(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
22.2.1 Pathogen and Pathogenesis
22.2.2 Pathophysiological Basis
22.2.3 Clinical Symptoms and Signs
22.2.5 Imaging Demonstrations
22.2.6 Diagnostic Basis
22.2.7 Differential Diagnosis
22.3.1 Pathogen and Pathogenesis
22.3.2 Pathophysiological Basis
22.3.3 Clinical Symptoms and Signs
22.3.5 Imaging Demonstrations
22.3.6 Discussion
22.3.7 Diagnostic Basis
22.3.8 Differential Diagnosis
22.4.1 Acute Renal Failure
22.4.2 Chronic Renal Failure
22.5.1 Pathogens and Pathogenesis
22.5.2 Pathophysiological Basis
22.5.3 Clinical Symptoms and Signs
22.5.5 Imaging Demonstrations
22.5.6 Diagnostic Basis
22.5.7 Differential Diagnosis
22.8.2 HIV/AIDS Related Renal Cyst
Abstract
HIV/AIDS may involve all of the systems and organs, including the urinary system. In HIV infected patients, about 30 % kidney dysfunctions. HIV infection can involve glomerulus, renal tubule, renal interstitium and blood vessels. HIV/AIDS related nephropathy (HIVAN) is the most common in the terminal stage of AIDS, which is the common reason for the end-stage renal failure (ESRF) and is related with the progression of AIDS and the occurrence of death. IgA nephropathy, heroin associated nephropathy and hypertensive nephropathy can also be found in AIDS patients. Opportunistic infections also involve kidneys. CMV infection is one of the most common opportunistic infections of kidney, accounting for about 12.8 %. It is believed to accelerate the development of HIVAN. Renal infection induced by fungal infections is likely to develop into intrarenal or perinephral abscesses, with possible concurrent involvements of the spleen and the liver. Usually, tuberculosis infection occurs prior to other opportunistic infections. Renal tuberculosis is a part of systemic TB. In cases of ARL, 6–12 % has the invaded kidney. KS is a commonly found renal neoplasm in AIDS patients. In the cases of HIV/AIDS related infections or cancer, 20–40 % has occurrence of acute kidney failure.
22.1 An Overview of HIV/AIDS Related Urogenital Diseases
HIV/AIDS may involve all of the systems and organs, including the urinary system. In HIV infected patients, about 30 % kidney dysfunctions. HIV infection can involve glomerulus, renal tubule, renal interstitium and blood vessels. HIV/AIDS related nephropathy (HIVAN) is the most common in the terminal stage of AIDS, which is the common reason for the end-stage renal failure (ESRF) and is related with the progression of AIDS and the occurrence of death. IgA nephropathy, heroin associated nephropathy and hypertensive nephropathy can also be found in AIDS patients. Opportunistic infections also involve kidneys. CMV infection is one of the most common opportunistic infections of kidney, accounting for about 12.8 %. It is believed to accelerate the development of HIVAN. Renal infection induced by fungal infections is likely to develop into intrarenal or perinephral abscesses, with possible concurrent involvements of the spleen and the liver. Usually, tuberculosis infection occurs prior to other opportunistic infections. Renal tuberculosis is a part of systemic TB. In cases of ARL, 6–12 % has the invaded kidney. KS is a commonly found renal neoplasm in AIDS patients. In the cases of HIV/AIDS related infections or cancer, 20–40 % has occurrence of acute kidney failure.
The invasion of HIV/AIDS to the reproductive system can cause diseases including HIV/AIDS related opportunistic infections and neoplasms. Of all the infective diseases, infections of Cryptococcus and CMV are more common. Of neoplastic diseases, KS is more common. In female patients, HIV infection has certain correlationship with the occurrence of cervical carcinoma.
22.2 HIV/AIDS Related Nephropathy
HIV/AIDS related nephropathy (HIVAN) is the leading cause for HIV/AIDS related renal diseases. HIVAN tends to occur in certain races and 90 % HIVAN patients are the black people. In the etiological factors for ESRF in the black people aged 20–64 years, HIVAN ranks the third. The prognosis of HIVAN is determined by the HIV infection instead of the kidneys. The diagnosis of HIVAN is the indicator of the advanced HIV infection.
22.2.1 Pathogen and Pathogenesis
Currently, the pathogenesis of HIVAN is still unknown, which is possibly related to the following factors: (1) direct infection of HIV to the kidney parenchymal cells, and then invasion of the renal epithelial cells including visceral epithelial cells and tubular epithelial cells; (2) indirect renal lesions after the coding products of HIV in the blood circulation being absorbed by renal cells; (3) indirect renal lesions caused by the cytokines released from HIV infected lymphocytes and mononuclear cells in the kidney. In addition, it may also be related to gene and environmental factors.
22.2.2 Pathophysiological Basis
The pathologic changes of HIVAN are characteristic, mainly including enlarged kidney volume, proliferation of epithelial cells, the whole or segmental contraction and collapse of the glomerular capillary wall with obvious podocyte proliteration, apoptosis in the glomerulus and renal interstitium. By light microscopy, the findings of whole collapse of any one glomerulus or segmental collapse in more than 20 % glomerulus should be suspected as the disease. Under an electron microscope, large quantity tubuloreticular inclusion bodies (in 80–90 % HIVAN patients) in endothelial cells and interstitial leukocytes of the glomerulus can facilitate to define the diagnosis.
22.2.3 Clinical Symptoms and Signs
Including serious albuminuria (above 3.5 g/day), azotemia, water electrolyte imbalance, hematuria by naked eyes, normal blood pressure, normal/enlarged kidney, acute progressive renal dysfunction. The normal blood pressure is characteristically HIVAN.
22.2.4 Examinations and Their Selection
22.2.4.1 Laboratory Tests
The urine precipitation examination demonstrates serious albuminuria (above 3.5 g/day), oval liposome and lipuria. A large quantity huge waxy casts is characteristically HIVAN.
22.2.4.2 CT Scanning and Ultrasound
The demonstrations are non-specific, with main manifestations of normal/enlarged kidney volume.
22.2.5 Imaging Demonstrations
22.2.5.1 CT Scanning
CT scanning demonstrates enlarged kidney volume. Plain CT scanning can occasionally demonstrate increased density of the kidney medulla, which may be caused by abnormalities of the renal tubule in the cases of HIVAN. Enhanced scanning demonstrates the kidney with stripes of enhancement.
22.2.5.2 Ultrasound
It demonstrates normal/enlarged kidney volume, with unclearly defined cortex and medulla. These demonstrations may be caused by focal/segmental sclerosis of glomerulus, and tubular dilation filled by protein casts. But echoes demonstrated by ultrasound fail to directly show the severity of renal lesions.
22.2.6 Diagnostic Basis
In the advanced stage of HIV infection, albuminuria occurs (being higher than 1 g/24 h), with increased creatinine. By the diagnostic imaging, the kidney is found enlarged and renal failure with other etiologic factors excluded. The cases with no typical clinical manifestations or ineffective treatment by antiretroviral therapy or other therapies should be performed kidney tissues biopsy to define the diagnosis.
22.2.7 Differential Diagnosis
22.2.7.1 IgA Nephropathy
It is commonly found in white people, with manifestations of hematuria by naked eyes or microscopy, slight/moderate renal dysfunction, albuminuria lower than 1 g/24 h, and a slow progression. Pathologically, it shows mesangium proliferation and IgA deposits. In some patients, interstitial inflammation occurs.
22.2.7.2 Heroin Associated Nephropathy
It has common manifestations of albuminuria and hypertension. By ultrasound, it is demonstrated to have decreased kidney volume. The process into end-stage renal disease is much slower than that of HIVAN (for 1–4 months). The renal tissues biopsy can facilitate the differential diagnosis.
22.3 HIV/AIDS Related Urogenital Tuberculosis
TB is the most common opportunistic infection of HIV/AIDS and extrapulmonary tuberculosis is more common. TB of urogenital system is one of the common extrapulmonary tuberculosis.
22.3.1 Pathogen and Pathogenesis
Almost all cases of renal tuberculosis occur secondary to pulmonary tuberculosis, and occasionally secondary to joint tuberculosis, lymphaden tuberculosis and intestinal tuberculosis. The invasion of tubercle bacilli to the kidneys is via 4 routes, blood, urinary tract, lymphatic vessel and direct extension. Blood borne spreading to the kidneys is recognized as the most common transmission route. Blood borne infection of renal TB is mostly simultaneous infections of both kidneys. However, in its progressive process, the severity of renal TB may be more serious in one kidney than the other. Due to the compromised immunity, the conditions may develop rapidly, with possible serious lesions in both kidneys. Pathological examinations have demonstrated that more than 80 % cases have simultaneous infection of both kidneys. But actually, the contralateral lesions are slight and can be self healed. Therefore, the clinical cases of renal TB is mostly unilateral, accounting for about 85 % and the cases of bilateral renal TB account for about 10 %.
Ureter tuberculosis is caused by downward spreading of the homolateral renal tuberculosis. And it can also be caused by the urinary reflux of mycobacterium tuberculosis in the bladder for the retrograde infection.
About 50–70 % of male patients with renal tuberculosis sustain the complication of reproductive system tuberculosis. Its occurrence in males originates from the prostate and the seminal vesicle. The condition with the most obvious clinical symptoms is epididymis TB. In the patients with renal TB complicated by reproductive TB, about 40 % have their epididymis tuberculosis occurring before or during the occurrence of renal tuberculosis.
22.3.2 Pathophysiological Basis
Along with the blood flow, mycobacterium tuberculosis invades the kidney to cause lesions, of which 90 % are located in the cortex and 10 % in the medulla. Cortex tuberculosis infection is self healing. However, in the cases with further progression, the medulla may be involved to form caseous necrosis and tuberculous abscesses. The abscess can penetrate into the kidney calices to cause cavities after the necrotic materials being discharged. The abscess rupture and access of mycobacterium tuberculosis into the urine via the tubules can cause mucosa lesions and ulceration in the kidney calices and pelvis. Subsequently, due to the formation of tuberculous granulation tissue, stenosis of the kidney calices and pelvis occurs with their wall thickened. Calyceal stenosis can cause the infection to involve the other kidney calices and further invade the adjacent renal parenchyma. The primary lesions in the renal parenchyma can also gradually enlarge to cause extensive lesions in the renal parenchyma to form multiple cavities. Therefore, tuberculous pyonephrosis occurs. This type is the most commonly found in the clinical practice. In some patients, if the compromised immunity improves, caseous materials thus are concentrated rather than liquefaction to cause extensive fibrous tissues hyperplasia and calcification, which is known as autonephrectomy or plaster kidney. Although the disease may clinically progress to calcified autonephrectomy, the actual pathological changes are caseous cavities, fibrous atrophy, and mixed hard nodules and calcification. Tubercle bacilli can still exist in the caseous substances.
Ureter tuberculosis often invades the ureteral mucosa, mucosal lamina propria and muscularis. In the early stage, ureteral mucosa is damaged, which leads to ulceration and lumen dilation. Subsequently, due to the formation of tuberculous granulation tissues, the ureteral wall is thickened and rigid, with stenosis and even occlusion. Urethral stenosis commonly occurs most commonly at the ureterovesical junction, followed by the ureteropelvic junction. Its occurrence at the middle segment is rare. The involved ureter can be partially or totally calcified.
Bladder tuberculosis is commonly caused by spreading of renal or ureteral tuberculosis. In the early stage, it is demonstrated to have bladder mucosal congestion, edema, irregular ulcers and (or) granuloma. The lesion begins adjacent to the ipsilateral ureteral opening, and then spreads to other parts to involve the delta or even the whole bladder. In the advanced stage, the lesions invade into the myometrium to cause serious fibroplastic proliferation and scar contraction, resulting in the shrinkage of the bladder capacity to less than 50 ml. It is known as bladder contracture. Bladder fibroplastic proliferation can cause ureteral stenosis or ureteral incompetence to form cave liked lesions. Both can lead to obstruction and urine reflux in the ureters, resulting in hydronephrosis. Ureteral incompetence also allows urine in the bladder flowing upwards to infect the contralateral kidney. In the cases of serious bladder lesions and deep ulceration, the bladder wall can be penetrated to involve the vagina or the rectum, resulting in vesico-vaginal fistula or vesico-rectal fistula.
The main pathological changes of urethral tuberculosis are ulcer and stenosis, which can cause dysuresia and urinary fistula and aggravate the kidney dysfunction.
22.3.3 Clinical Symptoms and Signs
The patients with renal tuberculosis commonly sustain the symptoms of urgent urination, frequent urination, painful urination and other bladder irritation symptoms, with accompanying hematuria, pyuria, backache, anemia, low grade fever, night sweating, poor appetite, weight loss, fatigue and other systemic symptoms.
22.3.4 Examinations and Their Selection
1.
Routine urine test provides important clues for the early screening of renal tuberculosis.
2.
Urinary tubercle bacilli culture is an important basis for the diagnosis of renal tuberculosis. It also monitors the drug resistance to tubercle bacilli.
3.
Immunological assays of ELISA detects tubercle bacilli antibody for the diagnosis of renal tuberculosis, which has a coincidence rate of 82 % with the pathological examinations. It is the most important examination for the diagnosis of renal tuberculosis.
4.
Intravenous urography (IVP) can demonstrate the calyx erosion and deformation and tuberculous abscesses of early renal tuberculosis. It can also demonstrate the general view of hydronephrosis caused by calyx and/or pelvic stenosis. Therefore, it is the examination of the choice for the early diagnosis of renal tuberculosis.
5.
Percutaneous kidney puncture is an important method for the diagnosis. Especially for the nonfunctional kidney that fails to be demonstrated by IVP, it can be favorably applied for the understanding of the condition above obstructed urinary passage.
6.
Ultrasound is of less significance for the early diagnosis of renal tuberculosis. However, for the cases with cavities or hydronephrosis, it is of great assistance.
7.
CT scanning is less favorable than IVP in demonstrating the early lesions. However, it can well demonstrate the calcification, thickened ureteral wall, renal functional assessment and severity of perinephral lesions, which is optimal for the examination of these lesions.
8.
MR imaging is not the conventional imaging examination for the diagnosis of urinary tuberculosis. But for the cases with failed demonstration by pyelography or unfavorable conditions for enhanced CT scanning, MR imaging can define the diagnosis.
9.
Cystoscopy is an important examination for the diagnosis of urinary tuberculosis.
22.3.5 Imaging Demonstrations
22.3.5.1 Renal Tuberculosis
Ultrasound demonstrates early renal TB as echo free areas from the kidney parenchyma, with fine small spots or patchy echoes. The advanced renal TB is demonstrated as hydronephrosis, with spots echoes in it. For the cases with calcification, the lesions are demonstrated with strong echo patches and posterior sound shadows. Tuberculous abscesses are demonstrated as low echo. CT scanning demonstrates focal low density lesions in the kidneys, liver and the spleen, with abdominal lymphadenectasis and decreased density areas in it. Tuberculous abscesses are demonstrated as low density. MR imaging is sensitive to early infiltrative foci of intrarenal tuberculosis, with focal or diffuse long T1 and long T2 signals. With the progression of the conditions, necrosis of the caseous lesion tissues occur to form cavities, with long T1 and long T2 signals of the cavities as well as equal T1, equal/short T2 signals of the cavity walls. When the lesions penetrate the kidney capsule, there are signal changes of perirenal adipose layer, with thickened perirenal fascia.
22.3.5.2 Ureteral Tuberculosis
CT scanning demonstrates no abnormalities or slight dilation of the ureter. In its advanced stage, the ureteral wall is thickened, with multiple irregular stenosis and dilation of the lumen, which can involve the whole ureter. MR imaging demonstrates unfavorably ureteral tuberculosis, sometimes with demonstrations of thickened ureteral wall and peripheral exudations.
22.3.5.3 Bladder Tuberculosis
Ultrasound demonstrates no early abnormalities. After the occurrence of diffuse fibrosis, the bladder wall can be found thickened. In the cases with their urine containing pus, blood and tissue fragments, fin spots echoes can be found. CT scanning demonstrates irregular inner layer of the bladder wall, thickened bladder wall and shrinkage of bladder lumen. MR imaging has similar demonstrations to CT scanning.
Case Study 1
A female patient aged 47 years was confirmatively diagnosed as having AIDS by the CDC. She had a history of paid blood donation in the year of 1994 and sustained symptoms in 2008 of low grade fever, night sweating and weight loss. The urine test demonstrated tubercle baccili positive and his CD4 T cell count was 88/μl.
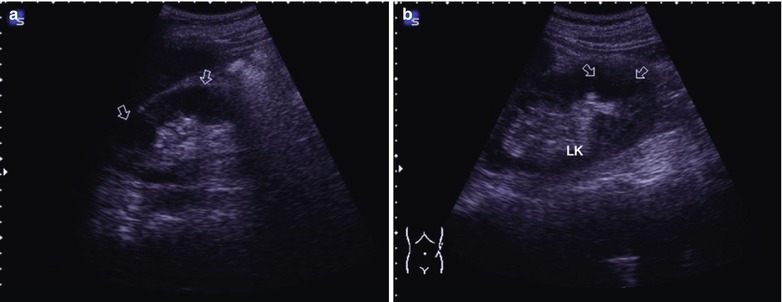
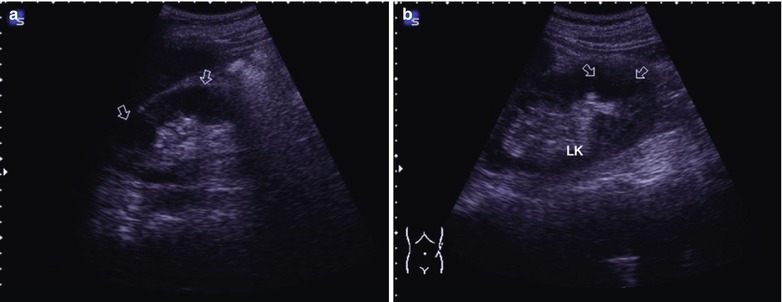
Fig. 22.1
(a, b) HIV/AIDS related renal tuberculosis. (a, b) Color Doppler demonstrates normal kidney size, unsmooth capsule, uneven echo from the renal parenchyma with multiple irregular low echo areas (arrows), unclear boundary and uneven internal echo. CDFI demonstrates unobvious internal blood flow signal. LK left kidney
Case Study 2
A male patient aged 41 years was confirmatively diagnosed as having AIDS by the CDC. He sustained symptoms in 2008 of frequent urination, and bloody urine found by naked eyes. The urine test found tubercle baccili positive. His CD4 T cell count was 67/μl.
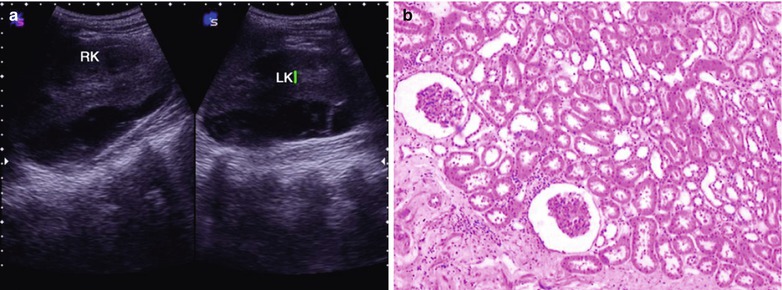
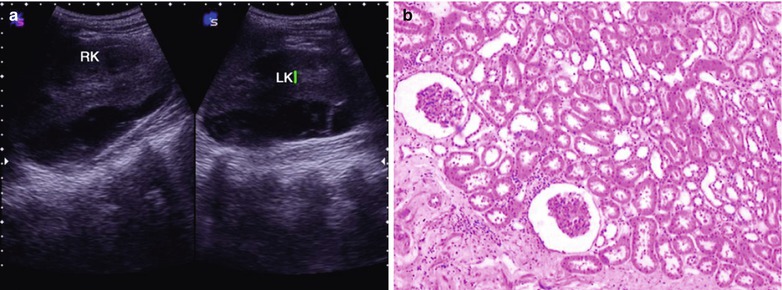
Fig. 22.2
HIV/AIDS related renal tuberculosis. (a) Color Doppler demonstrates normal kidney size, smooth capsule, uneven echo from the renal parenchyma with multiple irregular low echo, unclear boundary and uneven internal echoes. CDFI demonstrates unobvious internal blood flow signal. (b) Microscopy at a low magnification demonstrates chronic inflammatory cell infiltration in the renal cortex. LK left kidney, RK right kidney
Case Study 3
A male patient aged 36 years was confirmatively diagnosed as having AIDS by the CDC. He complained in 2008 of frequent urination, left lower back pain for 6 months. The urine test demonstrated tubercle baccili positive and his CD4 T cell count was 71/μl.


Fig. 22.3
HIV/AIDS related renal tuberculosis. Color Doppler demonstrates normal kidney, tough capsule, uneven echo from the renal parenchyma. An irregular shaped low echo area in size of 22 × 23 mm can be found in the right lower kidney (arrows), with unclear boundary and mixed internal echoes. CDFI demonstrates unobvious internal blood flow signal. The left renal collecting system is separated a width of 18 mm. LK left kidney, RK right kidney, RL right liver
22.3.6 Discussion
Due to their compromised immunity, AIDS patients are susceptible to renal tuberculosis, which is the most common and earliest urinary TB. It can spread from the kidney to involve the whole urinary system. Therefore, renal tuberculosis actually represents urinary tuberculosis.
Renal tuberculosis occurs commonly in age group of 20–40 years old-old, accounting for 70 %. The male patients are more than female patients, with a ratio of 2:1. About 80 % cases of renal tuberculosis are unilateral, with similar lesions in the left and right kidney.
Renal tuberculosis commonly originates from pulmonary tuberculosis, and rarely from bone and joint tuberculosis. Tubercle bacilli disseminate from the primary lesions to the renal cortex along with the blood flow to form multiple micro-TB lesions. When the defense system is weakened, it progresses into renal medullary tuberculosis, which is the clinical renal TB.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree