removal to evaluate for the presence of complications, such as esophageal perforation or a tracheoesophageal fistula. Figure 99-3 A swallowed battery. e-Figure 99-4 The swallowed battery from Figure 99-3. An oblique view from the esophagram shows contrast in both the esophagus and the tracheobronchial tree as a result of the tracheoesophageal fistula. Overview: Impacted food boluses are relatively infrequent in children but may be the initial presenting symptom of eosinophilic esophagitis, peptic stricture, achalasia, vascular rings, or an extrinsic mass.19,20 Eosinophilic esophagitis is the major cause of food bolus impaction in children, accounting for >50% of all cases. The most common remaining cause of food bolus impaction in children is an area of narrowing in a patient with prior esophageal atresia repair or Nissen fundoplication surgery.21 Clinical Presentation: Acute impaction of food typically leads to symptoms of dysphagia and drooling; difficulty swallowing may lead to aspiration. Imaging: On UGI imaging, an impacted food bolus appears as a persistent filling defect in the esophagus (Fig. 99-5). The impacted food can completely obstruct the esophagus, which is seen on UGI imaging as a standing column of contrast that does not pass beyond the food bolus. Treatment: When a food bolus is identified, it is removed endoscopically. An esophagram can be performed after extraction or passage of the food bolus to evaluate for the underlying cause, if it is not already known. An esophageal biopsy is recommended in patients diagnosed with food bolus impaction, particularly if they do not have a history of prior esophageal surgery. Overview: Ingestion of caustic materials remains relatively common in childhood. In 2009, a total of 212,263 ingestions of household cleansers were reported to the American Poison Control Centers, more than 75% of which occurred in children.13 The age group at highest risk for caustic ingestion is children younger than 5 years,13 with a peak around 2 years of age when children are learning to explore their home but are not yet able to distinguish between harmless and harmful substances.22 Whereas caustic ingestion is usually accidental in children, in adults or adolescents it is usually purposeful. The extent and severity of injury depends on several factors: the corrosiveness of the ingested substance, the quantity ingested, the physical state of the substance, the duration of the contact time of the substance with the esophagus, and subsequent secondary infection.22,23 A variety of substances can cause a caustic injury, including alkalis (pH up to 12) and acids (pH as low as 2). In contrast to acidic substances, which are sour, alkalis have a relatively innocuous taste, leading to ingestion of a greater volume.22 Further, alkaline agents produce liquefaction necrosis and rapid penetration, leading to more severe injury.23 Clinical Presentation: After caustic ingestion, patients with severe injury typically present with pain, drooling, and airway symptoms; more visible signs of tissue damage include lip swelling, mouth ulcers, and erythema of the tongue.22 Esophageal stricture is an important late complication of caustic ingestion, occurring in 2% to 63% of patients23; it can form in as little as 3 weeks after injury.24 Imaging: Initial management of patients with caustic ingestion includes a radiograph of the chest and lateral neck to evaluate for pneumomediastinum. An esophagram is not indicated in the acute phase because it delays endoscopy and does not reveal mucosal injuries.22 When strictures develop, they can be diagnosed on the basis of symptoms and confirmed with an esophagram (Fig. 99-6 and e-Fig. 99-7). Caustic strictures can be focal or can occupy a long segment of the esophagus depending on the substance ingested; acid ingestion typically causes a focal or short segment stricture, whereas alkali substances cause a long segment stricture.24 Strictures most commonly occur in the upper or mid esophagus. Multiple strictures also can occur. Figure 99-6 Caustic ingestion. e-Figure 99-7 An esophagram in the patient shown in Figure 99-6 after the esophageal perforation had healed shows a stricture in the mid esophagus (arrow). The esophagus proximal to the stricture is dilated. Treatment: Acutely, patients are treated with steroids, proton pump inhibitors, and antibiotics. Endoscopic evaluation is performed to assess the extent of damage and to grade the injury. Strictures are first treated with balloon dilation under fluoroscopy. The advantage of balloon dilation over dilation using a bougie is that balloons dilate strictures in a radial direction rather than in a longitudinal direction. This is thought to be less likely to cause an esophageal perforation.22 After the balloon is inflated and the waist is seen to disappear, an esophagram is performed to evaluate for a leak that occurs in 4% to 30% of patients.24 If balloon dilation fails, operative treatment with either stricture resection or esophageal replacement is performed. Patients with a history of caustic ingestion are at risk of developing squamous cell carcinoma of the esophagus. Given this risk, these patients should undergo surveillance with endoscopy as adults.22 Overview: Pill esophagitis is an esophageal injury caused by medications; the drugs most frequently implicated are doxycycline and alendronate.25 Other drugs reported to cause esophageal injury include nonsteroidal antiinflammatory drugs, potassium chloride, ferrous sulfate, phenytoin, and quinidine.25 Characteristics of medications that are more likely to cause esophageal injury include the acidity of the medication and a capsule formulation that renders it more likely to stick in the esophagus.26 Pill esophagitis is also more likely to occur in patients with delayed esophageal transit time. Factors that delay esophageal transit include taking a pill with little or no water immediately before going to bed, decreased saliva production, and anatomic areas of narrowing.26 Clinical Presentation: Patients with pill esophagitis typically present with dysphagia, odynophagia, and chest pain. Pill esophagitis often can be diagnosed by history alone. Imaging: UGI imaging is not commonly performed due to the classic history but can show a circular area of ulceration. If endoscopy is performed, a circular ulceration is identified with normal surrounding mucosa. The ulceration typically occurs at an anatomic area of narrowing such as at the level of the aortic arch, left mainstem bronchus, or gastroesophageal junction.26
Acquired Esophageal Disorders
Overview
Imaging
Gastroesophageal Reflux

Image from an upper gastrointestinal examination shows retrograde flow of contrast from the stomach into the esophagus. Note the wide-open esophageal sphincter.
Trauma
Coins
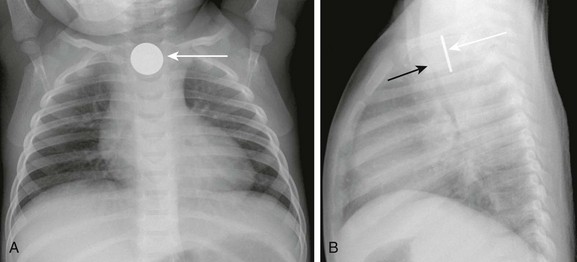
A, A frontal radiograph of the chest shows a coin lodged in the proximal esophagus (arrow) at the level of the thoracic inlet. B, A lateral view of the chest shows the coin (white arrow) lodged in the proximal esophagus. The trachea (black arrow) is located anterior to the esophagus and is narrowed at the level of the foreign body. Thickening of the space between the esophagus and trachea can be seen.
Batteries
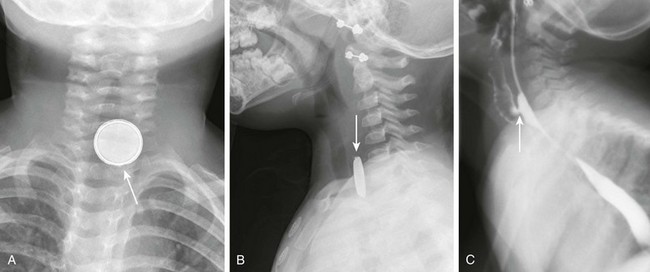
A, A frontal radiograph of the airway shows a button battery (arrow) lodged in the proximal esophagus. The inferior margin of the battery is eroded and has an irregular edge. Note that the battery has a characteristic appearance with alternating dense and lucent bands. B, A lateral radiograph of the airway shows the button battery (arrow) lodged in the proximal esophagus. On the lateral view, the edge of the battery has a beveled appearance. C, A lateral view from an esophagram after removal of the battery shows a tracheoesophageal fistula (arrow) at the site where the battery was lodged.

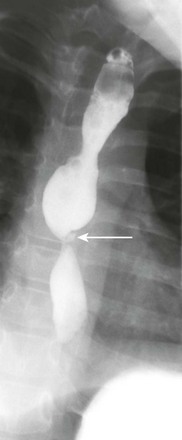
Food Bolus Impaction
Caustic Ingestion
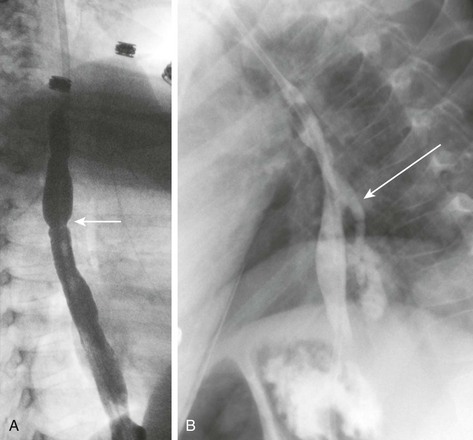
A, An esophagram in a patient with a recent history of lye ingestion shows an irregular contour of the esophagus and a focal area of narrowing (arrow). B, An esophagram in the same patient 3 months later and immediately after dilation of an esophageal stricture shows an esophageal perforation with leakage of contrast (arrow).
Pill Esophagitis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








