Systems-related
Technical
Workflow
Construction
Culture of safety
Equipment design
Safety compliance
Ease of use
Protocols and policies
Safety features
Staffing
Work environment
Work hours
Equipment maintenance
Ergonomics
Engineering
Leadership
Department design
Supervision
Hardware
Clinical governance
Software
Table 7.2
Examples of human failures that may occur in an imaging department
Patient | Practitioners |
|---|---|
Compliance | Training |
Co-operation | Experience |
Co-morbidities | Skills |
Extent of illness | Knowledge |
Anatomic factors | Supervision |
Habitus | Interpretation |
Hardware | Communication |
One of the most important causes of error in radiology is failure of communication between referring physicians, reception/secretarial staffs, radiographers, radiologists and others who form part of the radiology communication loop. System-related failures of communication can occur at many points in a patient’s interaction with the imaging department from the clinical information provided by the referrer, patient preparation instructions, image acquisition and processing, radiologist interpretation and reporting of the images through to communication of results to the referring physician (Table 7.3). System errors occur due to higher-level decision-makers’ or managers’ failures and, although not immediately apparent at the time of an adverse event, have generally made a major contribution to the error occurring.
Table 7.3
Steps where system failures of communication may occur
1. Physician requests investigation |
2. Radiology protocoling and scheduling of request |
3. Image acquisition and post-processing |
4. Image archiving to PACS |
5. Images appear on appropriate worklist |
6. Radiologist interpretation of images |
7. Report generation |
8. Report checking or double reading |
9. Result communication to referring physician |
10. Physician electronic acknowledgement of receipt of report |
7.4.2 Active Failures
An active failure is usually person-related and generally immediately apparent. It is due to human error by a radiologist (to be discussed in more detail later in this chapter), but it is occasionally attributable to patient-related or external failure. The patient’s build or the presence of metal hardware may degrade image quality; the patient may be unable to comply with instructions due to youth, advanced age or language difficulties; or they may move during image acquisition. External causes such as complete loss of electrical power or natural disasters, such as flood or earthquake, are rare causes of active failure.
7.5 Radiologist Error
Guidelines issued by professional bodies governing radiological practice recommend that all imaging procedures should include an expert opinion from a radiologist in the form of a written report. Image interpretation is subjective and although variation between radiologists may be due to error on the part of one observer, it may be due to a genuine difference of opinion about the correct interpretation. As not all differences in opinion constitute an error, the term “reporting discrepancy” has been increasingly applied in radiology. The definition of what constitutes an error is a matter of “expert opinion”, and a radiologist can be judged to have made an error if he or she fails to reach the same conclusion as that reached by a group of their peers. In order for a report to be incorrect, it must be possible for a “correct” report to be generated.
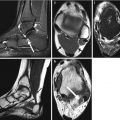
Robinson (1997) has produced a helpful template (Fig. 7.1) describing the relationship between degrees of abnormality, doubt and certainty and error and variation. Case A where a major abnormality is recognised with certainty can be considered to be an “easy” case. Case B where a minor but clearly demonstrated finding (e.g. a small lung nodule on CT) and case C where a major but difficult to appreciate finding (e.g. an impacted femoral neck fracture) is present are considered more “difficult” cases. The most difficult cases (represented by case D) are those where minor degrees of abnormality are perceived with low levels of certainty. Somewhere between the obvious error and the inevitable difference of opinion is an arbitrary division defining the limit of professional acceptability. The position of this division or watershed between error and acceptable variation is defined by the performance standards of radiologists set by their professional bodies and interpreted by the law courts in negligence and malpractice cases.
Fig. 7.1
Proposed relationship between severity and certainty in recognising abnormalities. Errors occur when “easy cases” (e.g. A) are wrongly interpreted; different readings of “difficult” cases (e.g. D) represent acceptable observer variation (Robinson 1997)
7.5.1 Classification of Radiologist Error
In image interpretation, the most common error is that of perception, i.e. a visible abnormality is not appreciated resulting in a false-negative report. Perceptual errors tend to be sporadic and are four times more common than errors of interpretation when an abnormality is observed but misinterpreted (Donald and Barnard 2012). False-negative errors are five times more common than false-positive errors (Kundel 1989). Radiological error can be further subdivided using the scheme initially published by Smith (1967) and subsequently adapted by Renfrew et al. (1992) and is summarised in Table 7.4.
Table 7.4
Classification of radiological error
Class | Cause of error | Explanation and examples | Decision-analysis term |
|---|---|---|---|
I | Complacency | Errors of overreading and misinterpretation in which a finding is appreciated but is attributed to the wrong cause | False-positive error |
II | Faulty reasoning | Errors of overreading and misinterpretation in which the finding is appreciated and interpreted as abnormal but is attributed to the wrong cause. Misleading information and a limited differential diagnosis are included in this category | True-positive reading but misclassification |
III | Lack of knowledge | The finding is seen but is attributed to the wrong cause because of a lack of knowledge on the part of the viewer | True-positive reading but misclassification |
IV | Under-reading | The finding is missed. Under-reading may result from failure to isolate important material or from satisfaction of search | False-negative error |
V | Poor communication | The lesion is identified and interpreted correctly but the message fails to reach the clinician | |
VI | Miscellaneous | The lesion was not present on the image obtained, even in retrospect. This may be secondary to limitations of the examination or to an inadequate examination | False-negative error |
VII | Complications | Untoward events happened during the course of examination, most frequently encountered during invasive procedures |
7.5.2 Causes of Radiologist Error
Many factors contribute to radiologist error, including variables such as level of radiologist alertness or fatigue, workload and speed of reporting, viewing conditions and distraction factors.
7.5.2.1 Workload
Excessive workload is a proven factor that increases the likelihood of perceptive error. Most abnormal findings on radiographs are found during the first few seconds of searching the image, with the number of true-positive findings dropping rapidly after a short time. A radiologist who spends only a few seconds interpreting an image, however, is gambling that a large part of the image shows normal findings, and it has been shown that reducing the viewing time of chest radiographs to less than 4 s increases lesion miss rate (Oestmann et al. 1988). Experimental studies recording the eye movements of radiologists searching radiographs for subtle nodules found that about 30 % of misses were due to incomplete scanning, 25 % to failure of recognition and 45 % to wrong decisions (Kundel et al. 1978). Interestingly, the same investigators also showed that prolonged scrutiny of one specific area on the image (“visual dwell”) increased both false-negative and false-positive errors (Kundel et al. 1989). There has been at least one instance where a radiologist in the United States has been sued for missing a breast cancer on a mammogram because “the defendant radiologist read too many X-ray examinations on the day in question, demonstrating a wanton disregard of patient well-being by sacrificing quality patient care for volume in order to maximise revenue” (Berlin 2000a).
A recent study of radiologists’ visual accommodation and performance showed that the ability to focus and detect fractures diminished at the end of the working day (Krupinski et al. 2010), and a 1997 study looking at error rates in the interpretation of abdominal CT showed a more than doubling when a radiologist reported more than 20 studies per day (Bechtold et al. 1997). The Royal College of Radiologists (2012a) has recently published guidance on radiologists’ reporting figures, and their indicative modality-based figures, estimated for one hour of uninterrupted time with no confounding factors, are listed in Table 7.5.
Table 7.5
Indicative modality-based figures for 1 h of uninterrupted time with no confounding factors recommended by Royal College of Radiologists (2012a)
Modality (suggested average values/hour of uninterrupted work) | Activity/hour with no confounding factors |
|---|---|
Plain film reporting (examinations) | 30–60 |
Checking of reports (e.g. for trainees) | 6–12 |
CT/MRI | 3–6 |
Complex CT/MRI | 1–2 |
Cardiac MRI | 1–2 |
PET CT | 1–2 |
Mammography – symptomatica | 4–6 |
Breast workup (e.g. mammo/US/biopsy) | 2–3 |
Barium study | 2–4 |
USb | 4–6 |
Complex US ± biopsy | 2–3 |
Interventional proceduresc | Agreed at job planning discussion |
7.5.2.2 Satisfaction of Search
This describes the situation in which the detection of one radiographic abnormality results in a premature termination of the search for further findings, with a likelihood of overlooking more subtle abnormalities (Berbaum et al. 1990). A study comparing lesion detection rates in radiographs with single abnormalities compared with those with multiple abnormalities found similar detection rates for one finding in both groups, but the detection rate for the second and third abnormalities in the multiple finding cases was about halved (Ashman et al. 2000).
7.5.2.3 Complexity of Examination
Technological advances have reduced the acquisition time while increasing the number of images for CT examinations. Despite concurrent technological advances in reporting hardware and software including PACS, the ability to scroll through stacks of CT images and the ability to use 3D visualisation CT scans are disproportionately over-represented in published series of perceptive and interpretative error (McCreadie and Oliver 2009; Donald and Barnard 2012). This is due not only to the large number of clinically unsuspected findings revealed by CT such as bowel and pancreatic cancers, bone lesions, lung nodules and thromboembolic diseases but also of unexpected lesions, usually benign and sometimes described as “incidentalomas”.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree