(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
24.2.1 Pathogen and Pathogenesis
24.2.2 Pathophysiological Basis
24.2.3 Clinical Symptoms and Signs
24.2.5 Imaging Demonstrations
24.2.6 Diagnostic Basis
24.2.7 Differential Diagnosis
24.3.1 Pathogen and Pathogenesis
24.3.2 Pathophysiologic Basis
24.3.3 Clinical Symptoms and Signs
24.3.5 Imaging Demonstrations
24.3.6 Diagnostic Basis
24.3.7 Differential Diagnosis
24.4.1 Pathogen and Pathogenesis
24.4.2 Pathophysiologic Basis
24.4.3 Clinical Symptoms and Signs
24.4.5 Imaging Demonstrations
24.4.6 Diagnostic Basis
24.4.7 Differential Diagnosis
24.5.1 Pathogen and Pathogenesis
24.5.2 Pathophysiologic Basis
24.5.3 Clinical Symptoms and Signs
24.5.5 Imaging Demonstrations
24.5.6 Diagnostic Basis
24.5.7 Differential Diagnosis
24.6.1 Pathogen and Pathogenesis
24.6.2 Pathophysiological Basis
24.6.3 Clinical Symptoms and Signs
24.6.5 Imaging Demonstrations
24.6.6 Diagnostic Basis
24.6.7 Differential Diagnosis
24.7.1 Cerebral Atrophy
24.7.2 Cerebral Infarction
24.8.1 Pathogen and Pathogenesis
24.8.2 Pathophysiologic Basis
24.8.3 Clinical Symptoms and Signs
24.8.5 Imaging Demonstrations
24.8.6 Diagnostic Basis
24.8.7 Differential Diagnosis
24.9.1 Pathogen and Pathogenesis
24.9.2 Pathophysiologic Basis
24.9.3 Clinical Symptoms and Signs
24.9.5 Imaging Demonstrations
24.9.6 Diagnostic Basis
24.9.7 Differential Diagnosis
24.10.1 Osteoporosis
24.10.2 Epiphyseal Sclerosis
24.11.1 Pathogen and Pathogenesis
24.11.2 Pathophysiologic Basis
24.11.3 Clinical Symptoms and Signs
24.11.4 Examinations and Their Selection
24.11.5 Imaging Demonstrations (X-ray)
24.11.6 Diagnostic Basis
24.11.7 Differential Diagnosis
Abstract
Since the prevalence of HIV/AIDS, there had been 3.2 million children patients with HIV/AIDS worldwide till the year of 2002. The diagnostic criteria for pediatric AIDS formulated by the CDC of the United States are: children under the age of 13 years, with characteristic opportunistic infection or neoplasm caused by cellular immunodeficiency that excludes primary immunodeficient diseases, other congenital diseases and the cases with a history of immunodepressant used. Pediatric HIV/AIDS is the most commonly infected via vertical transmission from mother to children, and blood transfusion and the use of blood products are the second commonly transmission route. The vertical transmission occurs in the late period of pregnancy and before/after delivery. The HIV gains its access to the fetus via the placenta (intrauterine infection) or via contacting secretions containing HIV during delivery. It is believed that the transmission rate is related to the viral load of the mother. In the cases with HIV RNA above 50,000 copies/ml, vertical transmission occurs.
24.1 An Overview of HIV/AIDS Related Pediatric Diseases
Since the prevalence of HIV/AIDS, there had been 3.2 million children patients with HIV/AIDS worldwide till the year of 2002. The diagnostic criteria for pediatric AIDS formulated by the CDC of the United States are: children under the age of 13 years, with characteristic opportunistic infection or neoplasm caused by cellular immunodeficiency that excludes primary immunodeficient diseases, other congenital diseases and the cases with a history of immunodepressant used. Pediatric HIV/AIDS is the most commonly infected via vertical transmission from mother to children, and blood transfusion and the use of blood products are the second commonly transmission route. The vertical transmission occurs in the late period of pregnancy and before/after delivery. The HIV gains its access to the fetus via the placenta (intrauterine infection) or via contacting secretions containing HIV during delivery. It is believed that the transmission rate is related to the viral load of the mother. In the cases with HIV RNA above 50,000 copies/ml, vertical transmission occurs.
Compared to AIDS in adults, pediatric HIV/AIDS is characterized by: (1) The latent period after HIV infection is short, with acute onset of the disease and rapid progression. (2) The growth retardation deviated from common growth curve is a typical manifestation of pediatric HIV infection. (3) Bacteria infections recur, commonly lymphatic interstitial pneumonia. (4) Encephalopathy syndrome is common in infants and young children, which has an early onset, rapid progression and poor prognosis. (5) About 50 % infected children have accompanying diffuse lymphadenectasis and repeated diarrhea. About one third infected children have accompanying thrombocytopenia. Some infected children have eczema liked skin rashes and repeated otitis media.
24.2 HIV/AIDS Related Lymphoid Interstitial Pneumonia
Lymphoid interstitial pneumonia (LIP) is a lung disease with respiratory distress caused by HIV infection of children. Its pathological changes are characterized by specific pulmonary infiltration of lymphocytes. It was firstly reported by Carrhigton and Liebow in 1966 [1]. Since then, its occurrence in children with HIV/AIDS is continually reported. LIP in children under 13 years of age is defined as the diagnostic indicator of HIV/AIDS by the CDC of the United States.
24.2.1 Pathogen and Pathogenesis
LIP has an incidence of 16–50 % in children with HIV, commonly at the age of 2–3 years. Currently, it is believed that LIP in children with HIV infection is caused by the immunological responses. Most studies indicate that the proliferating lymphocytes in HIV infected patients are CD8 or cytotoxic/inhibited T lymphocytes. These cells cause immunological impairments via different ways, including T cells activation caused by immunological identification of antigens, production of lymphokines by CD4 lymphocytes such as interleukin-2 and proliferation of effector cells responsible for tissue lesions caused by lymphokines that is mainly CD8 cells in HIV/AIDS. Currently, the following three factors are believed to be related to the pathogenesis of HIV/AIDS. (1) HIV infection causes proliferation of lymphocytes in the body. The lung lesions can be relieved by using the Zidovudine therapy. HIV antigens and antibodies can be found in the bronchoalveolar lavage fluid of LIP patients. (2) HIV and EB virus synergetic infection: Most children with LIP have concurrent EBV infection. Otherwise, EB virus genome can be found that causes lymphatic tissue hyperplasia in lungs of HIV positive children. EB virus infection is transmitted via contacts, with LIP patients as its susceptible population. (3) The immunogenetics basis: It has been demonstrated that more HLA-DR6 can be found in HIV positive patients, with occurrence of CD8 lymphocytosis syndrome and LIP. Generally, the factors of immunological nonspecific stimulation, HIV specific stimulation or EB virus infection and HIV infection contribute to the onset of LIP in HIV positive patients.
24.2.2 Pathophysiological Basis
Gross lung specimen demonstrates diffuse thickening of the pulmonary interstitium. Microscopy demonstrates mass liked mixed cells infiltration in the septa of pulmonary lobes, alveolar wall, bronchus, bronchioles and perivascular tissues, which is mainly mature lymphocytes and occasionally generative center with no nucleus cleavage. Lymphatic follicle with generative center is common. There are hyperplasia of type II alveolar epithelium, and increased macrophages in the alveolar cavity.
24.2.3 Clinical Symptoms and Signs
The onset is chronic, with symptoms of cough, dyspnea and hypoxia. Lung auscultation may be negative or may find weakened respiration sound, wheezing and end-inspiratory dry rales. Most of the children patients have bronchospasm, with no cough before demonstration of lesions by chest X-ray. The patients with long term illness course have clubbing fingers/toes and parotid/lymphaden enlargement. The pulmonary functions impaired children have serious hypoxia which causes oxygen dependency. Due to the decrease of lymphocytes and CD4 T cell count, the critical cases with lift threatening conditions are rare, but the patients are more susceptible to opportunistic infections.
24.2.4 Examinations and Their Selection
24.2.4.1 Laboratory Tests
Laboratory tests may demonstrate slight anemia, immunoglobulin manufacturing abnormalities and about 80 % patients with LIP have serum protein abnormality.
24.2.4.2 Pulmonary Function Examinations
Pulmonary function examinations commonly demonstrate restricted pulmonary ventilation disturbance, decreased functional diffusion and hypoxemia.
24.2.4.3 Alveolar Lavage
Alveolar lavage fluid has certain diagnostic value for LIP. The increases of lymphocytes, CD3 T cells, and polyclone CD20 B cells in bronchoalveolar lavage fluid indicate the diagnosis of LIP.
24.2.4.4 Chest X-ray and CT Scanning
Both are commonly used examinations, but with non-specific findings.
24.2.4.5 Lung Biopsy
The diagnosis of LIP depends on histological examination.
24.2.5 Imaging Demonstrations
24.2.5.1 Chest X-ray
Chest X-ray demonstrates non-specific findings for the diagnosis of LIP. Both lungs have diffuse interstitial infiltration that is mostly symmetric network or find network and nodular shadows. Otherwise, they are thick network and nodular shadows or thick nodular shadows. The network liked shadows are linear or leather liked, with a distribution in the basement of the lungs. The lesions can also be located in the upper lungs or middle lobes, with air bronchogram sign. Hilar/Mediastinal lymphadenectasis is rare, and pleural effusion is rare.
24.2.5.2 CT Scanning
High-resolution computed tomography (HRCT) has main demonstrations of diffuse ground glass liked changes, blurry centrilobular nodules and subpleural small nodules (1–4 mm), thickened interlobular septa, thickened bronchovascular bundles and scattering thin-walled cysts. The demonstrations of turbid interlobular grids, honeycomb liked deformation and bronchiectasis are rare. By HRCT, thin walled cysts can be found in 68–82 % children with LIP, which have diameters of 1–3 mm in a small quantity. Pulmonary involvement can be found in less than 10 % cases, with demonstrations overlapping with ground glass liked changes. The pulmonary ground glass liked changes pathologically demonstrate diffuse infiltration of alveolar septum lymphocytes and plasmocytes. Generally, demonstrations by CT scanning of thin sections of ground glass liked changes predict that the lesions can be absorbed or are healing. Due to the infiltration of lymphocytes in the surrounding tissues of bronchioles, the airway is obstructed and dilated to finally cause cysts. The primary lesions of parenchymal changes can also progress into cysts and the formation of cysts is irreversible. The pulmonary parenchymal changes can be partially absorbed and partially progress into honeycomb liked lung. Generally, the newly emerging cysts mostly occur at the site of primary centrilobular nodules. And the honeycomb liked changes commonly occur in the areas with original pulmonary parenchymal changes.
Case Study
A boy patient aged 2 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 25/μl.
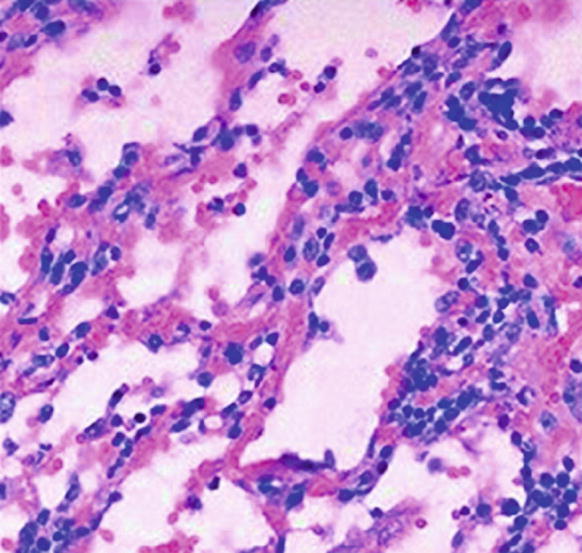
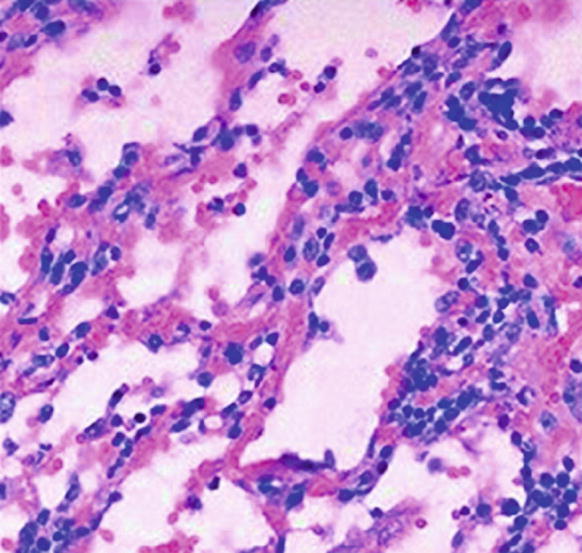
Fig. 24.1
HIV/AIDS related lymphoid interstitial pneumonia. It is demonstrated to have infiltration of large quantity lymphocytes around alveoli
24.2.6 Diagnostic Basis
Clinical manifestations in pediatric AIDS patients include cough, dyspnea and hypoxia, which have a slowly progressive course. The occurrence of lymphocytosis and hyperglobulinemia with no other isolated pathogens in combination with chest diagnostic imaging findings can define the clinical diagnosis. Based on the findings of bronchoalveolar lavage fluid examination and lung biopsy, the definitive diagnosis can be made.
24.2.7 Differential Diagnosis
24.2.7.1 Pneumocystis Carinii Pneumonia
The characteristic CT scanning demonstrations of PCP are bilaterally symmetric extensive ground glass liked shadows in both lungs. Otherwise, the shadows are in patchy or map liked distribution. However, early PCP is difficult to be differentiated from LIP by the diagnostic imaging. Bronchoalveolar lavage contributes to the differential diagnosis.
24.2.7.2 Miliary Pulmonary Tuberculosis
Most cases of military pulmonary tuberculosis have symptoms of acute infections. The pulmonary lesions are mostly located in the upper and middle lungs, with even size and in bilaterally symmetric distribution. Pathological examinations contribute to the differential diagnosis.
24.2.7.3 Cytomegalovirus Pneumonia
The clinical manifestations are non-specific. Chest X-ray demonstrates diffuse network nodular shadows or flaky thin shadows. The definitive diagnosis depends on the histological diagnosis.
24.3 HIV/AIDS Related Pulmonary Bacterial Infection
Respiratory system is the most commonly involved body part by opportunistic infections of AIDS. Bacterial pneumonia is one of the major causes of death in AIDS patients. It has been reported that in every 10 cases of death in AIDS patients each year, 1 case is from bacterial pneumonia, and the cases of HIV positive bacterial pneumonia are 78 times as many as those of HIV negative bacterial pneumonia.
24.3.1 Pathogen and Pathogenesis
AIDS children are susceptible to bacterial pneumonia, which is related to their immune deficiency. B cell dysfunction leads to decreased production of antigen specific antibody, T cell functional impairment and neutrocytopenia, which, in combination with intravenous drug use and other factors, result in their susceptibility to various bacteria. Currently, the reported pathogenic bacteria include streptococcus pneumonia, hemophilus influenza, pseudomonas, staphylococcus aureus and legionella.
24.3.2 Pathophysiologic Basis
By microscopic observation, pneumonia caused by streptococcus pneumonia has lesions in different sizes with small spots and flakes of focal inflammation. The lesions are more serious in the inferior lobes and dorsal segment of both lungs. The lesions are in dark red and slightly protrude in the section that is smooth with no particle. In the young children, fusion of multiple small lesions is common, and sometimes even involves the whole lung lobe. Under a microscope, at the center and peripheral areas of the lesions, there are inflammatory bronchi and the lesions are filled with neutrophilic granulocyte as well as lytic and shed epithelial cells. The surrounding alveoli are initially filled with exudates containing abundant proteins, followed by occurrence of neutrophilic granulocyte, erythrocytes as well as shed and enlarged alveolar epithelial cells. The cellulose is rarely found. In the advanced stage of pneumonia, the exudates are commonly transformed into purulent fluid.
By the naked eyes observation, staphylococcus aureus pneumonia has coverage of the pleural surface by a thick layer of fibrinous purulent secretions, protruding grayish yellow or yellowish parenchymal changes under the pleura, extensive hemorrhagic necrosis and multiple small abscesses in the lungs. Once the subpleural small abscesses rupture, pyothorax or pneumopyothorax occurs, sometimes with involved bronchi to form bronchopleural fistula. Microscopic observation demonstrates alveoli filled with bloody edema, occasionally macrophages and small quantity neutrophils. There are also large quantities of Staphylococcus aureus and necrotic tissue debris in the abscess, bronchial lumen filled with pyocyte, seriously damaged mucosa, collapsed parenchymal changes on the cross section to form most abscesses.
24.3.3 Clinical Symptoms and Signs
The involvement of lungs in HIV positive patients has non-specific symptoms and signs. The clinical manifestations include cough, fever and shortness of breath. The symptoms are obvious, being more acute and serious than those in adult patients. Fever and shortness of breath are especially common in HIV/AIDS children. Its further progression may cause bacteremia and sepsis. By physical examinations, there are tachypnea, tachycardia, pulmonary dry and moist rales and pulmonary parenchymal changes.
24.3.4 Examinations and Their Selection
24.3.4.1 Laboratory Tests
Laboratory tests demonstrate increased C-reactive protein concentration, which is important for the diagnosis and differential diagnosis of bacterial pneumonia. Pathogenic examinations are the basis for the definitive diagnosis.
24.3.4.2 Diagnostic Imaging
Chest X-chest and CT scanning are commonly used imaging examinations, which contribute greatly to the diagnosis and prognosis prediction.
24.3.5 Imaging Demonstrations
Chest X-ray demonstrates pneumococcus pneumonia as high density blurry shadows in the lungs fields, commonly with concurrent pleural effusion or pyothorax. Sometimes nodular lesions and clubbed lesions can also be found at the base of lungs. CT scanning demonstrates thickened bronchial wall and bronchiectasis.
Chest X-ray and CT scanning demonstrate legionella pneumonia as involvement of singular or multiple lung lobes, with a rapid progression. Cavities and empyema are common. Interstitial infiltration may also occur.
Chest X-ray and CT scanning demonstrate bronchogenic staphylococcus aureus pneumonia as multiple small patches of high density shadows in the middle zone of both lungs, with blurry boundary and accompanying transparent areas, which are lesions of focal obstructive emphysema. Dynamic observation of the intrapulmonary lesions demonstrates that the lesions can progress from patches of parenchymal changes into extensive large flakes or segments of lesions within several hours or 1 day. Round or oval shaped low density air sacs occur within 1–2 days after the onset. The rapid progression demonstrated by the diagnostic imaging is characteristic. Sometimes, pulmonary cavities containing gas–liquid level can be found. Pleural effusion, empyema, and pyopneumothorax are also common. By chest X-ray, the secondary blood-borne staphylococcus aureus pneumonia is demonstrated to have patches or spherical high density shadows in middle and lower fields of both lungs.
Case Study 1
A boy patient aged 4 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 25/μl.
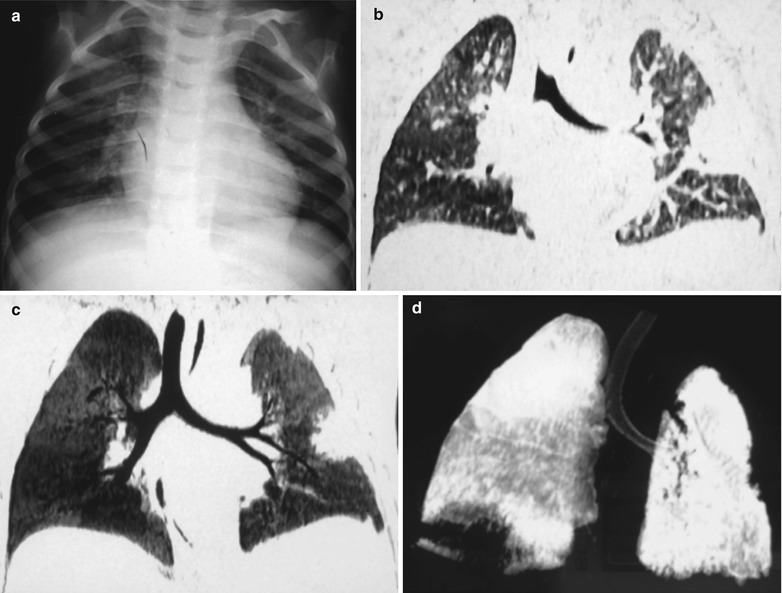
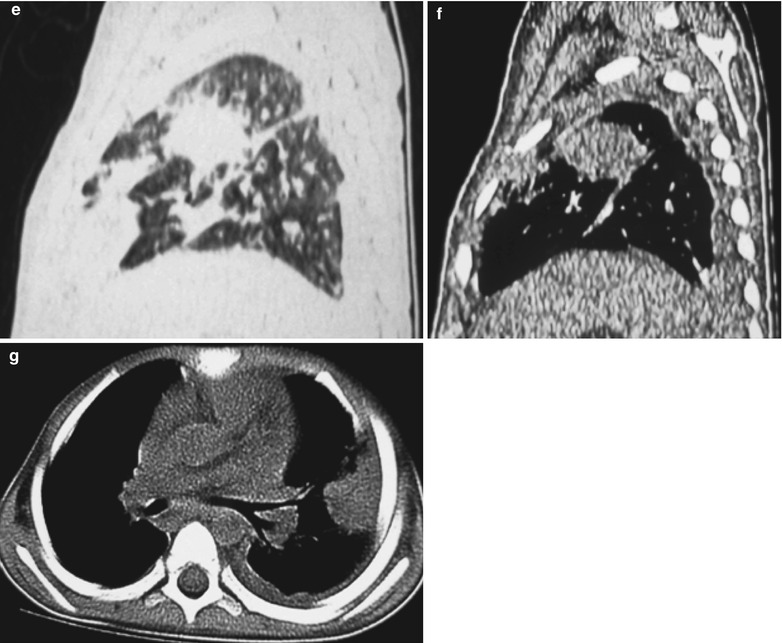
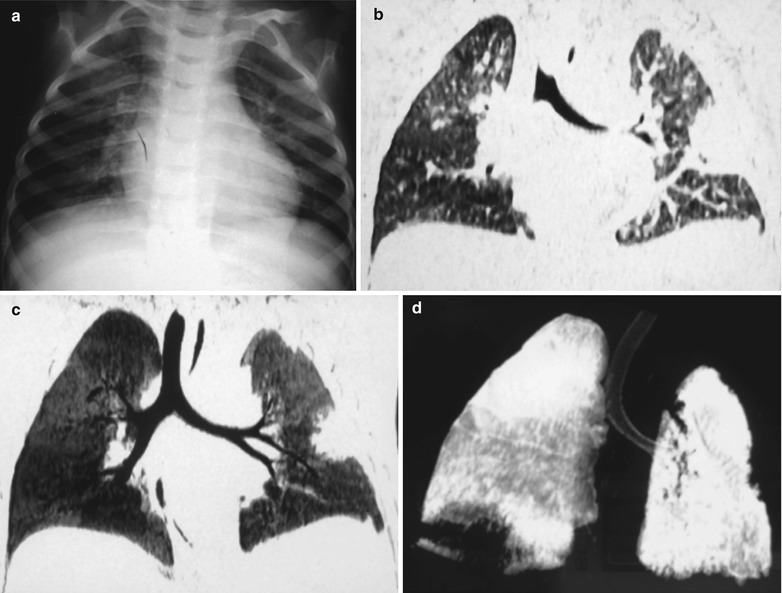
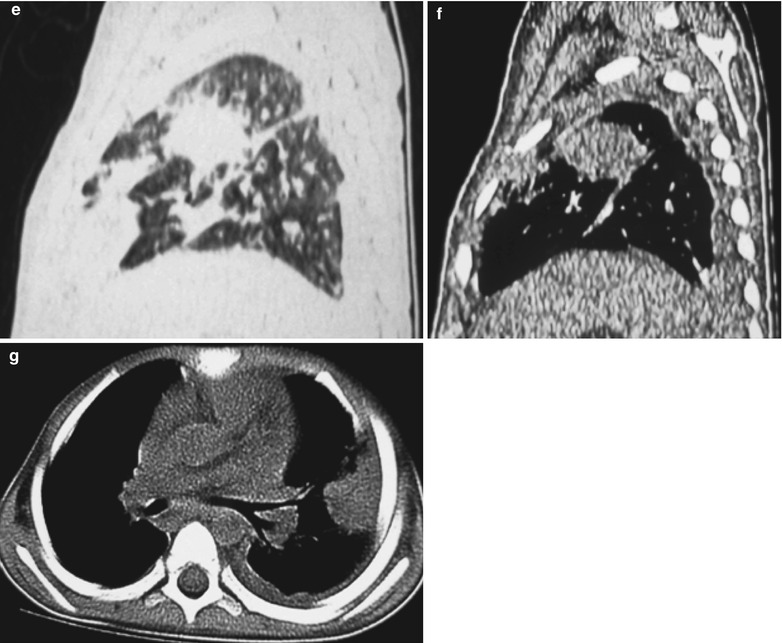
Fig. 24.2
(a–g) HIV/AIDS related bacterial infection. (a) Chest X-ray demonstrates multiple shadows with increased density in both lungs, which is more obvious in the right upper lung. (b–d) Coronal plain CT scanning demonstrates high density parenchymal changes shadows in both lungs, which is more obvious in the left lung. (e, f) Sagittal plain CT scanning demonstrates parenchyma lesions. (g) CT scanning of the mediastinal window demonstrates parenchyma lesions in the left lung, left pleural effusion and pleural hypertrophy
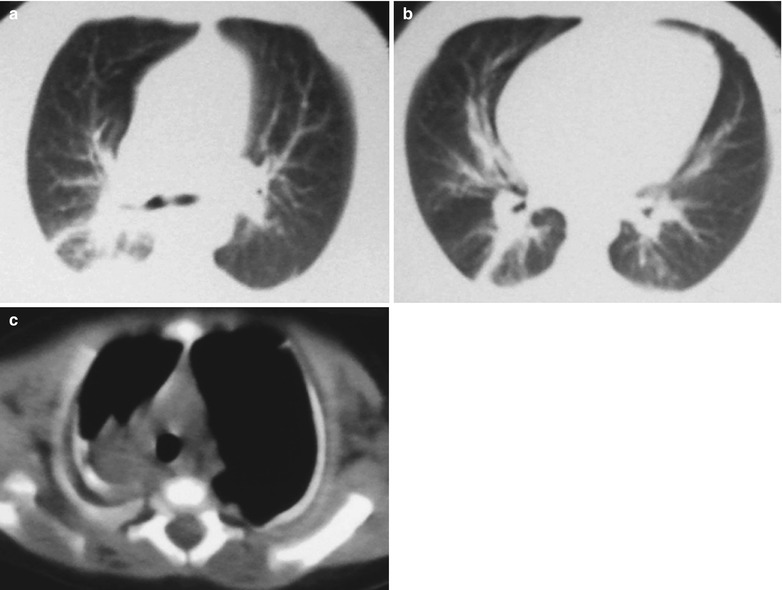
Case Study 2
A boy patient aged 3 years was confirmatively diagnosed as having AIDS by the CDC. He had symptoms of cough and fever and his CD4 T cell count was 45/μl.
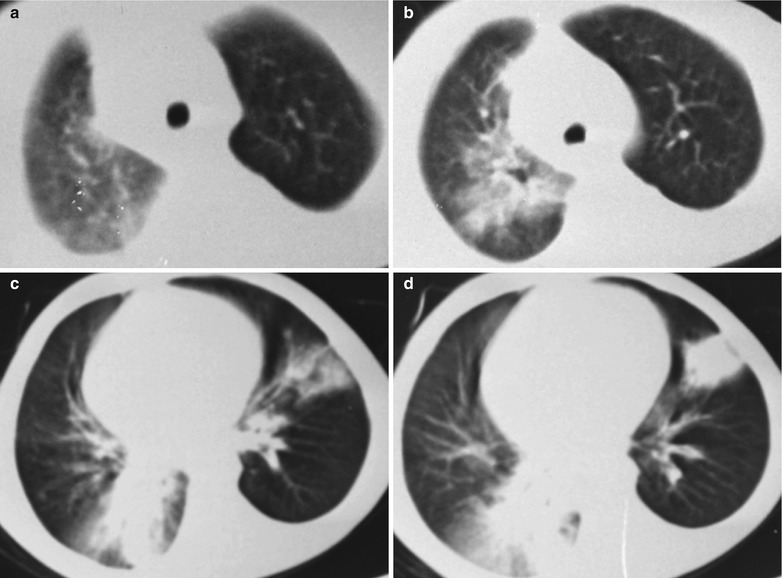
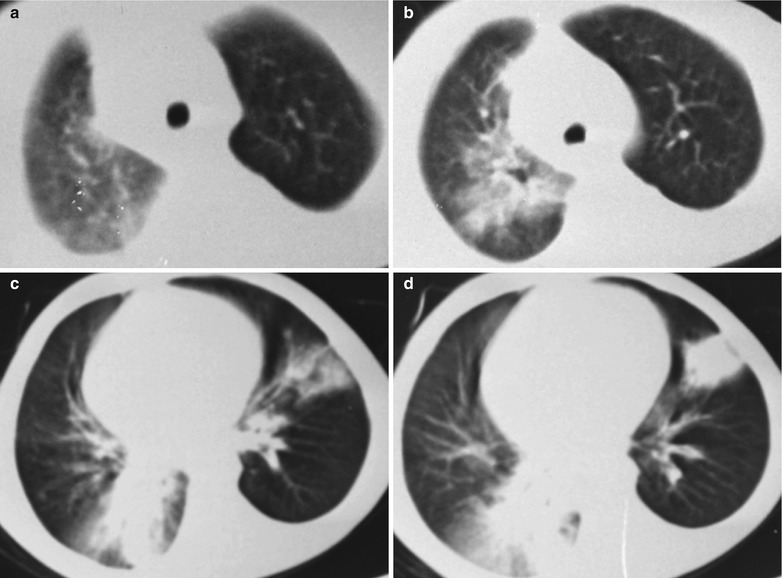
Fig. 24.3
(a) CT scanning demonstrates increased density shadows in the upper lobe of the right lung, and small flakes of ground glass liked shadows. (b) CT scanning demonstrates large flakes of high density parenchymal shadows in the upper lobe of the right lung, with blurry boundary. (c, d) CT scanning demonstrates high density parenchyma shadows in both lungs, with air bronchogram sign in them
Case Study 3
A boy patient aged 11 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 29/μl.
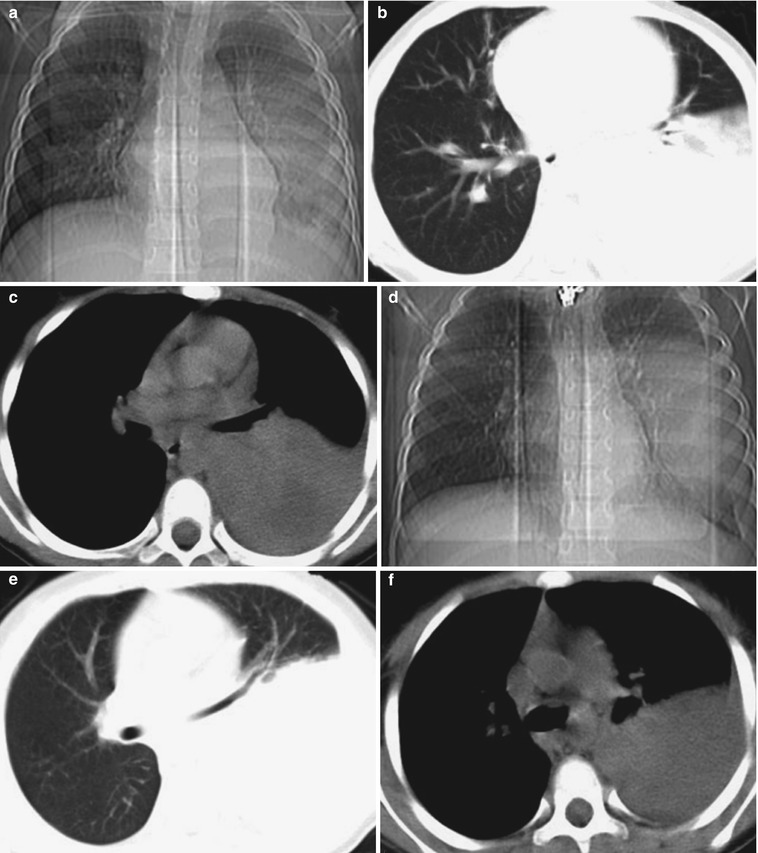
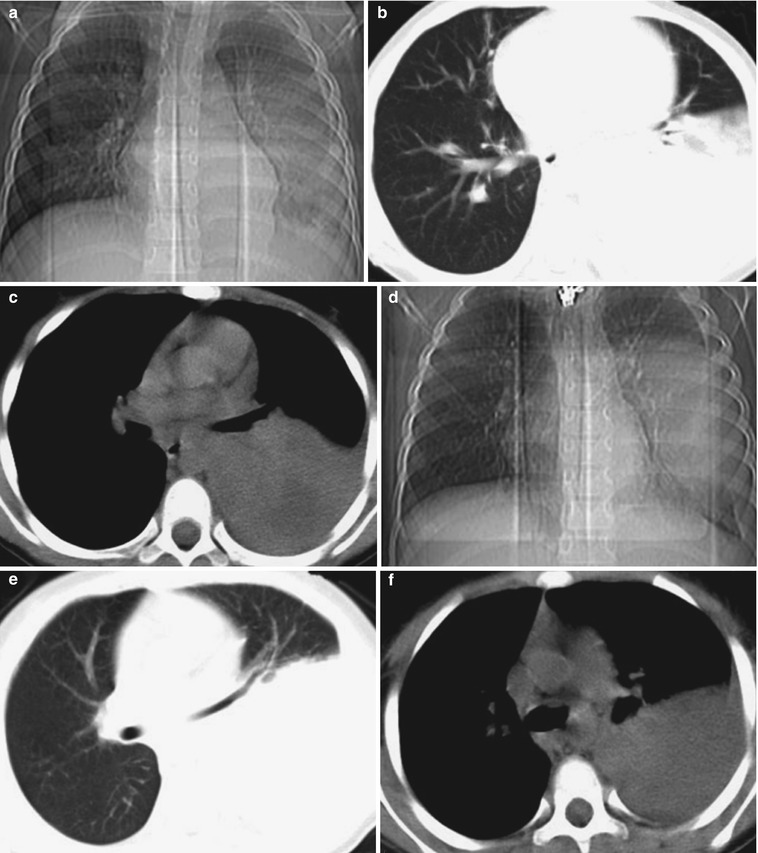
Fig. 24.4
(a–f) HIV/AIDS related bacterial infection. (a–c) It is demonstrated the lesions pre-treatment. (d–f) It is demonstrated the lesions post-treatment. (a) DR demonstrates large flakes of shadows with increased density in left lung. (b) Pulmonary window demonstrates high-density parenchymal shadows in the left lung, with smooth anterior margin; and cords liked shadows in the medial segment of the middle lobe of the right lung. (c) Mediastinal window demonstrates parenchymal changes of soft tissue density in the left lung, with irregular low density areas in them. (d) DR demonstrates progressed lesions in the left lung, lesions with increased density, and extended range with lesions. (e) Pulmonary window demonstrates high density parenchymal shadows in the left lung, compressed and narrowed bronchi in the upper lobe of the left lung, with forward migration. (f) Mediastinal window demonstrates even density of lung tissues with parenchymal changes, straight and smooth anterior margins of the lesions
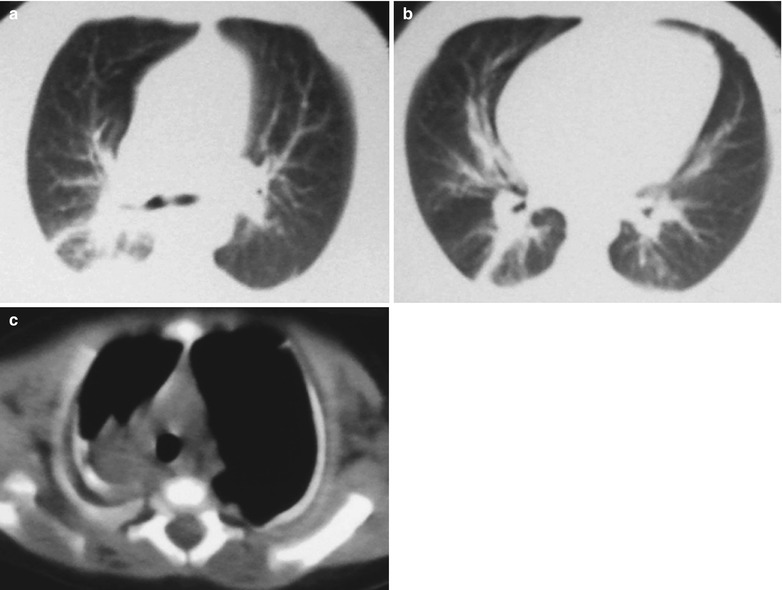
Case Study 4
A girl patient aged 9 years was confirmatively diagnosed as having AIDS by the CDC. She was infected via vertical transmission of HIV, with manifestations of fungal stomatitis, drug induced hepatitis, moderate anemia and hepatitis C. Her CD4 T cell count was 6/μl.
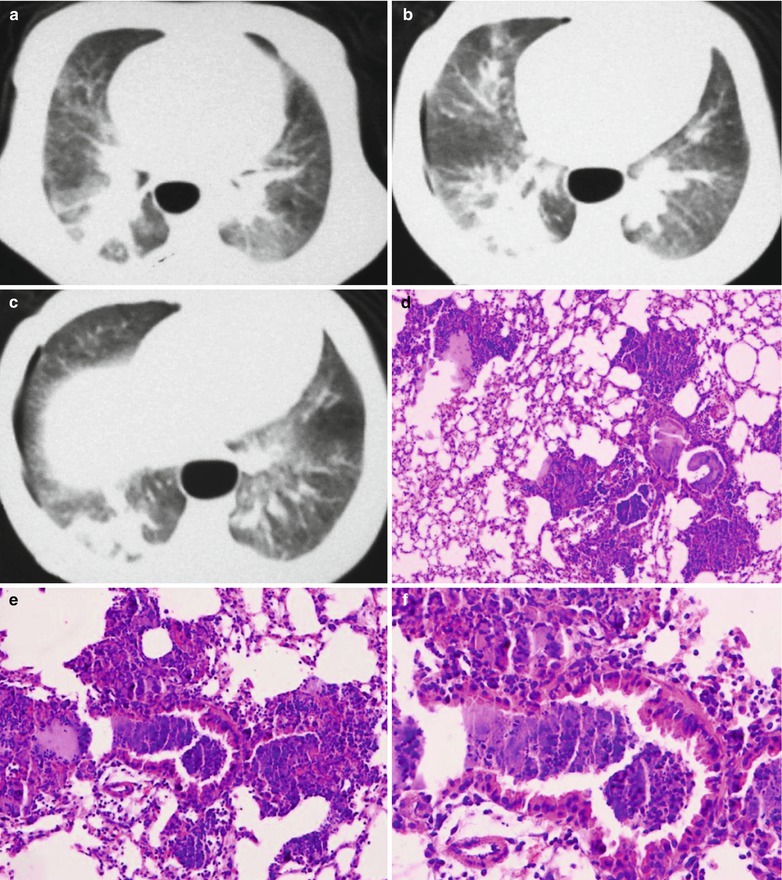
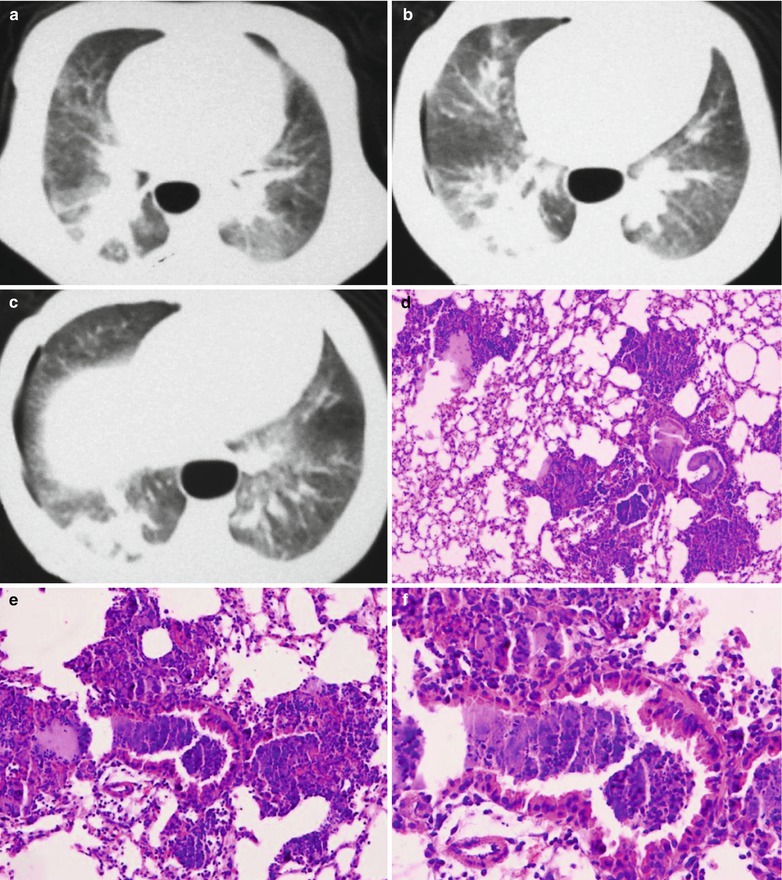
Fig. 24.5
(a–f) HIV/AIDS related bacterial infection and pneumothorax. (a–c) Pulmonary window demonstrates multiple patches and large flakes of shadows with increased density in both lungs, abnormal transparent area without lung markings in the lateral zone of the right lung. (d–f) HE staining demonstrates many inflammatory cells infiltration in the lung tissues around the bronchioles, and inflammatory exudates in the bronchiole lumen (HE × 10, ×20, ×40)
Case Study 5
A boy patient aged 8 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 13/μl.
Figs. 24.6
(a–c) HIV/AIDS related bacterial infection. (a, b) CT scanning demonstrates high density parenchyma shadows and multiple cords liked shadows in the right lung, and ground glass liked shadows in the left lung. (c) CT scanning of the mediastinal window demonstrates decreased volume of the right lung, and soft tissue density of the lung tissues with parenchymal changes
Case Study 6
A boy patient aged 6 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 63/μl.
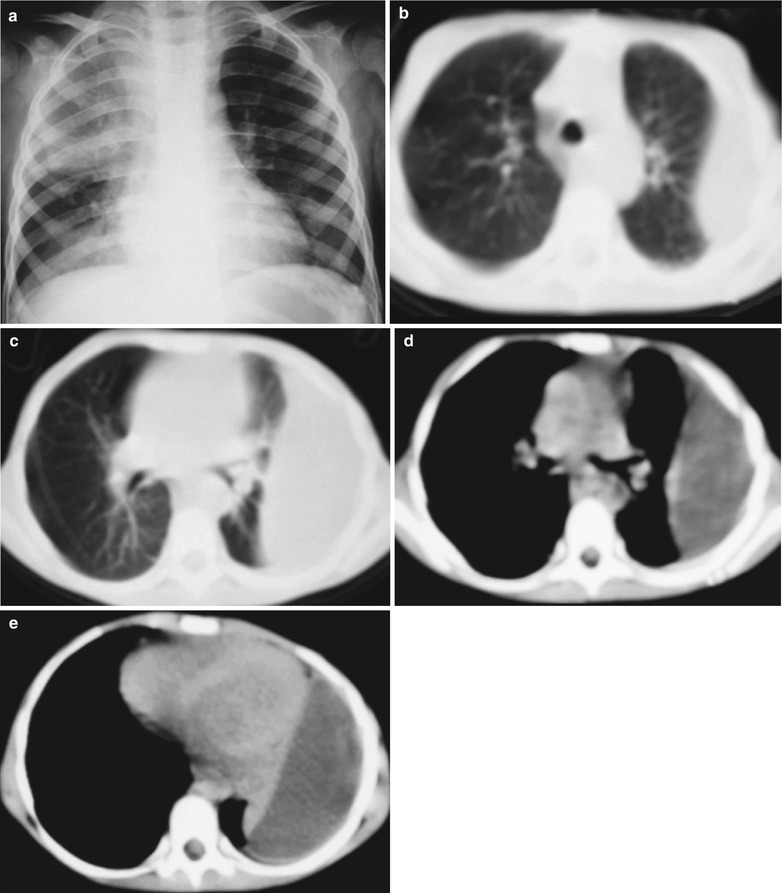
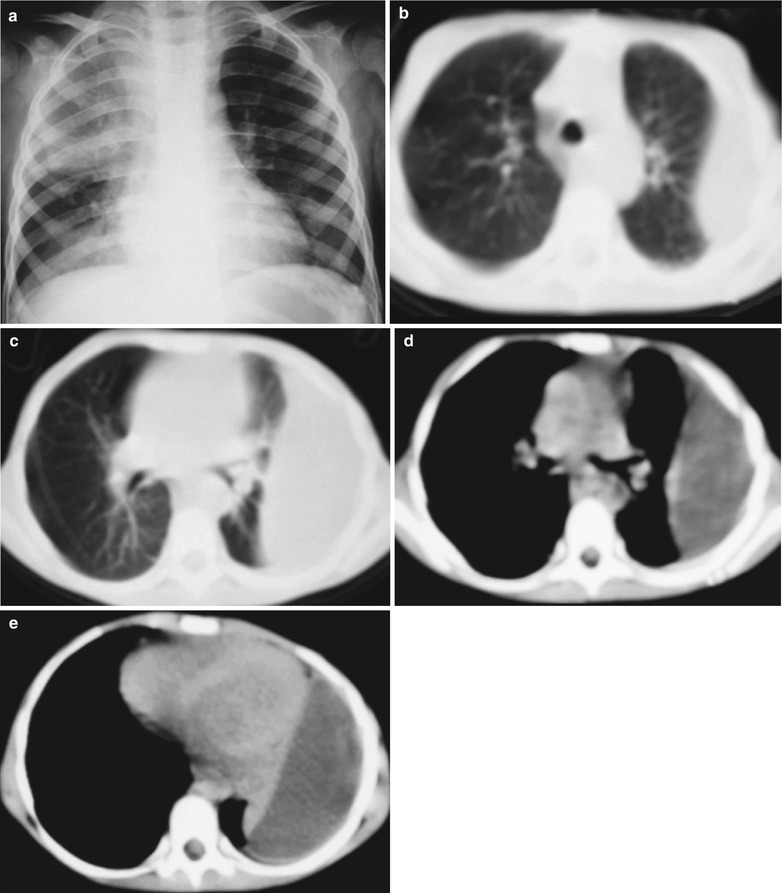
Fig. 24.7
(a–e) HIV/AIDS related bacterial infection and encapsulated pleural effusion. (a) Chest X-ray demonstrates parenchymal changes in the right lung, which is more obvious in the upper right lung; and blurry flakes of shadows in the left lower lung. (b, c) CT scanning of the pulmonary window demonstrates increased density of both lungs, left encapsulated pleural effusion, compressed left lung with shrinkage of lung volume. (d, e) Mediastinal window demonstrates left encapsulated pleural effusion and left pleural hypertrophy
24.3.6 Diagnostic Basis
1.
The most common clinical manifestations are cough, fever and shortness of breath. There is also moist rale of lungs.
2.
Laboratory tests demonstrate obviously increased total WBC count.
3.
The imaging demonstrations include lobar or segmental high density shadows of parenchymal changes, air bronchogram sign with blurry boundary.
24.3.7 Differential Diagnosis
Pulmonary infection in AIDS children should be firstly differentiated from PCP, which is the most common pulmonary opportunistic infection in AIDS children. Therefore the sputum specimen should be conventionally stained. In combination with the clinical manifestations and imaging findings, differential diagnosis can be made. However, complications of various bacterial infections occur in AIDS children with PCP, which should be paid focused attention. Meanwhile, it should also be differentiated from pulmonary tuberculosis. The clinical manifestations, results of PPD test and the findings of pathogenic examinations should be integrated for the differential diagnosis.
24.4 HIV/AIDS Related Pneumocystis Carinii Pneumonia
Pneumocystis carinii pneumonia is an opportunistic infections of the respiratory system caused by the Pneumocystis carinii. In the past, it was only found in severely malnourished infants and children with leukemia undergoing immunosuppressive therapy. With the increasing incidence of AIDS, the incidence of PCP is obviously increasing, which is one of the common opportunistic infections in AIDS children and the common cause of death. PCP occurs commonly in infants aged 3–12 months, and rarely in young children aged above 1 year.
24.4.1 Pathogen and Pathogenesis
Pneumocystis carinii belongs to the fungus, with lungs as its most common target of invasion. In immunocompetent people, it can be clear out of the body by concurrent actions of cellular immunity and activated macrophages. In AIDS patients, due to their decreased CD4 T cell count and compromised immunity, its clearance ability against Pneumocystis carinii is also decreasing, which enables them to multiply in a large quantity in the alveoli to obstruct the capillaries. Thereafter, large quantity of foamy substances exudates from the alveolar cavity, together with inflammatory cells infiltration and pulmonary interstitial fibrous tissue proliferation, causes a serious of clinical manifestations and X-ray demonstrations.
24.4.2 Pathophysiologic Basis
By the naked eyes observation, the lung tissue has parenchymal changes. In some serious cases, the lungs are swelling and enlarged, with increased weight. The lungs are solid like the liver, in brown, with increased resistance during dissections. The float and sink test demonstrates positive findings. Microscopy demonstrates interstitial pneumonia and alveolar pneumonia, which are characterized by filling of pink foamy or honeycomb liked material in the dilated terminal bronchioles and in the alveolar cavities. The pink foamy or honeycomb liked material contains piles of worms and their disintegrated components; shed alveolar epithelial cells, lymphocytes, plasmocytes, eosinophils, histocytes or alveolar macrophages. There are also congestion and thickening of the pulmonary interstitium with accompanying infiltration of macrophages, lymphocytes and plasma cells. In the serious cases, the lung tissue has parenchymal changes, which are caused by large quantity proliferation of pneumocystis carinii in the alveoli. The infiltration is predominated by plasma cells in infants, and lymphocytes in children, with findings of macrophages and eosinophils.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree