(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
Abstract
Due to compromised immunity and weakened defense function in patients with AIDS, opportunistic infections commonly occur. Nearly 80 % patients suffering from AIDS die from opportunistic infections. The pathogens causing opportunistic infections include the following four types: viruses, bacteria, fungi and parasites.
Keywords
Virus InfectionBacterial InfectionFungal Infection3.1 AIDS Related Pathogenic Microorganisms
3.1.1 Structure and Classification of Pathogenic Microorganisms
Due to compromised immunity and weakened defense function in patients with AIDS, opportunistic infections commonly occur. Nearly 80 % patients suffering from AIDS die from opportunistic infections. The pathogens causing opportunistic infections include the following four types: viruses, bacteria, fungi and parasites.
3.1.1.1 Virus Infection
Herpes viruses include varicella-zoster virus (VZV), cytomegalovirus (CMV), Epstein-Barr virus (EBV), herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). It is believed in literatures that in incidences of AIDS related opportunistic infections, CMV infection is only second to pneumocystis carinii infection. CMV infection is disseminating to infect almost all organs, with the most commonly infected including adrenal gland, lung and digestive tract. Herpes simplex virus (HSV) infections involve the skin and mucous membranes to cause local thin-walled herpes. In HIV infected patients, the incidence of lung diseases caused by herpes simplex virus infection is less than 2.2 %, including interstitial pneumonia with intra-interstitial infiltration of the mononuclear cells. Patients with AIDS have a higher occurrence of EB virus infection, 96 % patients being EBV antibodies positive. The infection rates of human herpesvirus type 6 (HIV-6), human herpesvirus type 7 (HIV-7) and human herpesvirus type 8 (HIV-8) are high in the general population. Their viral antigens can be detected in most AIDS patients, but with no detectable specific pathological changes.
3.1.1.2 Bacterial Infection
About 13–40 % of AIDS patients sustain bacterial infections, including escherichia coli, staphylococcus aureus, pseudomonas aeruginosa, haemophilus influenzae, streptococcus pneumoniae, klebsiella pneumoniae, and mycobacterium. In Europe and America, mycobacterium is the third common opportunistic pathogen attacking patients with AIDS. In AIDS-related tuberculosis, pulmonary tuberculosis is the most common, followed by lymphoid tuberculosis, hepatobiliary tuberculosis and renal tuberculosis.
3.1.1.3 Fungal Infection
Various fungal infections occur in patients with AIDS. In the United States and Africa, during the periods of AIDS-related syndromes and AIDS, 58–81 % patients are fungus infected. By autopsy, the detection rate of fungal infection is 8–40 %. The common fungi are candida albicans, cryptococcus neoformans, aspergillus, mucor, histoplasma, coccidioides, and pneumocystis carinii.
Candida Albicans
Candida infection is the most common infection in patients with AIDS. By autopsy, its detection rate is approximately 25 %. The pulmonary candida infection occurs in 23 % patients with AIDS but a low incidence of brain or kidney candida infection.
Pneumocystis Carinii
In Europe and America, pneumocystis carinii is the most common pathogen causing opportunistic infection in AIDS patients. Its incidence rate is 54–85 % by pathological autopsy for patients with AIDS. Pneumocystis carinii infection causes interstitial pneumonia and alveolar pneumonia. The over proliferation of pulmonary bacteria and exudative lesions lead to its extrapulmonary dissemination along lymph or blood circulation. About 2.5 % patients show involved lymph nodes, bone marrow, spleen, liver, gastrointestinal tract, pancreas and other parts of body.
3.1.1.4 Parasitic Infections
AIDS-related parasitic opportunistic pathogens include toxoplasma gondii, cryptosporidium, isospora, giardia lamblia, entamoebiasis histolytica, microsporidia, strongyloides stercoralis, blastocystis hominis and leishmania donovani. Toxoplasma gondii and cryptosporidium are the most common pathogens.
3.1.2 Characteristics of Pathogenic Microorganisms
3.1.2.1 Protozoon
Toxoplasma
Toxoplasma is an intracellular parasitic protozoan, categorized into the top complexes subphyla, cryptosporidium classis, eucoccidia order. As a zoonotic disease, toxoplasma infection can infect people when HIV infection develops into AIDS, resulting in serious consequences of central nervous system damage and systemic disseminated infection. Toxoplasma infection is primarily an animal infectious disease caused by a parasitic protozoan, mouse toxoplasma. Its transmission routes in human include congenital infection from mother to fetus via placenta and acquired infection caused by eating raw or undercooked meat containing tissue cysticercosis.
Cryptosporidium
Cryptosporidium is a small sized coccidia parasite, surviving in a variety of vertebrates. The diseases caused by cryptosporidium are called cryptosporidiosis, which is a zoonotic disease with a prominent symptom of diarrhea.
3.1.2.2 Virus
Cytomegalovirus
Cytomegalovirus is a herpes DNA virus, with an extensive existence. Most CMV infected patients are asymptomatic. Human CMV homogeneously spreads, with its proliferation in human fibroblasts. But CMV infected patients can excrete the viruses through urine, saliva, feces, tears, breast milk and sperm. Thus, CMV infection can be transmitted via blood transfusion, mother’s placenta, organ transplantation, sexual intercourse and breast milk feeding.
Herpes Simplex Virus
Herpes simplex virus is the most common pathogen attacking human body and human is its only natural host. The main transmission routes are direct contact and sexual contact. It also can be transmitted through droplets. The viruses gain their access to the human body via the respiratory tract, mouth, eyes, genital mucosa or lacerated skin. Pregnant woman can pass the virus to her baby during childbirth.
Elzatein-Barn Virus
Elzatein-Barn virus is also known as human herpes virus, commonly infecting the human oropharyngeal epithelial cells and B lymphocytes.
3.1.2.3 Fungus
Pneumocystis Carinii
Pneumocystis carinii had been thought to be a protozoan. Recently, scholars consider it to be a fungus. In its life history, it survives in lungs in two forms, sporozoites and trophozoites.
Candida Albicans
Candida albicans is commonly found in oral cavity of healthy population and is an opportunistic pathogen. It can invade many parts of the human body, including skin, mucous membrane, internal organs and central nervous system.
Cryptococcus
Cryptococcus is also known as torula histolytica, the saprophytes of the soil, pigeons, cow milk, and fruits. It can also survive in human mouth and is an opportunistic pathogen.
3.1.3 Pathogenicity of Pathogenic Microorganisms
The opportunistic infections are caused by conditional pathogenic factors, which cannot cause diseases when human immunity is normal due to their low pathogenicity. However, when the human immunity is compromised, these pathogenic microorganisms have a conditional opportunity to invade human body, causing diseases that are known as opportunistic infections. Therefore, opportunistic infections occur in the special physical situation of the AIDS patients. In fact, opportunistic infections are the major cause of death in AIDS patients. Findings by autopsy indicated that 90 % AIDS patients die from opportunistic infections. The following elaborates the pathogenicity of protozoa, viruses, fungi and bacteria.
3.1.3.1 Protozoa
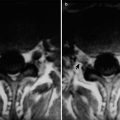
Toxoplasma Infection
The AIDS patients with toxoplasmosis infection are commonly toxoplasmosis of the nervous system, with an incidence of 26 %. Its clinical manifestations are paralysis, focal neurological abnormalities, convulsions, disturbance of consciousness and fever. CT scanning demonstrated singular or multiple focal lesions. Examinations of histopathological sections or cerebrospinal fluid can find toxoplasma gondii. It is rare (incidence of about 1 %) to find toxoplasmosis with lungs involved.
Cryptosporidiosis
Cryptosporidium is a small protozoan parasitizing in domestic or wild animals. Its invasion of human by attaching to epithelial cells in the small intestine and colon causes malabsorptional diarrhea. The patients sustain large quantities of uncontrollable watery stools, more than 5–10 times daily. And their daily water loss can be up to 3–10 L. The death rate from it is as high as above 50 %. Its diagnosis can be defined by colonoscopic biopsy or by stool examination to find protozoan oocysts.
3.1.3.2 Viruses
Cytomegalovirus Infections
AIDS related cytomegalovirus infection commonly has clinical manifestations of hepatitis, cytomegalovirus pneumonia, cytomegalovirus retinitis, thrombocytopenia and leukopenia, skin rash. Its diagnosis can be defined by finding the inclusion bodies or isolating the virus in biopsy or autopsy specimens. According to autopsy by Guarda et al. on 13 cases of AIDS, the most common diagnosis is cytomegalovirus infections (12 cases), followed by Kaposi’s sarcoma (10 cases). Cytomegalovirus infection in all 12 cases is disseminative, with 2 or more organs involved.
Herpes Simplex Virus Infections
Herpes simplex virus infection causes impaired skin and mucous membrane in AIDS patients, with perioral, external vaginal, perianal, back of the hand, esophageal, bronchial mucosa and intestinal mucosa involved. The most common is herpes simplex in lip margin and corner of the mouth. The lesion is a highly dense cluster of small blisters, with a slightly red base. Ulcer usually occurs after blisters scraped. The ulcers are large and deep with pain, accompanied by secondary infection. The symptoms are mostly severe, with a long-term progression. Tissues from the lesion can be cultured to find the herpes simplex virus. By biopsy, typical inclusion bodies can be found.
3.1.3.3 Fungi
Pneumocystis (Carinii) Pneumonia
Studies have proved that PCP is a fungal infection, instead of a protozoan infections. Until now, it is sometimes called as pneumocystis carinii in some documents and literatures. PCP is transmitted via respiratory tract, specifically via air and droplets. After healthy people are infected by HIV, their immunities are compromised. As a result, pneumocystis (carinii) obtains its conditional opportunity to invade human body and there to multiply itself in large amount. The alveoli are filled with exudates and various pneumocystis carinii, resulting in serious damage to the lungs. PCP is a common cause of death in AIDS patients and is the most serious opportunistic infection in more than 60 % AIDS patients. PCP occurs in about 80 % AIDS patients at least once. AIDS related PCP initially has clinical symptoms of progressive malnutrition, fever, general upset, weight loss and lymphadenectasis, followed by cough, difficulty breathing and chest pain. The whole progression lasts about 4–6 weeks. Signs of fever (89 %) and shortness of breath (66 %) are the most commonly found concerning the respiratory system, with lungs rales heard in some patients. PCP is frequently recurrent and serious, being a common cause of death in AIDS patients. The chest X-ray for patients with PCP found extensive infiltration of both lungs. But the chest X-ray of a few patients (about 23 %) may be normal or close to normal. The progression of PCP is acute, sometimes chronic, ended by death from respiratory failure due to progressive difficulty breathing and hypoxia. The death rate from PCP is up to 90–100 %.
Candidal Infection
Candida albicans is an opportunistic pathogenic fungus. When the defense system is weak or dysbacteriosis occurs, candida albicans is pathogenic, leading to candidal infection. Candidal infections can be categorized into cutaneous candidiasis and mucosal candidiasis. The later is commonly specified as thrush, a milky white coating on the oral mucosa, tongue and throat, gums or lips mucosa. The coating is susceptible to peeling off with exposure of its fresh and moist red base. Candidal infection is common in the advanced stage of serious diseases or in HIV-infected patients. For homosexuals with persistent thrush of unknown reasons, it is an indicator of HIV infection or progression into AIDS. Candida esophagitis causes swallowing difficulty and pain, or retrosternal pain. By esophagoscopy, irregular ulcers and white pseudomembrane can be found in esophageal mucosa. Other candida infections include candidal angular cheilitis, candidal vaginitis, candidal balanoposthitis, and organ candidal infection. The diagnosis of skin and mucosal candidiasis depends on clinical manifestations and laboratory tests on fungi.
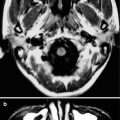
Cryptococcosis
Cryptococcosis is an acute or chronic deep mycosis caused by cryptococcus neoformans infection. When the immune defense is weak, cryptococcus obtains chances to invade the human body via the respiratory tract, occasionally via the intestine or skin, leading to diseases. Cryptococcal meningitis is a common complication of AIDS, with a high death rate. The clinical manifestations include fever, headache, insanity, and meningeal irritation. Pulmonary cryptococcosis is subacute or chronic, with accompanying cough, thick phlegm, low grade fever, chest pain and fatigue. Chest X-ray findings are non-specific. And its diagnosis can be defined by clinical manifestations and laboratory tests on fungi.
3.1.3.4 Bacteria
Mycobacterium Tuberculosis
Tuberculosis often occurs in patients with HIV infection but no progression into AIDS. Its occurrence may probably due to the stronger virulence of mycobacterium tuberculosis than other AIDS-related opportunistic pathogens, such as pneumocystis carinii. Thus, tuberculosis is more likely to occur in early stage of immunodeficiency. In HIV infected patients with tuberculosis, 74–100 % substain pulmonary tuberculosis, whose signs and symptoms are often difficult to be differentiated from those of other AIDS-related lung diseases. AIDS patients usually have disseminative infections. The characteristic clinical finding of HIV-infected patients with concurrent tuberculosis is the high incidence of extrapulmonary tuberculosis, being up to 70 %. The most common findings of AIDS with extrapulmonary tuberculosis are lymphadenitis and miliary lesions, with involvements of bone marrow, genitourinary tract and central nervous system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree