Ankle
Anthony Wilson
John H. Harris Jr.
GENERAL CONSIDERATIONS
The ankle includes the distal end of the tibia, the fibula, and the talus. The medial and lateral malleoli, together with the horizontal plate of the distal articulating surface of the tibia, constitute the ankle mortise that receives the dome-shaped superior articulating surface of the talus. Although the talus is intimately involved in the ankle joint, it is one of the tarsal bones, and primary injuries of the talus are discussed in Chapter 22, Foot and Heel. Only those talar injuries associated with primary injuries of the ankle are discussed in this chapter.
The radiographic evaluation of acute lesions of the ankle requires accurate clinical assessment of the site of the injury. Conditions affecting the heel and foot, which may produce symptoms referable to “the ankle,” may not be recorded on ankle views and, thus, may be overlooked. The foot, heel, and ankle are distinct anatomic regions. Logically, then, each region requires particular radiographic projections that are usually inappropriate for the proper radiographic examination of the adjacent anatomic region.
Acknowledgement of the basic ligamentous anatomy of the ankle is fundamental to an understanding of the pathophysiology of ankle injuries and the clinical significance of the radiographic appearance of the skeletal injuries.
Ligamentous Anatomy
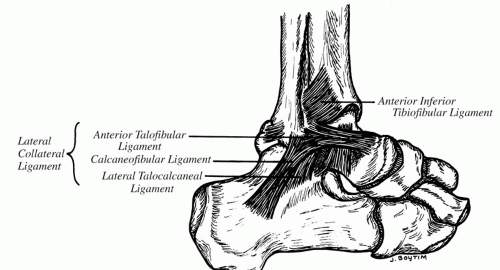
Laterally (Fig. 21.1), the anterior and posterior talofibular ligaments, together with the calcaneo-fibular ligament, constitute the lateral collateral ligament. The anterior and posterior talofibular ligaments extend horizontally from the anterior and posterior cortical surfaces of the fibula to the talus. The calcaneofibular ligaments extend inferoposteriorly from the tip of the lateral malleolus to the lateral surface of the body of the os calcis.
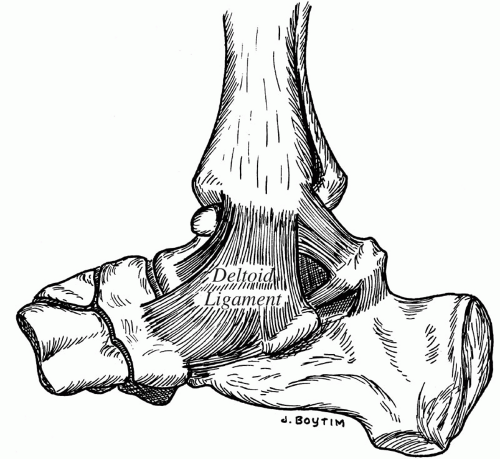
The medial collateral deltoid ligament (Fig. 21.2) is stronger and denser than the lateral collateral ligament and consists of superficial and deep fibers loosely arranged into three groups. These groups extend from the lateral malleolus to the tarsal navicular, the sustentaculum tali of the os calcis, and the talus.
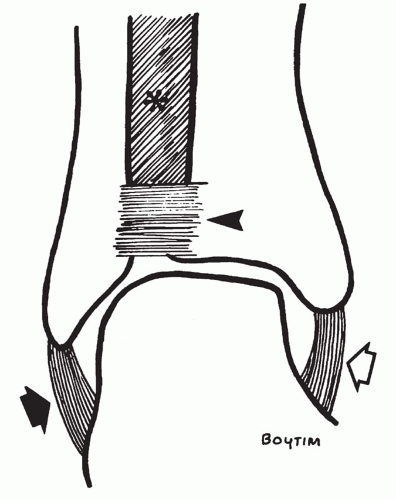
Distally, the tibia and fibula are united by the anterior and posterior tibiofibular ligaments; the interosseous ligament, which is the distal extension of the interosseous membrane; and the interosseous membrane itself (Fig. 21.3). Even from this brief description, it must be apparent that the ligaments of the ankle are integral to the anatomy of the ankle joint. The presence of specific ligamentous injury about the ankle is deducible from the location and orientation of malleolar fractures. Identification of the disrupted and intact ligaments should be included as part of the radiologic report of ankle injuries.
RADIOGRAPHIC EXAMINATION
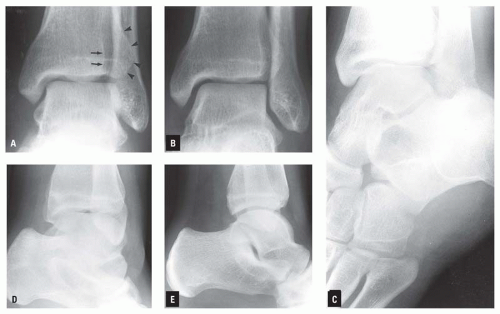
The routine radiographic examination of the ankle should include anteroposterior (AP), “mortise” internally rotated oblique, and lateral projections (Fig. 21.4), unless the patient’s condition
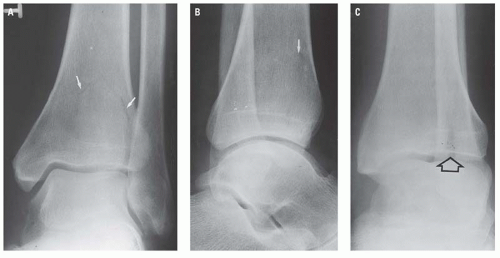
dictates a more limited AP and lateral examination. Oblique views, as included in the routine radiographic examination, can be useful in identifying minimally displaced fractures that are frequently identified or confirmed only by these projections (Figs. 21.5 and 21.6).
dictates a more limited AP and lateral examination. Oblique views, as included in the routine radiographic examination, can be useful in identifying minimally displaced fractures that are frequently identified or confirmed only by these projections (Figs. 21.5 and 21.6).
The oblique projections of the ankle are obtained by rotation at the hip because rotation is not a physiologic function of either the ankle or the knee. The internally rotated oblique projection (e.g., the mortise view) requires only approximately 10 degrees of internal rotation at the hip or sufficient internal rotation so that the lateral malleolus is on the
same horizontal plane as the medial malleolus and both are parallel to the x-ray tabletop. The mortise view is the true AP projection of the ankle joint. Oblique projections,1 plain radiograph tomography (Fig. 21.7), computed tomography (CT), or magnetic resonance imaging (MRI) may be required to identify minimally displaced ankle fractures.
same horizontal plane as the medial malleolus and both are parallel to the x-ray tabletop. The mortise view is the true AP projection of the ankle joint. Oblique projections,1 plain radiograph tomography (Fig. 21.7), computed tomography (CT), or magnetic resonance imaging (MRI) may be required to identify minimally displaced ankle fractures.
RADIOGRAPHIC ANATOMY
The osseous and ligamentous anatomy of the ankle is described and illustrated earlier. It is important to remember that the ankle mortise is composed not only of the malleoli and horizontal plate of the distal articulating surface of the tibia plafond, but also of the very important ligamentous structures that are not visible on plain radiographs.
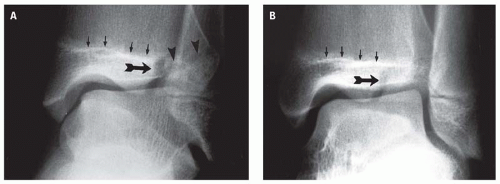
In the straight AP view of the ankle, the lateral malleolus, lying slightly posterior in the fibular notch of the lateral aspect of the distal end of the tibia, is superimposed on the lateral aspect of the body of the talus. In this projection, therefore, the talofibular joint space cannot be adequately evaluated. The need to visualize the talofibular space and to be able to compare it with the talotibial medial space, to obtain an unobstructed view of the lateral margin of the talar trochlea dome, and to determine the relationship of the proximal talar articulating surface to the plafond have all prompted the routine use of the mortise view. In this projection, the lateral surface of the talar body and the cortex of the posterior margin of the fibular notch should normally be on approximately the same vertical plane (Fig. 21.4B). In the lateral projection (Fig. 21.4C), the concavity of the distal tibial articulating surface and the convexity of the talar trochlea are normally congruous.
The optimum lateral radiograph of the ankle results when the part is positioned so that the malleoli are directly superimposed on each other (Fig. 21.4C). This view should include the entire os calcis and the bones of the midfoot, including the base of the fifth metatarsal. Although neither the calcaneus nor the fifth metatarsal is a component of the ankle, each must be consciously studied for the presence of a fracture that may have been clinically interpreted as an injury to the ankle. For this reason, it is particularly important that the base of the fifth
metatarsal be included in all radiographic examinations of the ankle. Fracture of the base of the fifth metatarsal (Fig. 21.8) is commonly misdiagnosed as an ankle fracture clinically, and the patient referred for radiographic examination of the ankle. In these circumstances, if the midfoot is not included on the ankle examination, the fifth metatarsal fracture could be missed.
metatarsal be included in all radiographic examinations of the ankle. Fracture of the base of the fifth metatarsal (Fig. 21.8) is commonly misdiagnosed as an ankle fracture clinically, and the patient referred for radiographic examination of the ankle. In these circumstances, if the midfoot is not included on the ankle examination, the fifth metatarsal fracture could be missed.
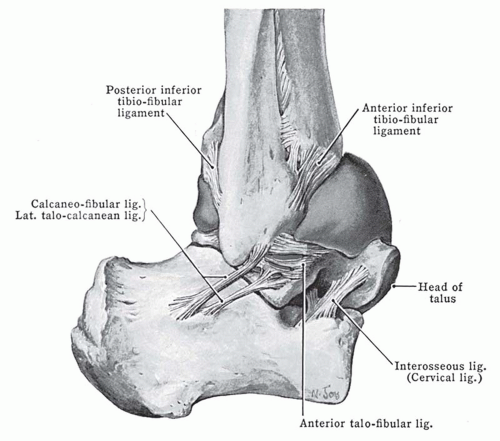 Figure 21.9. Note the anterior bulge of the distended capsule of the ankle joint. (From Anderson JE. Grant’s Atlas of Anatomy. 6th ed. Baltimore, MD: Williams & Wilkins; 1972, used with permission.) |
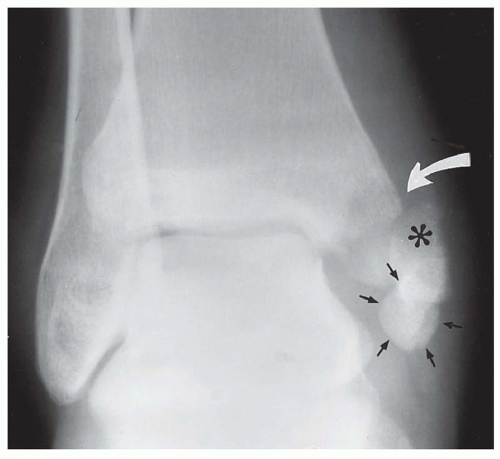
The articular capsule of the ankle surrounds the joint. It is attached to the margin of the distal tibial articulating surface, the malleoli, and extends distally to attach onto the neck of the talus. Laterally, the capsule attaches on the fibula near the lateral malleolar fossa (Fig. 21.9).2 Thus, posttraumatic distention of the ankle joint capsule, which may be visible on a properly exposed lateral ankle radiograph (Fig. 21.10), should be considered indicative of an intra-articular fracture of the distal tibia, the malleoli, or the talar body until specifically excluded by any of the appropriate imaging modalities, including MRI.
The radiographic appearance of the normal child’s ankle is seen in Figure 21.11. The distal tibial epiphysis appears during the 2nd year of life and fuses in the
18th year. The distal fibular epiphysis appears at age 2 and fuses at age 20. Infrequently, the tip of the medial malleolus arises from a separate ossification center. The radiographic characteristics of this apophysis, its relationship to the epiphysis, and its frequent bilaterality help distinguish this normal variant from an avulsion fracture fragment (Fig. 21.12).
18th year. The distal fibular epiphysis appears at age 2 and fuses at age 20. Infrequently, the tip of the medial malleolus arises from a separate ossification center. The radiographic characteristics of this apophysis, its relationship to the epiphysis, and its frequent bilaterality help distinguish this normal variant from an avulsion fracture fragment (Fig. 21.12).
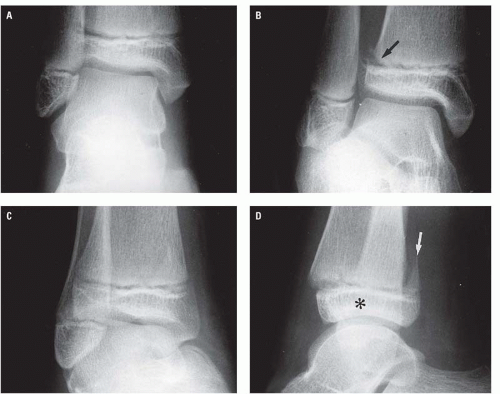
 Figure 21.10. Distended ankle joint capsule (solid arrows) in an adolescent with a minimally displaced physeal injury (open arrow). |
RADIOGRAPHIC MANIFESTATIONS OF TRAUMA
Extracapsular soft tissue swelling about the ankle joint is discernible in a properly exposed radiograph. Although this is a nonspecific finding and is frequently present without associated skeletal trauma, it may signal a subtle fracture (Fig. 21.13). The radiographic distinction between extra-articular soft tissue swelling and joint capsular distention and its significant posttrauma is shown in Figure 21.14.
Physeal Injuries
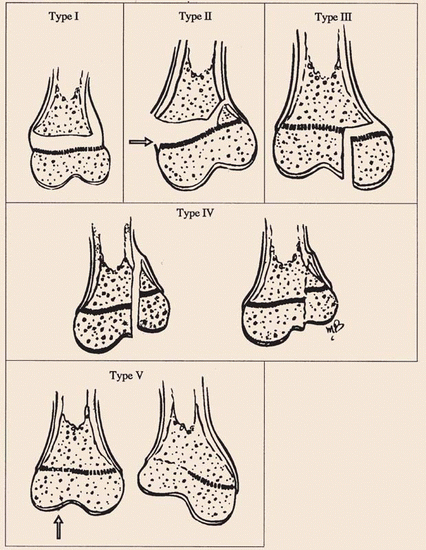
Epiphyseal-physeal injuries, which commonly involve the ankle, are designated according to the Salter-Harris classification (Table 21.1).3, 4 The distal tibial
epiphysis is the single most common site of physeal injury.5 Types III and IV occur more commonly at the ankle than at any other site.
epiphysis is the single most common site of physeal injury.5 Types III and IV occur more commonly at the ankle than at any other site.
TABLE 21.1 Salter-Harris Classification of Physeal Injuries | ||
|---|---|---|
|
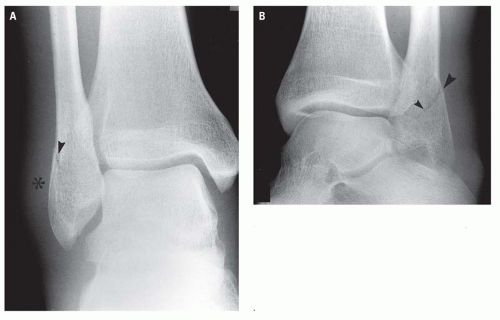
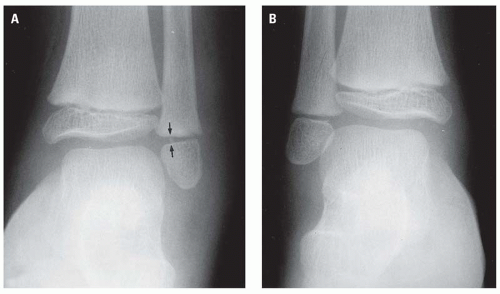
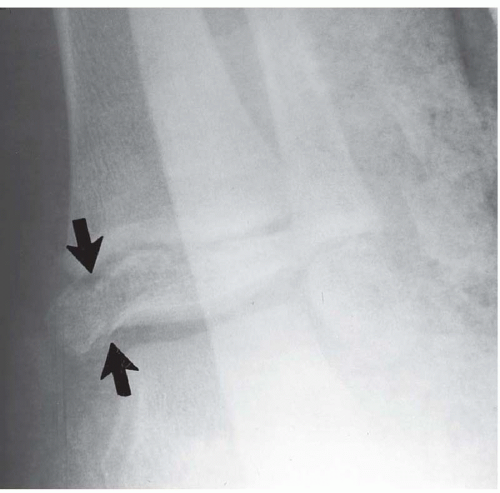
Type I epiphyseal injury, which occurs most commonly in young children, was originally described by Salter as being an epiphyseal separation without a metaphyseal or epiphyseal fracture. Typically, the momentarily separated epiphysis returns to an anatomic or type position with respect to the adjacent metaphysis by the intact periosteum. For this reason, the type I physeal injury is difficult to recognize radiographically. The most striking radiographic sign of type I injury is soft tissue swelling adjacent to the physis and minor uniform or eccentric widening of the physis itself (Figs. 21.15 and 21.16). In displaced type I physeal injuries, the periosteum is attenuated or disrupted, permitting epiphyseal displacement. The periosteum is usually disrupted on the convex side while remaining intact on the concave side of the epiphyseal displacement. Occasionally, a tiny fragment of bone is pulled off the margin of the metaphyseal or epiphyseal surface of the physis. The presence of such a fragment, usually situated in the lateral aspect of the physis between the metaphyseal and epiphyseal surfaces, together with widening of the physis and adjacent soft tissue swelling, establishes a type I physeal injury (Fig. 21.17). This tiny avulsion fracture fragment, although not included in the original Salter-Harris classification, is very commonly visible and is very helpful in the
radiologic identification of the type I physeal injury. The tiny separate fragment has none of the characteristics of the metaphyseal component of the type II physeal injury. Consequently, it seems reasonable to include this type of avulsion fracture as a variant of the type I injury.
radiologic identification of the type I physeal injury. The tiny separate fragment has none of the characteristics of the metaphyseal component of the type II physeal injury. Consequently, it seems reasonable to include this type of avulsion fracture as a variant of the type I injury.
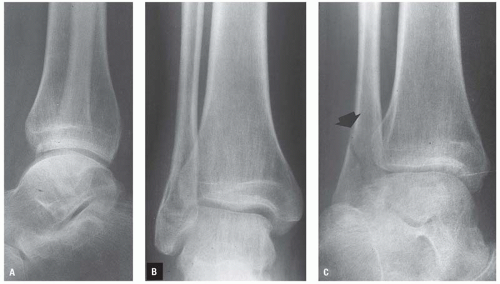
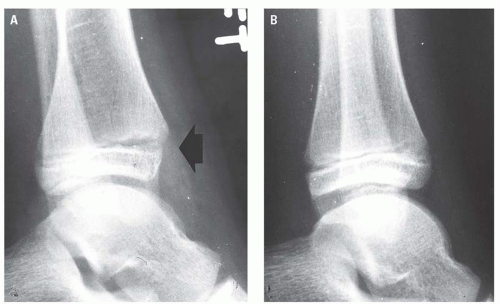
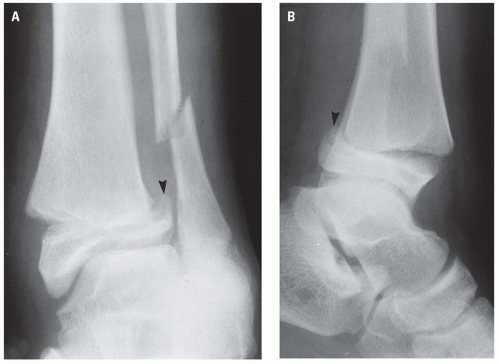
Type II physeal injury consists of an oblique fracture extending through the metaphysis into the physis with separation through the remainder of the physis. The triangular metaphyseal fragment, together with the intact epiphysis, constitutes the distal fragment of the type II injury (Fig. 21.18). The type II injury is by far the most common of the physeal injuries and usually occurs in older children. The prognosis for normal growth is excellent. Type II injuries of the ankle are usually obvious radiographically but may be subtle and not discernible on all ankle views (Fig. 21.19).
Physeal injuries are limited to a single bone but may also be associated with a fracture (Fig. 21.20) or physeal injury of an adjacent bone.
Physeal injuries are limited to a single bone but may also be associated with a fracture (Fig. 21.20) or physeal injury of an adjacent bone.
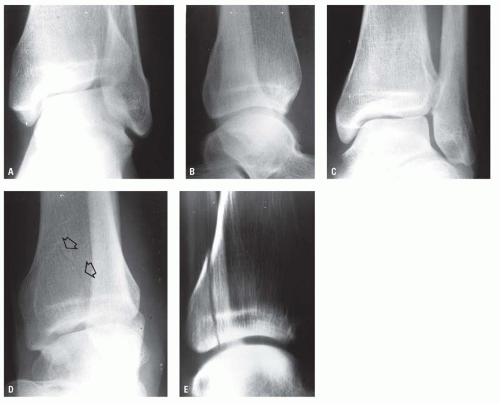
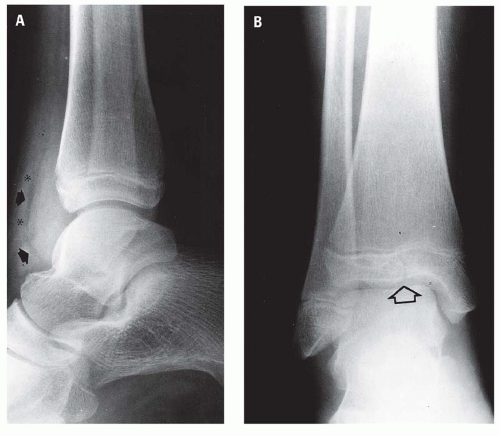
Type III injury is uncommon, is usually seen in the distal tibial epiphysis, and is entirely intracapsular. The prognosis of normal growth is good, provided the blood supply to the separated portion of the epiphysis has not been disrupted. Radiographically, the injury consists of a vertical fracture line that extends perpendicularly through the epiphysis from its articulating surface to the physis and then along the physis to its margin. Figure 21.21 illustrates a minimally displaced Salter-Harris III physeal injury in a very young child.
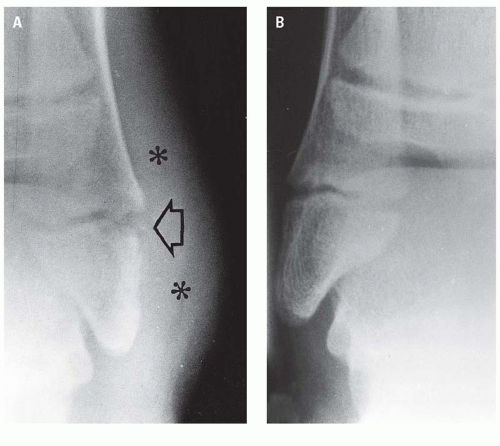
The biplane fracture of Tillaux6 (Fig. 21.22) is a variant of the type III injury of the distal tibial epiphysis. The vertical epiphyseal fracture, situated in the lateral aspect of the epiphysis, occurs in older children in whom fusion of the medial portion of the distal tibial physis is more advanced than the lateral (Fig. 21.23). The mechanism of injury has been described as eversion or external rotation. The epiphyseal injury is an avulsion fracture produced by the intact anterior and posterior tibiofibular ligaments. The age of the patient usually 12 to 14 years, radiographic evidence of fusion of the medial portion of the distal tibial physis, and lateral displacement of the epiphyseal fragment distinguishes the biplane fracture of Tillaux (Fig. 21.24) from the typical type III injury of the distal tibial epiphysis.
The type IV and the rare type V physeal injuries differ in two significant aspects from the other Salter-Harris injuries, in that each is caused by a compressive rather than a shearing or rotational force and each has a high propensity for growth arrest secondary to premature or uneven physeal fusion. In both type IV and type V injuries, premature physeal closure may result from physical crushing of the physeal cells, impairment of their blood supply,
or damage to the metaphysis and epiphysis with the resultant formation.7 Additionally, peculiar to the type IV injury is growth arrest secondary to fusion of the epiphyseal component of the separate fragment to the metaphysis of the major fragment. This is described in more detail later.
or damage to the metaphysis and epiphysis with the resultant formation.7 Additionally, peculiar to the type IV injury is growth arrest secondary to fusion of the epiphyseal component of the separate fragment to the metaphysis of the major fragment. This is described in more detail later.
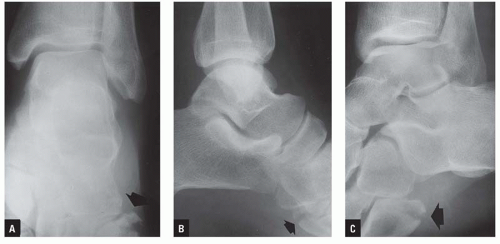
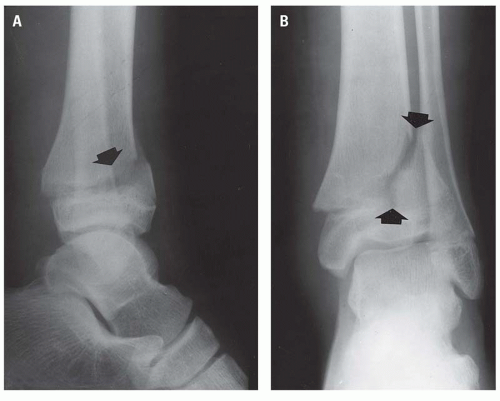
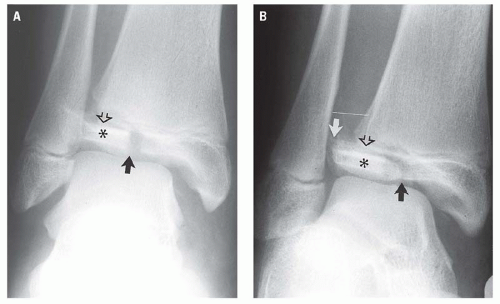
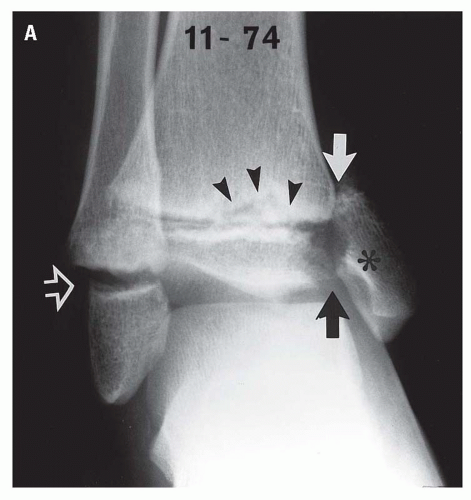
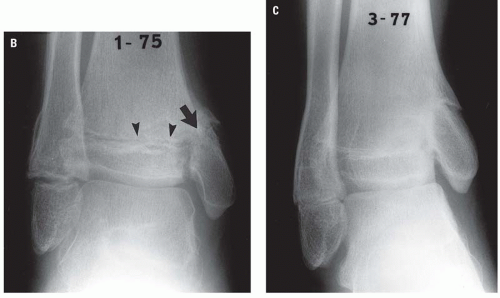
Type IV injury consists of a vertical fracture extending through the entire thickness of the medial third of the distal tibial epiphysis, across the physis, and continuing vertically through the metaphysis to exit through the medial metaphyseal cortex (Fig. 21.25). The entire separate fragment, therefore, includes the
medial malleolus with variable amounts of the medial portion of the plafond, the physis, and the metaphysis as a single unit. The mechanism of injury is primarily axial-loading vertical compression and inversion of the foot, causing the talus to impact against the medial malleolus. Continued inversion and/or vertical compression causes proximal displacement of the separate fragment (Fig. 21.26). The vertical compression component invariably results in a Salter-Harris type V injury of the physis itself. If the separate fragment remains proximally displaced and assuming there is no other distal tibial physeal injury, growth arrest will occur as the result of the epiphyseal component fusing with the metaphysis of the major fragment (Fig. 21.26B,C). “Perfect” open reduction and internal fixation7, 8 offers the best chance of healing without growth arrest. However, as mentioned earlier and as seen in the patient represented in Figure 21.26, a crushing injury Salter-Harris type V concurrently involving the distal tibial physis will contribute in large measure to the premature closure of the distal tibial physis.
medial malleolus with variable amounts of the medial portion of the plafond, the physis, and the metaphysis as a single unit. The mechanism of injury is primarily axial-loading vertical compression and inversion of the foot, causing the talus to impact against the medial malleolus. Continued inversion and/or vertical compression causes proximal displacement of the separate fragment (Fig. 21.26). The vertical compression component invariably results in a Salter-Harris type V injury of the physis itself. If the separate fragment remains proximally displaced and assuming there is no other distal tibial physeal injury, growth arrest will occur as the result of the epiphyseal component fusing with the metaphysis of the major fragment (Fig. 21.26B,C). “Perfect” open reduction and internal fixation7, 8 offers the best chance of healing without growth arrest. However, as mentioned earlier and as seen in the patient represented in Figure 21.26, a crushing injury Salter-Harris type V concurrently involving the distal tibial physis will contribute in large measure to the premature closure of the distal tibial physis.
The “triplanar” fracture5, 9, 10 is a variant of the Salter-Harris type IV injury7 in that it includes a fracture of the epiphysis, separation of a portion of the physis, and a fracture through the distal tibial metaphysis, as does the type IV injury. The triplanar fracture differs
from the type IV in that the triplanar injury occurs in three planes, whereas the type IV occurs in only one. The sites of disruption of the triplanar fracture occur in the sagittal plane epiphysis, the axial plane physis, and the coronal plane metaphysis. Triplanar fractures may occur in a two-part variety, in which all the components of the separate fragment exist as an intact unit (Fig. 21.27), or in a three-part configuration (Fig. 21.28),5 in which the epiphyseal component is a separate fragment (e.g., the third part) (Fig. 21.29).
from the type IV in that the triplanar injury occurs in three planes, whereas the type IV occurs in only one. The sites of disruption of the triplanar fracture occur in the sagittal plane epiphysis, the axial plane physis, and the coronal plane metaphysis. Triplanar fractures may occur in a two-part variety, in which all the components of the separate fragment exist as an intact unit (Fig. 21.27), or in a three-part configuration (Fig. 21.28),5 in which the epiphyseal component is a separate fragment (e.g., the third part) (Fig. 21.29).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree