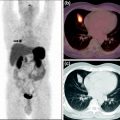
Fig. 1
99mTc-EDDA/HYNIC-TOC SRS and CT before and after neoadjuvant therapy with PRRT in a patient with inoperable midgut tumor (male, 48 years old)
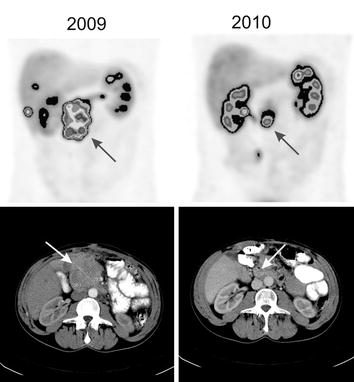
Fig. 2
99mTc-EDDA/HYNIC-TOC SRS and CT before and after neoadjuvant therapy with PRRT in a patient with inoperable pancreatic NET (male, 56 years old)
A group from Australia (Barber et al. 2012) used 177Lu-octreotate as neoadjuvant treatment. There were five patients, four with a primary nonfunctioning pancreatic neuroendocrine tumor and one with a locoregional recurrence of a duodenal tumor. Four patients had disease confined to local/locoregional sites, and one patient had also solitary liver metastases. Four patients with primary PNT were treated with four cycles of 177Lu-DOTATATE with administered activity ranging from 7 to 10 GBq, at 6- to 8-week intervals. The subsequent three cycles of PRRT were administered with a concurrent radiosensitizing dose of infusional 5FU chemotherapy (200 mg/m2/24 h) commencing 4 days prior and continuing for a total of 3 weeks. The remaining patient with a locoregional duodenal NET recurrence was treated with one cycle of 177Lu-DOTATATE, which was administered 3 weeks prior to previously planned external-beam radiotherapy (45 Gy in 25 fractions) to maximize the radiation dose delivered to the tumor. The patient received also concurrent 5FU chemotherapy. At 3 months post treatment, all five patients had scintigraphic response, four had radiological response, and three of the four symptomatic patients responded clinically. All five patients had ongoing treatment response beyond 3 months, including the one whose further tumor shrinkage facilitated curative surgery (6 months after completion of treatment). Complete resection was performed subsequently. Histological examination demonstrated a Ki67 index of 5%, which was lower than in the biopsy before surgery. The patient with distant metastases had ongoing complete scintigraphic and radiological response of the solitary liver metastasis at 18-month follow-up. The remaining patients were deemed unsuitable for curative resection due to medical comorbidities (two patients), ongoing technical surgical difficulties (one patient), and patient choice (one patient).
3 Conclusion
These reports indicate the possibility of utilization of PRRT as neoadjuvant treatment. Most of the patients in those small groups suffered from pancreatic neuroendocrine tumors. The treatment may enable total or partial excision of the tumor, sometimes with liver metastases, despite diverse details of treatment such as different isotopes, total activity of the isotope, or combination with radiosensitizing chemotherapy. The treatment was safe, without significant hematological or renal toxicity. In cases where the tumor was still inoperable after PRRT or only partial response was assessed, the patients also had symptomatic response. Decreasing the tumor size or total excision of the tumor corresponded with prolongation of overall survival. The results of these studies suggest that PRRT may become the preferred approach for treatment of inoperable NETs. All authors stated that PRRT should be started early enough, before disease progression. All studies concluded that PRRT may be used as neoadjuvant treatment in patients with NETs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree