, Gustav Andreisek2 and Erika J. Ulbrich2
(1)
Phoenix Diagnostic Clinic, Cluj-Napoca, Romania
(2)
Institute of Diagnostic and Interventional Radiology, University Hospital Zürich, Zürich, Switzerland
10.1 Anatomy and Normal MRI Appearance
On MR imaging of the knee, the most important vascular and nervous structures that are identified are the popliteal neurovascular bundle and the common peroneal nerve. However, several structures around the knee are vascularized or innervated by arteries or nerves that are not within the field of view of a normal knee MRI examination. The vascularization and innervation of the knee structures are detailed in Table 10.1.
Anatomical structure | Vascularization | Innervation |
|---|---|---|
Anterior cruciate ligament | Vascular synovial envelope from the middle genicular artery | Tibial nerve; nociceptive and proprioceptive receptors |
Posterior cruciate ligament | Mainly from the middle genicular artery; inferior medial and lateral genicular arteries also vascularize the ligament via the fat pad | Tibial nerve; nociceptive and proprioceptive receptors |
Menisci | Perimeniscal plexus from branches of lateral and medial genicular arteries; blood reaches the outer 10–33 % of the body of menisci | Tibial nerve; nociceptors and mechanoreceptors reaching the outer 66 % of the meniscus |
Cartilage | Devoid of vascularity | Devoid of innervation |
Capsule | Poorly vascularized | Highly innervated: nociceptors and mechanoreceptors |
Synovia | Highly vascularized from periarticular anastomotic plexus | Poorly innervated (insensitive to pain) |
Muscles around the knee | ||
Quadriceps muscle and tendon | Descending genicular artery and both superior genicular arteries | Femoral nerve |
Sartorius and semimembranosus | Descending genicular artery, branches of popliteal artery, and superior and inferior genicular arteries | Femoral nerve |
Gracilis | Branches of popliteal artery and inferior genicular artery distally | Obturator nerve |
Semitendinosus | Branches of popliteal artery and inferior genicular artery distally | Tibial nerve |
Medial and lateral head of the gastrocnemius, popliteus | Popliteal artery (sural branches), medial and lateral inferior genicular arteries, posterior tibial artery, and peroneal artery | Tibial nerve |
Biceps femoris | Popliteal artery (muscular branches) | Tibial nerve |
Plantaris | Popliteal artery (sural branches), posterior tibial artery, and peroneal artery | Tibial nerve |
Bones | ||
Patella | Five to six arteries forming an anastomotic network called Rete patellae; the descending genicular artery, superior and inferior genicular arteries, and anterior tibial recurrent artery contribute to this network | Femoral nerve through its vastus medialis and lateralis branches |
Distal femur | Superior and inferior genicular arteries (lateral condyle) and medial genicular artery and popliteal artery (medial condyle) | Tibial nerve |
Proximal tibia | Anterior and posterior tibial arteries | Tibial nerve |
Tibiofibular joint | Anterior tibial artery | Common peroneal nerve |
The popliteal neurovascular bundle consists of the popliteal artery, the popliteal vein, sural veins, and the tibial nerve. On “conventional” axial MR images, the neurovascular bundle is identified posterior to the intercondylar femoral fossa, between the lateral and the medial heads of the gastrocnemius (Fig. 10.1). The common peroneal nerve is located superficial and posterior to the lateral head of the gastrocnemius and adjacent to the medial margin of the biceps femoris (Fig. 10.1).


Fig. 10.1
The popliteal neurovascular bundle in a 40 year old male. Axial proton-density (PD) image shows the popliteal artery (large arrow), the tibial nerve (small arrow), and the common peroneal nerve (curved arrow)
10.1.1 Arteries
The popliteal artery is the continuation of the femoral artery. It descends slightly lateral to the intercondylar fossa, anterior to the popliteal vein and the tibial nerve, and it ends at the inferior margin of the popliteus muscle where it divides into the anterior and posterior tibial arteries (Fig. 10.2). Some authors use the term tibial-peroneal trunk for the arterial segment located between the origin of the anterior tibial artery which arises first and the origin of the posterior tibial artery and peroneal arteries [4, 5]. The length of the tibial-peroneal trunk is approximately 30 mm but can vary significantly [5]. Awareness of the anatomy of the popliteal artery, its variations, and its branches is important for radiologists and surgeons especially in complex traumatic injuries of the knee, such as dislocations, with a high likelihood for vascular involvement. The popliteal artery diameter is 7–8 mm and the length is approximately 190 mm [5]. Variants of branching pattern are rare. An important variant is the aberrant anterior tibial artery when the origin of the artery is high (proximal) and the tibial anterior artery courses inferiorly along the anterior surface of the popliteus muscle [6, 7]. The aberrant artery is at high risk of injury during surgery [6]. Another variant is the so-called trifurcation pattern. In this variant, the anterior tibial artery, the posterior tibial artery, and the peroneal arteries originate together from the popliteal artery [5].


Fig. 10.2
The anterior and posterior tibial arteries in a 44 year old female. Axial proton-density (PD) image shows the anterior tibial artery (large arrow) and posterior tibial artery (small arrow). Note the popliteal vein adjacent to the anterior tibial artery (curved arrow)
The middle genicular artery originates from the anterolateral surface of the popliteal artery in the popliteal fossa, 3–5 cm proximal to the joint line either alone or having a common origin with the lateral genicular artery [8]. It is 3–5 cm long and is situated between the popliteal artery anteriorly and the knee capsule posteriorly [8]. The artery is accompanied by two venae comitantes.
The superior medial genicular artery originates primarily from the femoral artery. It descends under the semimembranosus and semitendinosus muscle above the medial head of the gastrocnemius muscle and bifurcates into a superficial and a deep branch [9]. The deep branch joins the anterior tibial recurrent artery on the level of medial tibial plateau. It ends into and supplies the perimeniscal capillary plexus.
The superior lateral genicular artery arises from the popliteal artery beneath the lateral gastrocnemius muscle and passes under the biceps femoris tendon. It divides into a superficial and a deep branch and forms an anastomotic arch with the medial inferior genicular artery [9].
The inferior medial genicular artery originates from the popliteal artery closed to the origin of the anterior tibial artery [5]. It descends along the upper margin of the popliteus muscle, below the medial tibial plateau, and passes deep to the lateral collateral ligament.
The inferior lateral genicular artery originates from the anterior tibial artery deep to the lateral gastrocnemius muscle and runs laterally adjacent to the anterior aspect of the lateral tibial plateau and above the tibiofibular joint [5, 9]. The artery is situated deep to the lateral collateral ligament and biceps tendon.
The (medial and lateral) sural arteries originate just above the knee joint from the popliteal artery and distribute to the gastrocnemius, soleus, and plantaris muscles [9]. The sural artery is intimately connected to the sural nerve and supplies the skin of the lower and middle leg.
10.1.2 Veins
The popliteal vein is part of the deep vein system of the knee and collects the blood from the four anterior and posterior tibial veins. The popliteal vein is part of the popliteal neurovascular bundle and passes anteromedially in the distal thigh joining the deep femoral vein (Figs. 10.2 and 10.3).
Fig. 10.3
The popliteal vein in a 40 year old male. Sagittal T2-weighted fat-suppressed image shows the popliteal vein (large arrow) posterior to the popliteal artery (small arrow)
The great saphenous vein is part of the superficial venous system of the leg and is situated within the subcutaneous tissue on the anteromedial aspect of the knee region (Fig. 10.4).
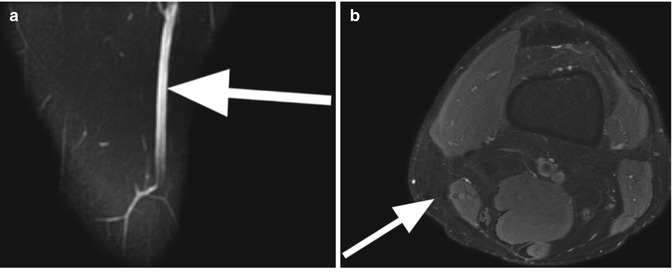
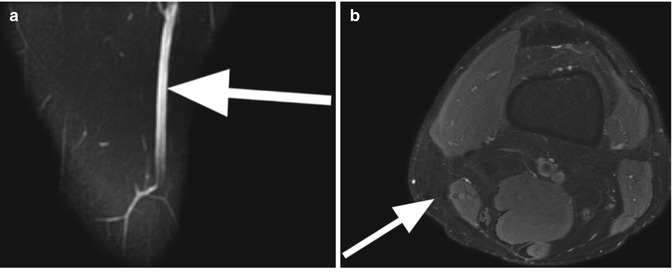
Fig. 10.4
The great saphenous vein in a 40 year old male. Sagittal T2-weighted fat-suppressed image (a) and axial proton-density (PD) image (b) show the great saphenous vein (large arrows in a, b) situated within the subcutaneous tissue on the medial aspect of the knee
The sural veins and the genicular veins accompany the sural and genicular arteries. Usually, there are five genicular veins which provide drainage to the knee.
10.1.3 Nerves
The tibial nerve is one of the two major branches of the sciatic nerve together with the common peroneal nerve. It branches off the sciatic nerve above the popliteal fossa where it is located lateral to the semimembranosus muscle. The tibial nerve descends between the medial and lateral heads of the gastrocnemius muscle and joins the neurovascular popliteal bundle. Within the neurovascular bundle, the tibial nerve is situated posterior to the popliteal artery and vein (Fig. 10.1). In the popliteal fossa, it divides into an articular branch to the knee, a cutaneous branch, and several branches to the calf muscles.
The common peroneal nerve descends from its origin, the sciatic nerve, posterior to the biceps femoris muscle and anterior to the tibial nerve and becomes more superficial at the knee line joint. At this level, the common peroneal nerve is located posterior to the biceps tendon and lateral to the lateral head of gastrocnemius muscle (Fig. 10.5). At the level of the proximal popliteal fossa, it divides into the superficial perineal nerve and the deep peroneal nerve which are both located posterior to the common peroneal nerve.
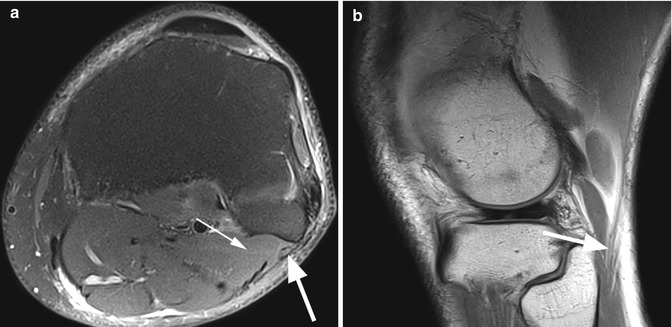
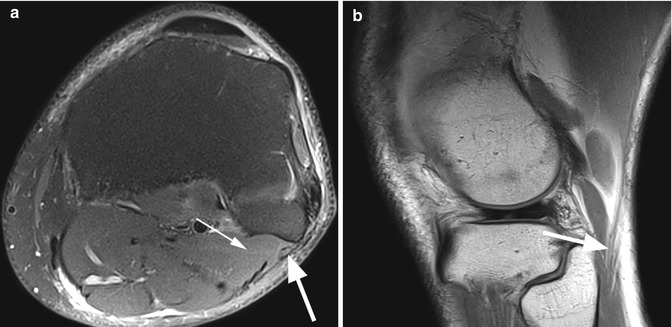
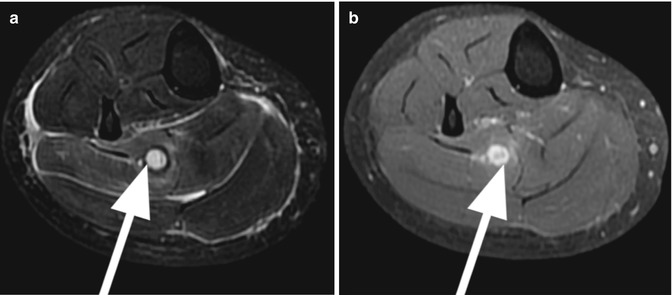
Fig. 10.5
The common peroneal nerve in 55 year old male. Axial proton-density (PD) fat-suppressed image (a) and sagittal proton-density (PD) image (b) show the common peroneal nerve (large arrow in a, b) posterior to the biceps tendon and lateral to the lateral head of gastrocnemius muscle (small arrow in a)
The nerves around the knee supply different groups of muscles of the leg. Knowing this distribution is important for the diagnosis of neuropathies based on indirect signs of muscles denervation (e.g., muscle atrophy) (Table 10.2).
Table 10.2
Innervation of the muscles around the knee
Nerve | Muscles supplied |
|---|---|
Tibial nerve | Posteromedial and posterolateral muscles of the knee: |
Long tendon of biceps muscle | |
Popliteus muscle | |
Gastrocnemius muscle (medial and lateral head) | |
Plantaris muscle | |
Soleus muscle | |
Superficial peroneal nerve | Lateral compartment of the leg: |
Peroneus brevis muscle | |
Peroneus longus muscle | |
Deep peroneal nerve | Anterior compartment of the leg: |
Tibialis anterior muscle | |
Extensor hallucis longus | |
Extensor hallucis brevis |
10.2 MRI Pathological Findings: Arteries
The main knee arteries can be affected by a variety of pathological conditions (Table 10.3). The affected patient population and the etiology of the pathological changes are often distinct, but the clinical signs and symptoms may frequently overlap [10]. MR imaging, including MR angiography, can be a “one-stop-shopping” examination due to the possibility of evaluating the muscle, ligamentous, and bone injuries as well as the vascular pathology in the same time. MR angiography has been shown to be equally effective as angiography in evaluating vascular injury of the knee with fewer complications than angiography [11]. A relatively new MR technique is time-resolved angiography, which provides dynamic imaging of the arterial and venous blood flow within one examination. The technique is based on rapid contrast-enhanced imaging and is based on an undersampling of the k-space with subsequent sharing of k-space information (view-sharing) to reconstruct a full volume data set. After image reconstruction, readers get realistic three-dimensional (3D) angiographic images, which show the arterial inflow, distribution, and venous drainage of the contrast agent. The image update rate defines the temporal resolution of the time-resolved MR angiography. While it is a compromise between image quality and speed, the temporal resolution can be as low as one 3D volume every second (1/s). Typical vendor acronyms for sequences are TREAT (Siemens), TRICKS (GE), and CENTRA (Philips).
Pathological condition | Etiology | Clinical findings |
|---|---|---|
Atherosclerosis and thrombosis | Endothelial injuries followed by atherosclerotic plaque formation | Intermittent claudication, rest pain, muscle atrophy |
Embolism | Most often cardiac source Proximal arterial plaque | Clinical findings of acute ischemia including pain, pulselessness, paresthesia, and pallor |
Aneurysm | Nonspecific | Asymptomatic in most of the cases; rarely, pain in the popliteal fossa |
Connective tissue diseases (e.g., Marfan’s syndrome) | ||
Trauma | ||
Iatrogenic injury due to surgery (false aneurysm) | ||
Artery entrapment syndrome | Abnormal relation to the normal or hypertrophic muscles or to fibrous structures | Arterial pulse that disappears in a particular knee or ankle position; claudication |
Traumatic injuries (occlusion, dissection, arteriovenous fistula) | Trauma | The clinical findings may be confusing; angiography is mandatory in patients with suspected injuries |
Iatrogenic injury due to surgery | ||
Hemangiomas | Benign proliferative tumors of the endothelial cells | Possible palpable and visible soft tissue mass if superficial |
Vascular malformations | Errors of vascular morphogenesis | Possible palpable soft tissue mass if superficial; may grow in time |
10.2.1 Atherosclerosis, Thrombosis, and Embolism
MR angiography (MRA) is a feasible diagnostic imaging option that provides all necessary information for choosing the therapeutic option in patients with peripheral atherosclerotic arterial disease. The popliteal artery is a very important artery for the evaluation of patients with peripheral ischemia because it is targeted for insertion of surgical bypass graft [18]. On MR angiography, popliteal arterial atherosclerosis appears as an irregular stenosis with or without collateral circulation. Post-stenotic dilation may be also present. The most important imaging findings in the diagnosis are the grade of the stenosis and the length of the involved segment. An imaging report should differentiate between a low-grade stenosis (<50 % narrowing) and a high-grade stenosis (>50 % narrowing). The latter is considered a hemodynamically significant lesion [18]. The length of the stenosis is also a significant criterion that influences the choice of treatment. Patients with more than 10 cm stenosis are less likely to benefit from angioplasty procedure [18].
In acute and severe arterial occlusion (embolism or thrombosis), MR angiography is usually not indicated since the patients need a rapid intervention. When is performed, MR imaging may show the enlargement of the vessel and diffuse perivascular edema (Fig. 10.6).