George M. Bridgeforth, Kevin Bozic, and Jay Patel
A 41-year-old man who is positive for the human immunodeficiency virus (HIV) is taking antiretroviral therapy. (He is a cocaine and intravenous drug abuser.) He presents to the emergency department with left hip pain that he sustained after a fall.

CLINICAL POINTS
- Patients may present with hip or groin pain.
- Initial plain radiographs may be negative.
- AVN may take 3 to 4 weeks to appear on standard radiographs.
- Sclerotic and/or cystic changes in the bone with a deformed femoral head may be evident.
- A positive Stinchfield or Faber test indicates intra-articular hip pathology. This may represent degenerative joint disease, acute fracture, metastatic disease, AVN, or a labral tear.
Clinical Presentation
Avascular necrosis (AVN), which is also known as osteonecrosis or aseptic necrosis, usually presents with complaints of severe hip or groin pain. Moreover, it is associated with pain-limited range of motion and gait. Initially, radiographs may be negative; findings of AVN appear on standard radiographs several weeks later. AVN may be traumatic, with the risk increasing following severe, acute trauma. Risk factors for atraumatic AVN include alcoholism, steroid use, chronic renal disorders, sickle cell and other hemoglobinopathies, Cushing disease, Gaucher disease, and HIV.
Groin pain may occur with groin strains, lumbar radiculopathies (third lumbar [L3] nerve), or occult hernias. Patients with pulled groin muscles have pain and soreness over the adductor muscles and inguinal region. Moreover, groin strains improve with analgesic medication and cold packs. Severe cases may require physical therapy. Lumbar (L3) radiculopathies are associated with pronounced low back pain that is exacerbated by flexion and positive straight leg raising signs. Moreover, sensory impairment to the upper one-third of the thigh (L3 sensory dermatome) may occur.
Radiographic Evaluation
Plain radiographs of the hip should be ordered, both anteroposterior (AP) and lateral (frog leg) views. If these are normal, magnetic resonance imaging (MRI) may also be performed (Fig. 12.1). Bone scans are highly sensitive but very nonspecific. An MRI scan produces superior anatomic delineation.
AVN may be classified into four different stages:
Stage 1: Standard radiographs are normal, but early AVN is detectable on MRI.
Stage 2: The femoral head develops cystic and sclerotic changes, which are apparent on standard radiographs. However, the shape of the femoral head remains intact.
Stage 3: The crescent sign is identified as a sclerotic rim along the femoral head. A subchondral radiolucent line runs beneath the rim of the femoral head, which is caused by osteonecrosis and bony reabsorption near the articular surface. The crescent sign is identified with cystic and sclerotic changes in the femoral head. It represents advanced AVN.
Stage 4: There is a collapse with flattening of the femoral head associated with marked sclerosis. As the condition progresses, the sclerosis is caused by necrotic bone that appears more dense, and the necrotic bone diminishes in size and becomes even more sclerotic. Ultimately, the diseased subchondral bone collapses, leading to deformation of the femoral head, and subsequently joint space narrowing and acetabular damage (Fig. 12.2).
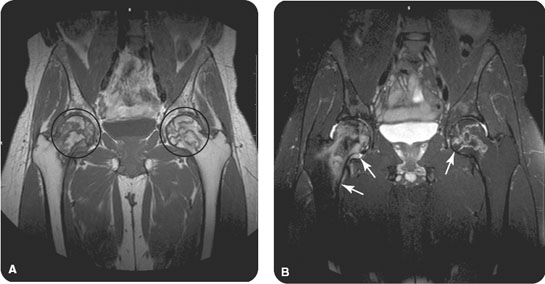
FIGURE 12.1 Magnetic resonance imaging of the bilateral hips demonstrates abnormal serpiginous signal in the bilateral femoral heads and necks on (A) T1-weighted and (B) T2-weighted images, consistent with avascular necrosis and bilateral bone infarcts. In addition, there is increased T2-signal in the right femoral head and neck, consistent with bone marrow edema. Compare with the normal T1 and T2 signals in the femoral diaphysis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








