(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
14.1.4 HIV/AIDS Related Myeloma
14.2.1 Pathogen and Pathogenesis
14.2.2 Pathophysiological Basis
14.2.3 Clinical Symptoms and Signs
14.2.5 Imaging Demonstrations
14.2.6 Criteria for the Diagnosis
14.2.7 Differential Diagnosis
14.5.1 Pathogen and Pathogenesis
14.5.2 Pathophysiological Basis
14.5.3 Clinical Symptoms and Signs
14.5.5 Imaging Demonstrations
14.5.6 Criteria for the Diagnosis
14.5.7 Differential Diagnosis
14.6.1 Pathogen and Pathogenesis
14.6.2 Pathophysiological Basis
14.6.3 Clinical Symptoms and Signs
14.6.5 Imaging Demonstrations
14.6.6 Criteria for the Diagnosis
14.6.7 Differential Diagnosis
14.7.4 Compound Mononeuritis
14.7.6 Multiple Mononeuropathy
Abstract
Up to now, reports about HIV/AIDS related myelopathy remain rare in China. McArthur collected 186 cases of HIV/AIDS complicated by brain and peripheral nerve lesions in the year of 1987 [11]. Only 13 cases had HIV/AIDS related myelopathy, accounting for 7 %. Levy et al. [8] reported the occurrence of HIV/AIDS related myelopathy is 2–22 % based on literature analysis. In another group of 150 patients with AIDS, 42 had HIV/AIDS related myelopathy, in which 24 % with spinal degeneration, 38 % with viral infection, 5 % with toxoplasmosis, 2 % with myelitis and the other 31 % with no pathological diagnosis [2]. Surprisingly, myelopathy is commonly found by autopsy. Peter and his fellow researchers [14] found 50 % of the total 178 patients with AIDS have myelopathy, with 29 % spinal degeneration, 5 % HIV myelitis, 8 % viral infection, 7 % other infections and 2 % lymphoma. Budka [3] retrospectively reviewed autopsies of 475 death cases from AIDS in 1997 and found that 22.5 % had spinal degeneration, 6 % myelitis, 58 % viral infection and 4.1 % fungal, bacterial and protozoal infections as well as 2.3 % lymphoma. Since the year of 1997, knowledge about the clinical treatment for HIV/AIDS complicated by myelopathy has been greatly improved.
14.1 Introduction of HIV/AIDS Related Myelopathy and Peripheral Neuropathy
Up to now, reports about HIV/AIDS related myelopathy remain rare in China. McArthur collected 186 cases of HIV/AIDS complicated by brain and peripheral nerve lesions in the year of 1987 [11]. Only 13 cases had HIV/AIDS related myelopathy, accounting for 7 %. Levy et al. [8] reported the occurrence of HIV/AIDS related myelopathy is 2–22 % based on literature analysis. In another group of 150 patients with AIDS, 42 had HIV/AIDS related myelopathy, in which 24 % with spinal degeneration, 38 % with viral infection, 5 % with toxoplasmosis, 2 % with myelitis and the other 31 % with no pathological diagnosis [2]. Surprisingly, myelopathy is commonly found by autopsy. Peter and his fellow researchers [14] found 50 % of the total 178 patients with AIDS have myelopathy, with 29 % spinal degeneration, 5 % HIV myelitis, 8 % viral infection, 7 % other infections and 2 % lymphoma. Budka [3] retrospectively reviewed autopsies of 475 death cases from AIDS in 1997 and found that 22.5 % had spinal degeneration, 6 % myelitis, 58 % viral infection and 4.1 % fungal, bacterial and protozoal infections as well as 2.3 % lymphoma. Since the year of 1997, knowledge about the clinical treatment for HIV/AIDS complicated by myelopathy has been greatly improved.
HIV/AIDS related myelopathy had been rarely reported probably due to the difficulty in its differential diagnosis from encephalopathy based on the clinical manifestations and the difficulty in its diagnosis resulted from its complex lesions.
HIV infected patients commonly have complicated peripheral neuropathy, which is clinically manifested as neuropathic pain. Its incidence rate is much higher than myelopathy and the diagnosis rarely depends on the diagnostic imaging. In cases complicated by central nervous disorders, the clinical manifestations are complex. The diagnosis of cerebral and spinal lesions can be greatly facilitated by the diagnostic imaging.
In the year of 1985, Petito et al. [15] confirmed by pathological examinations that HIV/AIDS related spinal lesions are commonly accompanied by spinal degeneration, peripheral neuropathy and dementia and about 20 % have ataxia and sphincter impairments. Nevertheless, there still have no explicit diagnostic criteria. Due to the high degree of immunodeficiency in patients with AIDS, spinal lesions are commonly secondary rather than primary. Abnormal findings of myelopathy by the diagnostic imaging are usually demonstrated in the advanced stage of AIDS. The commonly seen HIV/AIDS complicated by myelopathy include viral myelitis, spinal bacterial infection and myeloma.
14.1.1 HIV/AIDS Related Spinal Toxoplasma Infection
Patients with AIDS are highly susceptible to toxoplasma infection, especially recurrence of latent infection. In such cases with acquired toxoplasmosis, lymphadenopathy may be less evident but acute fetal infections with extensive dissemination may occur. The clinical manifestations include high fever, pneumonia, skin rash, hepatosplenomegaly and myocarditis. Sometimes, spinal toxoplasmosis occurs as a complication of HIV/AIDS.
14.1.2 HIV/AIDS Related Viral Myelitis
Patients with AIDS can develop myelitic lesions induced by multiple viruses, such as cytomegalovirus (CMV), varicella zoster virus (VZV) and herpes simplex virus (HSV). It is commonly believed that the lesion is resulted from demyelination secondary to infection and is related to the autoimmunity. The foci can be found at any part of spinal white matter, with characteristic demonstrations of concurrent lesions around the veins and under the soft pia mater in the diseased white matter area. The lesion may involve the gray matter, with a diffusive distribution.
Viral myelitis has an acute onset, with initial clinical manifestations of fever, headache, nausea and vomiting 1–2 weeks prior to the onset. The following manifestations are anxiety, deliration, lethargy, stiffness and coma. The imaging demonstrations are not characteristic, making it difficult to be differentiated from acute multiple sclerosis. CT scanning demonstrates diffusive low-density area in the spinal white matter. MR imaging demonstrates swollen spinal cord, with equal or low signal of T1WI and high signal of T2WI. The focus is prone to be complicated by hemorrhage and swollen and enlarged spinal cords show no enhancement by enhanced imaging. In the chronic stage, the spinal cord may be shrunk and thin, with dilated central duct. However, the manifestations are not specific, making it difficult to be differentiated from lymphoma.
14.1.3 HIV/AIDS Related Spinal Bacterial Infection
HIV/AIDS complicated by spinal tuberculosis [4] and syphilis [12] have been reported. Tuberculosis mycobacterium can cause meningoradiculitis or intramedullary tuberculoma. Syphilis may cause syphiloma within the spinal canal. In patients with frequent intravenous drug abusers, bacteremia commonly occurs, with possible occurrence of epidural abscess that may extend to paravertebral. The most common pathogen of epidural abscess is staphylococcus; tuberculosis mycobacterium, Nocardia and Aspergillus [13] are also reported to cause high fever with progression to paralysis within 24–72 h. The lesion may be sub-acute, with nerve symptoms in 1 week or several months. Intramedullary infection is resulted from venous occlusion by bacteria colonies, leading to spinal venous occlusion. CT and MRI scanning can definitively demonstrate the location and range of the abscesses. Plain CT scanning demonstrates local spinal thickening, irregular morphology, and clearly defined boundary of intraspinal foci. The enhanced scanning shows ring shaped enhancement of the capsule. MRI demonstrates low signal of T1WI and T2WI of the capsule, low signal of T1WI and high signal of T2WI of the abscess fluid. The enhanced MR imaging demonstrates ring shaped enhancement of abscess wall by T1WI. Both CT and MRI demonstrate flaky or nodular enhancement before the formation of large abscess cavity at the inflammation phase.
14.1.4 HIV/AIDS Related Myeloma
Due to dependence on the immune response, patients with AIDS rarely have myeloma. The rarely found reports also include cases of spinal lymphoma and plasmocytoma. Lytic enzyme in the extraspinal Kaposi’s tumor (KS) can also impair the spinal cord. In HIV/AIDS related neoplasms, the accompanying spinal metastasis tumor may occur.
14.1.5 Other HIV/AIDS Related Diseases
HIV/AIDS related multiple sclerosis is related to HIV-induced immunodeficiency, with acute or sub-acute onset. Its initial symptoms include bilateral or unilateral visual impairment. Spinal cord lesions commonly occur in the dorsal horn, with clinical manifestations of limbs pain, paresthesia, weakness and paralysis of limbs or hemiplegia. Some patients may develop sensory disturbance, specifically sensing the plane as incomplete. Plain CT scanning demonstrations are negative; uneven ring shaped enhancement of the spinal cord in the acute phase can be found by enhanced scanning, with low sensitivity. Sagittal MR imaging demonstrates clearly the range of the lesions by T1WI and T2WI. In the acute phase, T1WI only demonstrates thickened spinal cord, with normal intraspinal signal; T2WI demonstrates intraspinal singular or multiple high signal foci, with space occupying effects of different degrees. By enhanced imaging, some foci are in ring shaped enhancement. Increased dosage of the contrast reagent can increase the detection rate of the foci.
Diagnostic examinations for HIV/AIDS related myelopathy include: For patients with spastic paralysis or paraplegia of the lower extremities, CSF test should be firstly performed to find the common pathogenic microorganisms and PCR can be performed to detect myelitis related viruses. For patients with large epidural abscess, lumbar puncture is of tremendous risk. CT scanning can effectively detect epidural lesions, but with poor demonstration of intraspinal lesions. MR imaging is ideal for clinical diagnosis of HIV/AIDS related myelopathy to distinguish epidural and subdural structures, demonstrate spinal degeneration, extensive necrosis and hemorrhage. When MR imaging is not available or feasible, enhanced CT scanning can facilitate the preliminary diagnosis.
14.2 HIV/AIDS Related Spinal Toxoplasma Infection
14.2.1 Pathogen and Pathogenesis
Toxoplasma invades the human body via the digestive tract. Firstly, sporozoites or trophozoites invade intestinal mucosal cells and reproduce there to cause the rupture of the intestinal mucosal cells. The released trophozoites are disseminated along with blood or lymph flow throughout the body to cause parasitemia. The further involvement of the spinal tissues renders toxoplasma rapidly divide and proliferate in tissue cells to cause damages to the host cells and invasion of their adjacent cells. The repeated pathogenic processes cause necrosis of local tissue cells to form necrotic foci and to induce acute inflammatory responses predominantly with monocytes infiltration.
14.2.2 Pathophysiological Basis
By autopsy, the spinal cord is found to have tissue liquification and necrosis, with few inflammatory cells infiltration. Within the necrotic foci, there are cystic toxoplasma trophozoites, as granules of different sizes.
14.2.3 Clinical Symptoms and Signs
Typical spinal toxoplasmosis has a sub-acute onset, with clinical manifestations of headache, hemiplegia, seizure, visual disturbance, unconsciousness and even coma. The symptoms of fever and meningeal irritation are rarely found.
14.2.4 Examinations and the Selection of Examinations
14.2.4.1 Examinations for Pathogens
Cerebrospinal fluid, sputum, pleural effusion, ascites and marrow are collected for smears. Alternatively, lymphnodeimprintslide and tissue sections may also be prepared. Subsequently routine staining or immunocytochemistry can be performed to detect toxoplasm trophozoites or cysts. Moreover, the toxoplasm can be isolated by inoculating the above specimens in mice or by tissue culture. In recent years, nucleic acid hybridization in situ or PCR has been used to examine toxoplasma DNA, which might facilitate diagnosis of toxoplasma infection. Especially, PCR examination of toxoplasma DNA in cerebrospinal fluid and amniotic fluid is of great significance for diagnosis of spinal toxoplasmosis and congenital spinal toxoplasmosis.
14.2.4.2 Immunological Assays
A widely used technology in recent years is to examine toxoplasma circulating antigen (CAg) in the serum or body fluid with specific antibody to toxoplasma. Toxoplasma CAg positive is an indicator of pathogen, facilitating the diagnosis of acute toxoplasma infection.
14.2.4.3 CSF Test
Cerebrospinal fluid (CSF) pressure is commonly normal, with yellowish appearance, positive globulin test and a slight increase in cell count, which is commonly (100–300) × 106/L and monocytes. The glucose level remains normal or decreased, with increased level of protein and normal level of chloride.
14.2.4.4 Diagnostic Imaging
MR imaging can clearly define the size, shape, location of the foci as well as their relationship with the adjacent tissues, which is of great importance to the diagnosis of cerebral toxoplasmosis and its outcomes.
14.2.5 Imaging Demonstrations
14.2.5.1 CT Scanning
The brain and spinal cord commonly have multiple foci. The plain CT scanning demonstrates thickened spinal cord, foci in equal or low signal, foci complicated by calcification in high signal, surrounding edema in strip liked low density foci, and ring liked and target shaped enhancement of foci by enhanced scanning.
14.2.5.2 MR Imaging
Plain MR imaging demonstrates thickened and swollen spinal cord, foci in short T1 and T2 signals, surrounding edema in long strip liked high T1 and T2 signals. By enhanced imaging, the foci are in ring shaped or target liked enhancement, highly indicative of spinal cord infection.
Case Study 1
A patient aged 36 years was confirmatively diagnosed as having AIDS by CDC, with positive toxoplasma IgG and a CD4 T cell count of 45/μl.


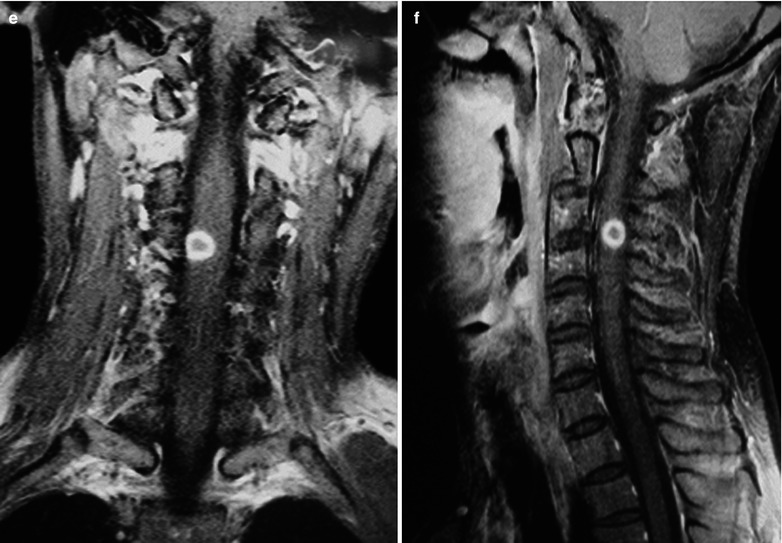
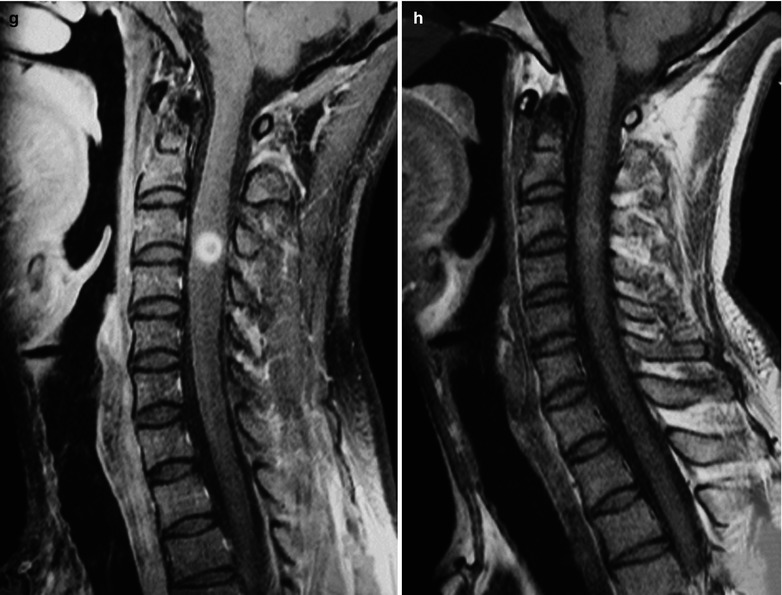
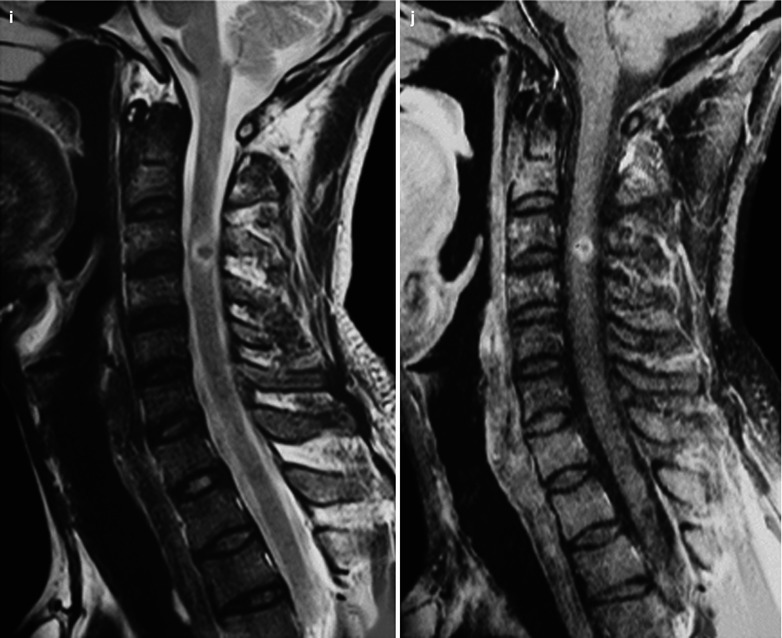


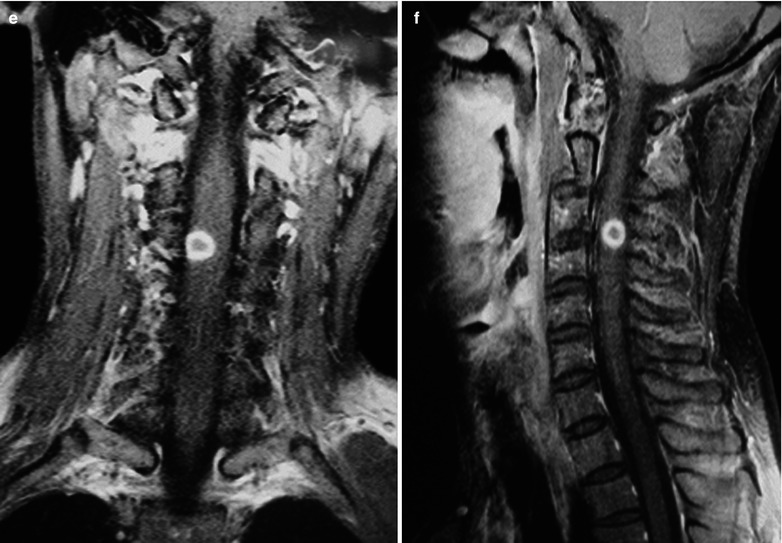
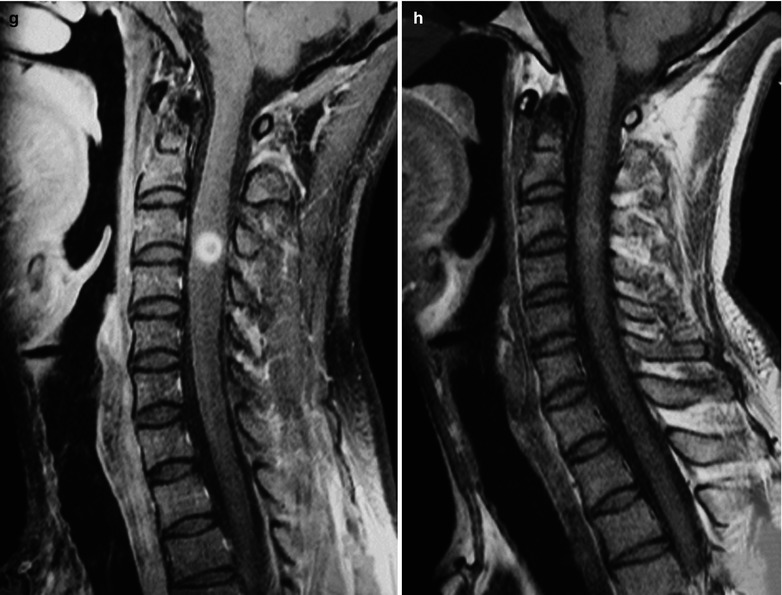
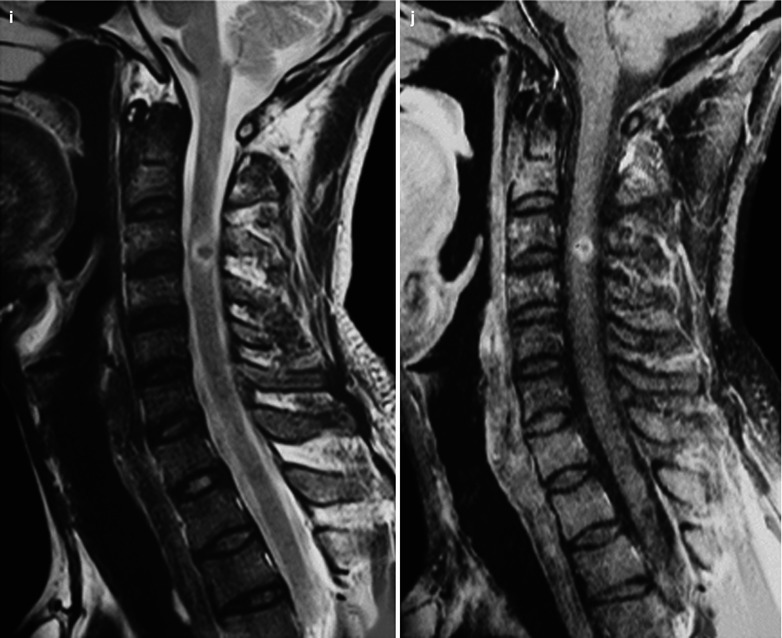
Fig. 14.1
(a–j) HIV/AIDS related spinal toxoplasma infection. (a–g) Pre-treatment. (h, j) Post-treatment. (a, b) Sagittal T1WI demonstrates round liked and slightly short T1 signal at C3–C4 level, equal T1 signal within it, swollen and thickened cervical spinal cord in the focal site. (c, d) Sagittal T2WI demonstrates long T2 signal of the focal margin with central even and short T2 signals, surrounded by spindle shaped edema. (e, f) Coronal and sagittal enhanced T1WI demonstrate obvious ring shaped enhancement of the foci. (g) Coronal enhanced T1WI demonstrates evident homogeneous enhancement of the foci. (h) Sagittal T1WI demonstrates shrunk foci. (i) Sagittal T2WI demonstrates ring shaped high signal of the foci with unobvious peripheral edema. (j) Saggital enhanced T1WI demonstrates shrunk foci with ring shaped enhancement
Case Study 2
A male patient aged 51 years was confirmatively diagnosed as having AIDS by CDC. His CD4 T cell count was 45/μl.
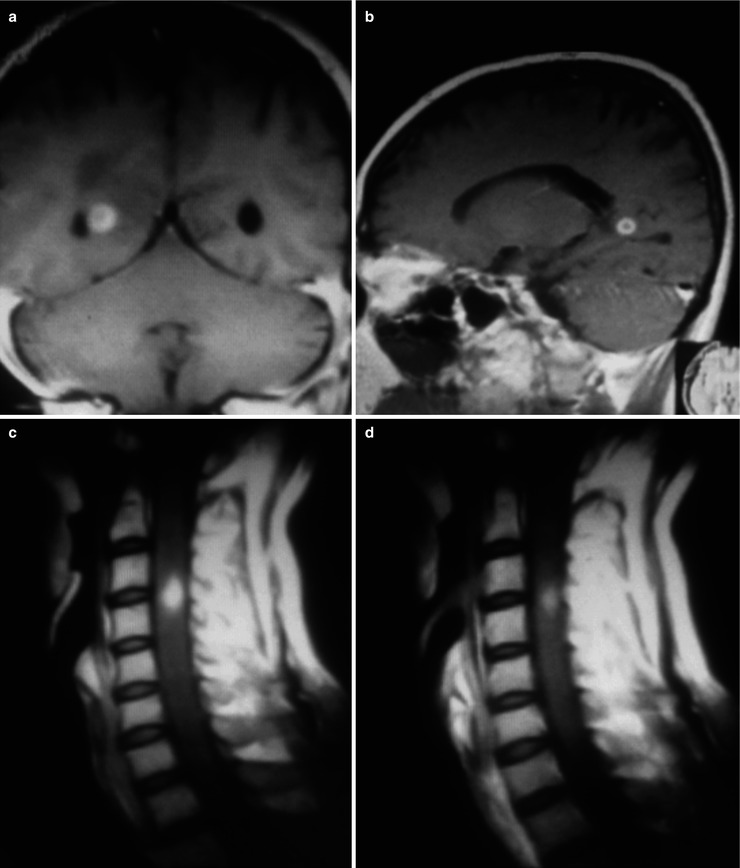
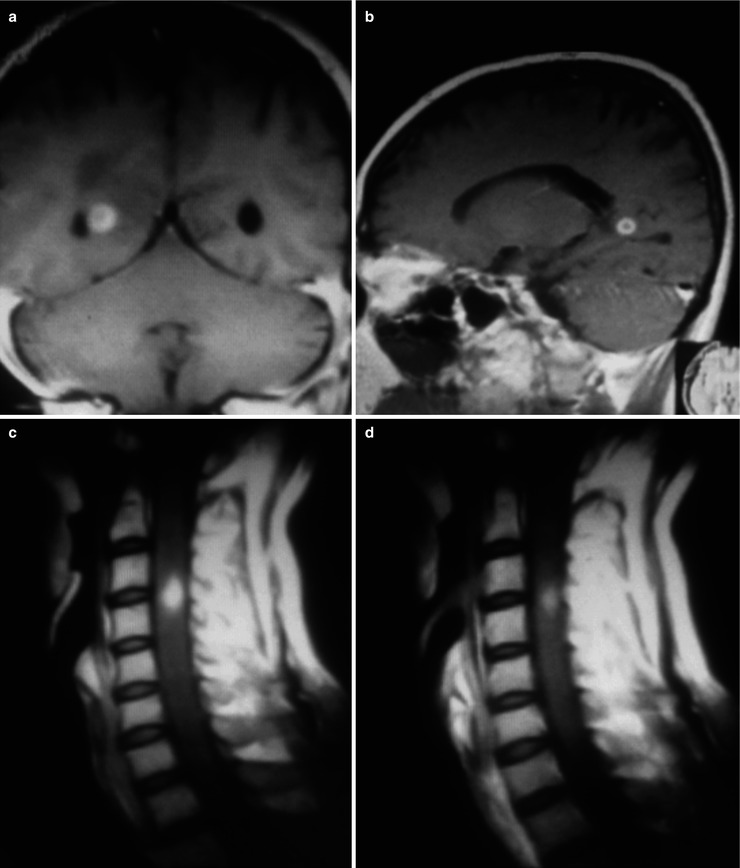
Fig. 14.2
(a–d) HIV/AIDS related cerebral and spinal toxoplasma infection. (a) Coronal enhanced T1WI demonstrates ring shaped enhancement of the foci adjacent to the right ventricle, with slightly compressed and deformed right ventricle. (b) Sagittal enhanced T1WI demonstrates ring shaped enhancement of the foci posterior to the body of lateral ventricle. (c, d) Sagittal enhanced T1WI demonstrates irregular foci at C3–C4 level, with homogeneous enhancement and blurry borderline
Case Study 3
The male patient aged 41 years was confirmatively diagnosed as having AIDS by CDC. His CT4 T count was 55/μl.
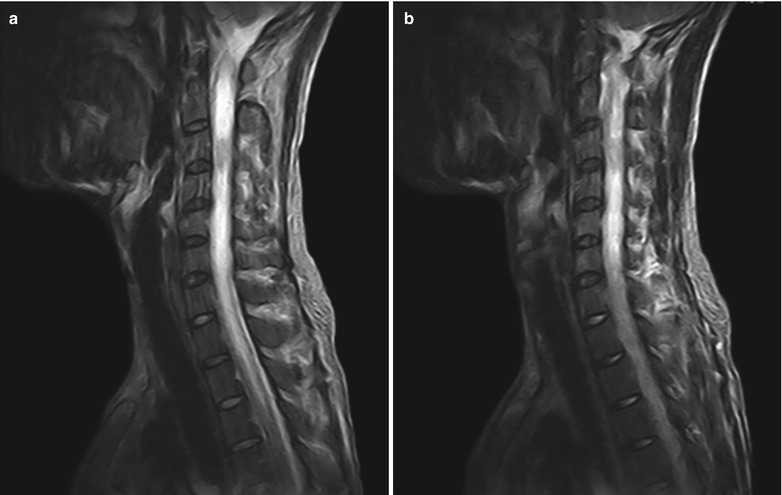
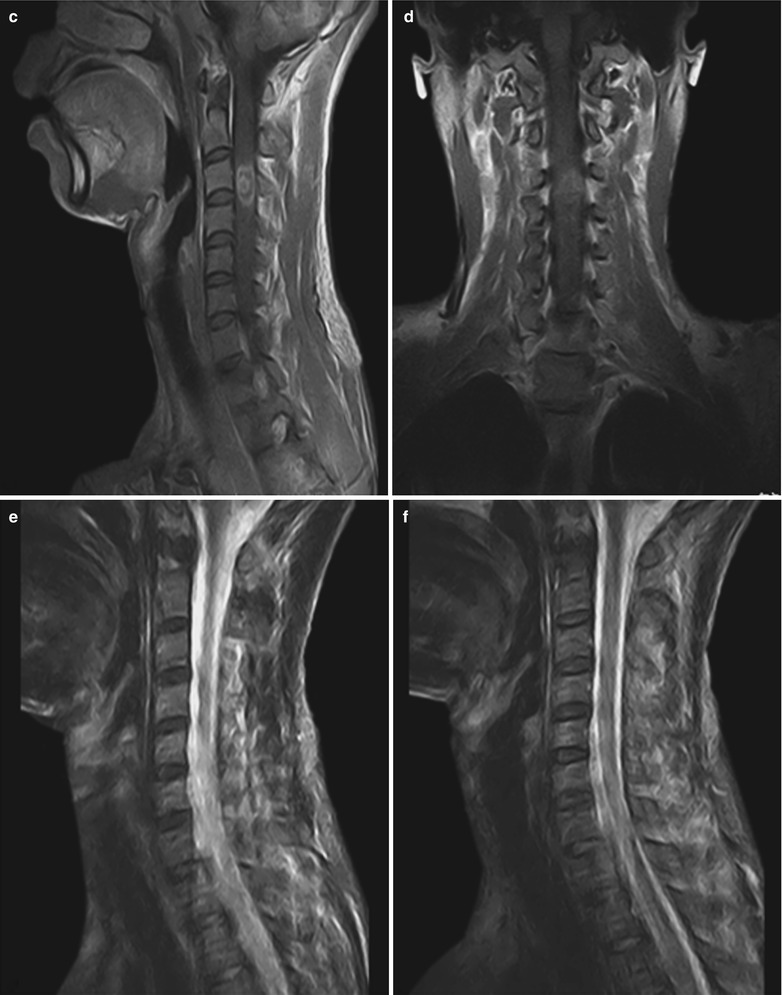
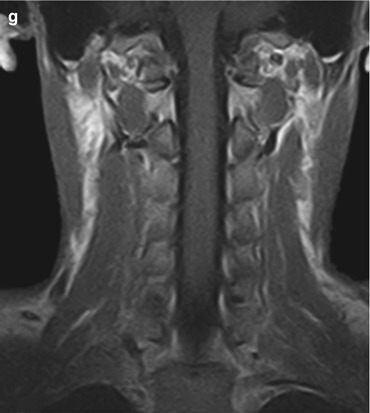
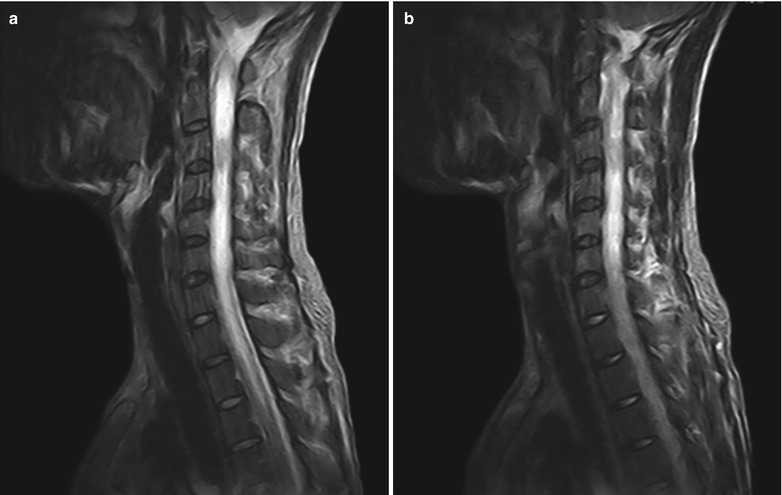
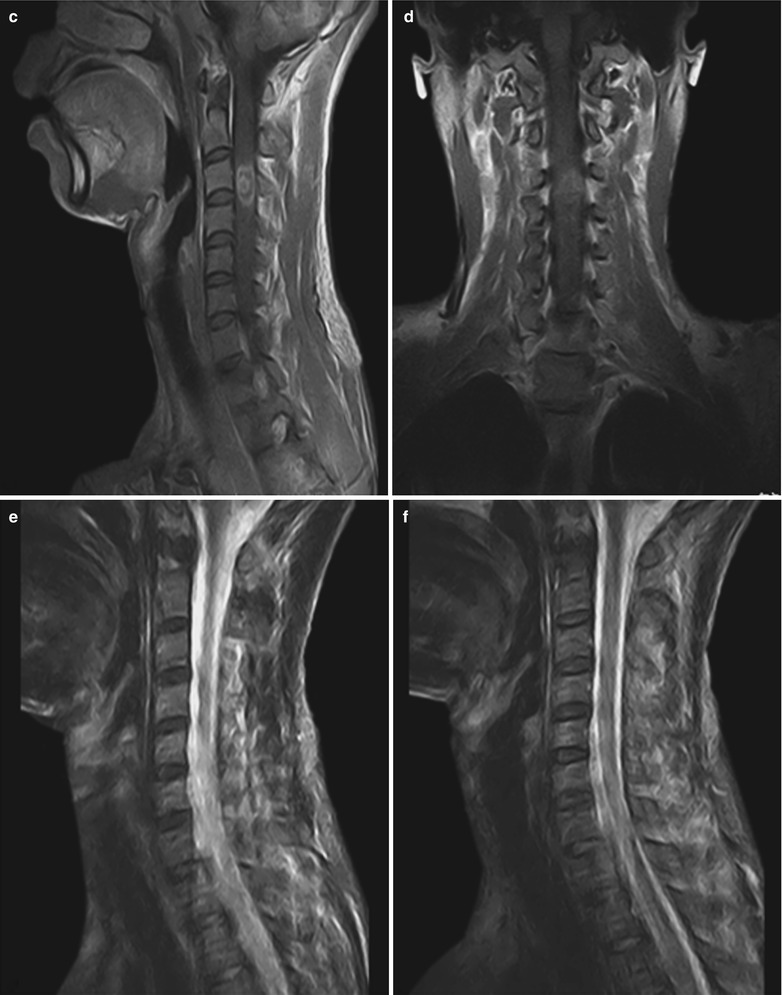
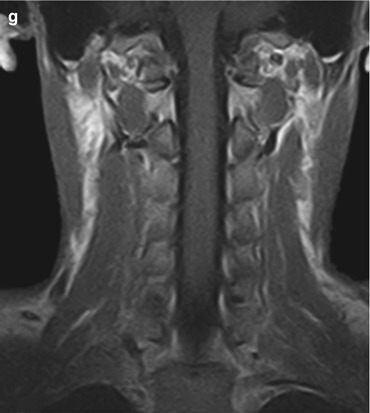
Fig. 14.3
(a–g) HIV/AIDS related spinal toxoplasma infection. (a, b) Sagittal T2WI demonstrates slightly swollen and enlarged cervical spinal cord, irregular short T2 signal of the foci at C3 level and peripheral long strips of edema with long T2 signal. (c) Sagittal enhanced T1WI demonstrates annular ring shaped enhancement of the spinal foci. (d) Coronal enhanced T1WI demonstrates inhomogeneous enhancement of the focuses. (e, f) Sagittal T2WI demonstrates no foci after treatment. (g) Coronal T1WI demonstrates no detectable foci
14.2.6 Criteria for the Diagnosis
The definitive diagnosis is based on the corresponding clinical manifestations. CSF test demonstrates a slight increase of white cells, increased proteins and positive serum toxoplasma antibodies IgA and IgG. The diagnosis can also be made based on biopsy of cerebrospinal fluid and histopathological examination.
14.2.7 Differential Diagnosis
14.2.7.1 Viral Myelitis
Viral myelitis has typical manifestations of concurrence of lesions around the veins and under the soft pia mater in the diseased white matter, with possible involvement of the gray matter, in a diffusive distribution. The disease has an acute onset, with initial clinical symptoms of fever, headache and nausea and the following symptoms of irritation, delirium, sleepiness and coma. The imaging demonstrations are not characteristic. CT scanning demonstrates diffusive low density areas in the white matter of the spinal cord. MR imaging demonstrates swollen spinal cord, equal or low signal by T1WI and high signal by T2WI. The foci are susceptible to bleeding. Enhanced scanning demonstrates no enhancement of the foci. The differential diagnosis depends on the test for serum anti-toxoplasma antibody, CSF biopsy and histopathological examination.
14.2.7.2 Spinal Bacterial Infection
Plain CT scanning demonstrates locally thickened spinal cord with irregular morphology, clearly defined border of intraspinal foci, and ring shaped enhancement of envelope membrane by enhanced scanning. Plain MR imaging demonstrates long T1 and short T2 signals of the envelope membrane, long T1 and T2 signals of the inner abscess fluids; and ring shaped enhancement of the abscess wall by enhanced imaging. CT and MRI demonstrate flaky or nodular enhancement before the formation of larger abscess cavity in the inflammation phase. By the diagnostic imaging, it is difficult to differentiate spinal bacterial infection from spinal toxoplasma infection. Laboratory tests and histopathological examinations should be performed for their differential diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree