(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
6.3.1 Acute Stage
6.3.2 Asymptomatic Stage
6.3.3 AIDS Stage
6.4.1 Pulmonary Type
6.4.2 Central Nervous Type
6.4.3 Gastrointestinal Type
6.4.4 Fever of Unknown Causes
6.4.5 Neoplasm Type
Abstract
After successful invasion of HIV into the human body, HIV antibody occurs within 4–8 weeks, followed by its incubation period lasting 2–10 years. During this period, HIV still replicates incessantly to compromise the immune system, with gradually decreasing CD4 T lymphocytes and infectivity. Even though the patients show no clinical symptoms, they, as HIV carriers, can spread the virus via various transmission routes.
Keywords
Clinical Symptoms and SignsClinical ClassificationDiagnostic Criteria and Treatment Guideline for HIV/AIDS6.1 Incubation Period
After successful invasion of HIV into the human body, HIV antibody occurs within 4–8 weeks, followed by its incubation period lasting 2–10 years. During this period, HIV still replicates incessantly to compromise the immune system, with gradually decreasing CD4 T lymphocytes and infectivity. Even though the patients show no clinical symptoms, they, as HIV carriers, can spread the virus via various transmission routes.
6.2 Clinical Characteristics
The progression of HIV infection is a long-term natural developing process. The patients’ survival duration depends on the quantity of HIV in the body, individual health difference, nutritional status and the effectiveness of the therapies. HIV induces exhaustion and death of T cells, which is demonstrated by decreased CD 4T lymphocytes count. Clinically, the progression of HIV infection can be divided into three stages, namely acute stage, asymptomatic stage and AIDS stage.
6.3 Clinical Symptoms and Signs
6.3.1 Acute Stage
After preliminary HIV infection, the HIV infection progresses into acute stage in 2–4 weeks. Some patients show symptoms of HIV related viraemia and acute immunity impairment. Most patients have slight clinical symptoms that are relieved after 1–3 weeks. The most commonly found symptom is fever, with accompanying sore throat, muscle pain, headache, nausea, vomiting, skin rash, thrush, arthralgia, splenohepatomegaly, enlarged lymph nodes, weight loss and nervous system symptoms. Some patients may also have slight leukocytopenia, thrombocytopenia or liver malfunction.
6.3.2 Asymptomatic Stage
During the stage, no clinical manifestation can be found, while 40–60 % patients may have specific lymphadenectasis, predominantly axillar lymph nodes. The persistent general lymphadenectasis is defined as the following:
1.
Lymphadenectasis occurs in at least two parts of the body in addition to groin;
2.
Lymph node is larger than 1 cm in diameter, with no tenderness and adhesion;
3.
Lymphadenectasis lasts at least 3 months;
4.
Exclusion of other etiologic factors.
6.3.3 AIDS Stage
AIDS stage is the final stage of HIV infection. The patients usually have obviously decreased CD4 T lymphocytes count of lower than 200/μl, obviously increased HIV virus load in plasma. During this period, the clinical manifestations include HIV-related symptoms, various opportunistic infections and neoplasms.
1.
Persistent irregular fever of above 38 °C for more than 1 month, with no cause found;
2.
Diarrhea (bowel movement more than three times daily), persistent more than 1 month;
3.
Weight loss over 10 % in 6 months;
4.
Recurrent attacks of oral candidiasis albicans;
5.
Recurrent attacks of herpes simplex virus infection or herpes zoster virus infection;
6.
Pneumocystis pneumonia (PCP);
7.
Recurrent bacterial pneumonia;
8.
Active tuberculosis or nontuberculous mycobacteria;
9.
Deep fungal infections;
10.
HIV-related dementia;
11.
Progressive multifocal leukoencephalopathy;
12.
Active cytomegalovirus infection;
13.
Cerebral toxoplasmosis;
14.
Penicillium infection;
15.
Recurrent septicemia;
16.
Kaposi’s sarcoma and lymphoma in skin mucus and organs;
17.
Chronic isosporiasis;
18.
Coccidioidomycosis and histoplasmosis;
19.
Invasive cervical cancer.
6.4 Clinical Classification
According to the clinical manifestations, AIDS can be divided into the following five types:
6.4.1 Pulmonary Type
Pulmonary type is the most common type of AIDS, with symptoms of dyspnea, hypoxemia and chest pain. Chest X-ray demonstrates pulmonary diffusive infiltration and decreased pulmonary functions. The most common deadly infection is pneumocystis pneumonia (PCP).
6.4.2 Central Nervous Type
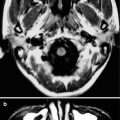
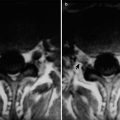
Central nervous type can be found in 30 % patients with AIDS. HIV itself can attack brain issue to cause encephalitis liked symptoms. Toxoplasma gondii and cryptococcus can attack central nervous system to cause cerebral abscess, diffusive encephalitis and encephalomeningitis. The symptoms include headache, vomiting, consciousness impairments, spasm, dementia and relevant symptoms of space-occupying lesions. The diagnosis can be defined by cerebrospinal fluid smear and culture as well as brain CT scanning.
6.4.3 Gastrointestinal Type
Patients with gastrointestinal type AIDS have diarrhea and weight loss. For serious cases, the symptoms also include malabsorption and cachexia. Cryptozoite infection is the common cause of AIDS related gastrointestinal infection, with symptoms of chronic diarrhea and watery stool for months. It is also the common cause of death in patients with AIDS. Infections of other pathogens, such as cytomegalovirus, salmonella, bacillus dysenteriae and Amoeba trophozoite, also contribute to symptoms of enteritis including diarrhea, abdominal pain, tenesmus, purulent and bloody stool and malabsorption. Candida albicans caused esophagitis and glossitis can be definitively diagnosed by gastroscopy.
6.4.4 Fever of Unknown Causes
Due to infection of pathogens, high fever, upset, fatigue and general lymphadenectasis occur.
6.4.5 Neoplasm Type
Kaposi’s sarcoma is the most common AIDS related neoplasm, with no discoloration under finger pressure but tawny ecchymosis surrounding it and rapid progression. The skin lesions can be found in face and neck, spreading to oral cavity, lungs and alimentary tract, to cause bleeding and death. Pathological biopsy can be applied for definitive diagnosis. Other malignant neoplasms include lymphoma, liver carcinoma, and pulmonary squamous cell carcinoma.
6.5 Characteristics of Children with HIV/AIDS
Most clinical manifestations of children with AIDS are similar to those of adult patients, except that lymph nodes lesions, Kaposi’s sarcoma and opportunistic infections do not occur in children with AIDS. Almost all children with AIDS sustain splenohepatomegaly, interstitial pneumonia and developmental impairments. After HIV infection, children have a shorter incubation period but fast progression. Both the survival rate and clinical manifestations are correlated with age. About 50 % children with AIDS survive 12 months after their definitive diagnosis. The 1 year survival rate of children suffering from PCP and being younger than 12-month-old is only 30 %. The 1 year survival rate of elder children with PCP is 48 %. The 1 year survival rate of elder children with other AIDS related diseases is 72 %. The characteristic clinical manifestations occur in early childhood. PCP, HIV wasting syndrome and encephalopathy occur in children aged 4–8 months. Concerning opportunistic infections, children patients are different from adult patients in occurrence of bacterial infections and Kaposi’s sarcoma. Children with AIDS have a higher occurrence of bacterial infections, such as otitis media, encephalomeningitis and pneumonia, but a rare occurrence of Kaposi’s sarcoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree