Fig. 7.1
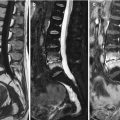
Transient osteoporosis of the hip, MR imaging.
Coronal T1-weighted image (a) of a 48-year-old man who presented with acute left hip pain shows hypointense bone marrow edema in the head, neck, and intertrochanteric zone of the left femur (arrow). On the corresponding fat-suppressed T2-weighted image (b), there is marked increase in the signal intensity of the abnormal marrow (large arrow). On the fat-suppressed post-contrast T1-weighted image (c), edematous marrow enhances intensely (arrow). Note the presence of a small joint effusion (small arrows on b)
Absence of hypointense areas in the subchondral bone marrow on MR images of the hip ensures reversibility of imaging findings and complete resolution of clinical symptoms. Occasionally though, thin hypointense subchondral lesions may be observed in patients with TOH due to subarticular insufficiency microfractures related to the demineralization [20]. When the thickness of these areas is equal to or exceeds 4 mm, there is a strong possibility for lesion irreversibility [3]. It must be stressed that the diagnosis of TOH is established with certainty only after demonstration of complete resolution of imaging findings and/or clinical symptoms (Fig. 7.2).
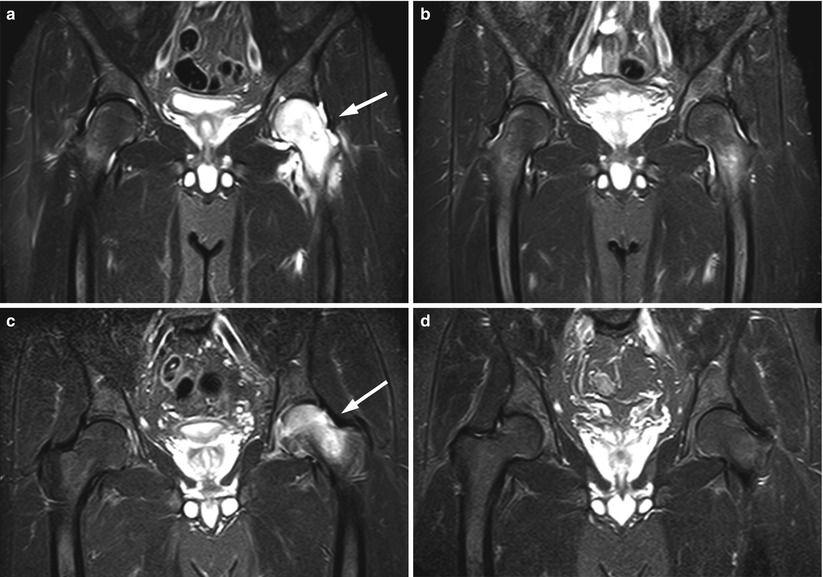
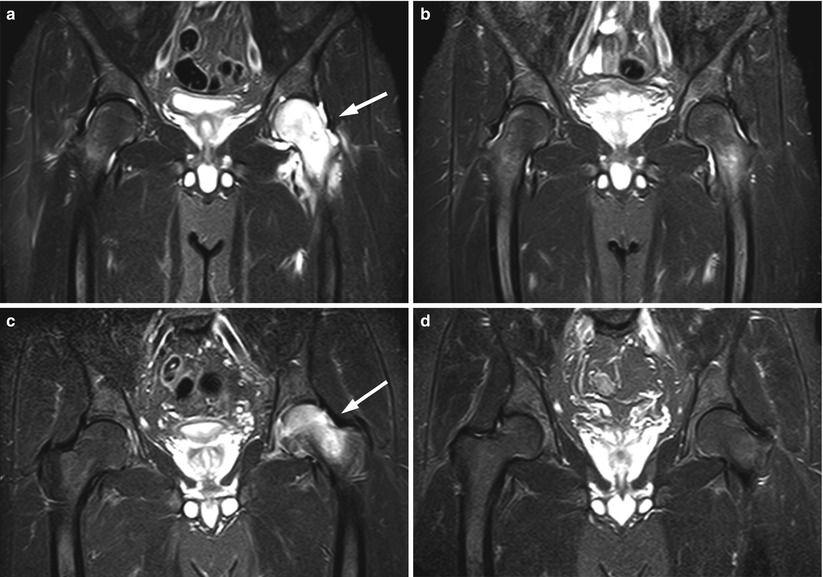
Fig. 7.2
Transient osteoporosis of the hip, MRI follow-up.
Coronal STIR image (a) of the hip of a 32-year-old man with acute left hip pain shows pronounced hyperintense marrow edema involving the head and neck of the left femur (arrow). A left joint effusion is also present. Follow-up STIR image (b) obtained 3 months later shows almost complete resolution of abnormal signal with minimal residual hyperintensity at the intertrochanteric region. At the time of the second MRI, the patient’s symptoms had markedly improved. Coronal STIR image (c) of a 44-year-old man with acute left hip pain shows hyperintense bone marrow edema in the head and neck of the left femur (arrow). Follow-up STIR image (d) obtained 9 months later shows complete resolution of the edema
Osteonecrosis (ON) or avascular necrosis of the femoral head more commonly affects young adults. It is more frequent in men than women with a 7:3 ratio [21]. Osteonecrosis, either idiopathic or secondary to a variety of conditions, is characterized by local ischemia which leads to necrosis of trabecular bone and bone marrow and eventually to collapse of the articular surface. The femoral head is more prone to osteonecrosis compared to other osseous sites, because of its relatively poor vascular supply. At presentation, symptoms of ON of the femoral head may be insidious with vague pain at the hip, thigh, and gluteal region.
Osteonecrosis of the femoral head does not present with a pure bone marrow edema pattern. Bone marrow edema is a late feature of this disorder, associated with worsening of pain and a more dismal prognosis [22]. According to one study of 200 patients with early findings of ON of the femoral head, bone marrow edema never occurred before the appearance of the characteristic band-like sign which consists of a band of abnormal signal intensity at the interface of necrotic and normal marrow [23]. On non-fat-suppressed T2-weighted spin-echo images, the abnormal interface is seen as two rims, a low-signal-intensity outer rim and a high-intensity inner rim (double line sign) [24]. On STIR or fat-suppressed FSE T2-weighted images and on contrast-enhanced fat-suppressed T1-weighted images, it is seen as a single high-intensity rim (bright band sign). A subchondral fracture with high T2 signal (corresponding to the radiolucent crescent sign seen on plain radiographs) is also, when present, strongly indicative of ON.
Transient osteoporosis of the knee (transient BME of the knee) is a distinct clinical entity. It presents with acute onset of pain without prior trauma and manifests with a bone marrow edema pattern on MR images, which by definition resolves completely at follow-up. According to a large study comparing MRI findings at presentation with final outcome, features which favor the diagnosis of transient osteoporosis of the knee over osteonecrosis include extension of edema to the non-weight-bearing surface of the bone and sparing of the subchondral marrow (found, respectively, in 44.9 % and 37.7 % of patients with a final diagnosis of transient osteoporosis of the knee) (Fig. 7.3) [25]. In the same study, almost half of patients with BME of the knee associated with a T2 hyperintense subchondral fracture were finally diagnosed with transient osteoporosis; therefore, according to this study, in the knee (unlike the hip), the presence of a subchondral fracture does not exclude the diagnosis of transient osteoporosis.
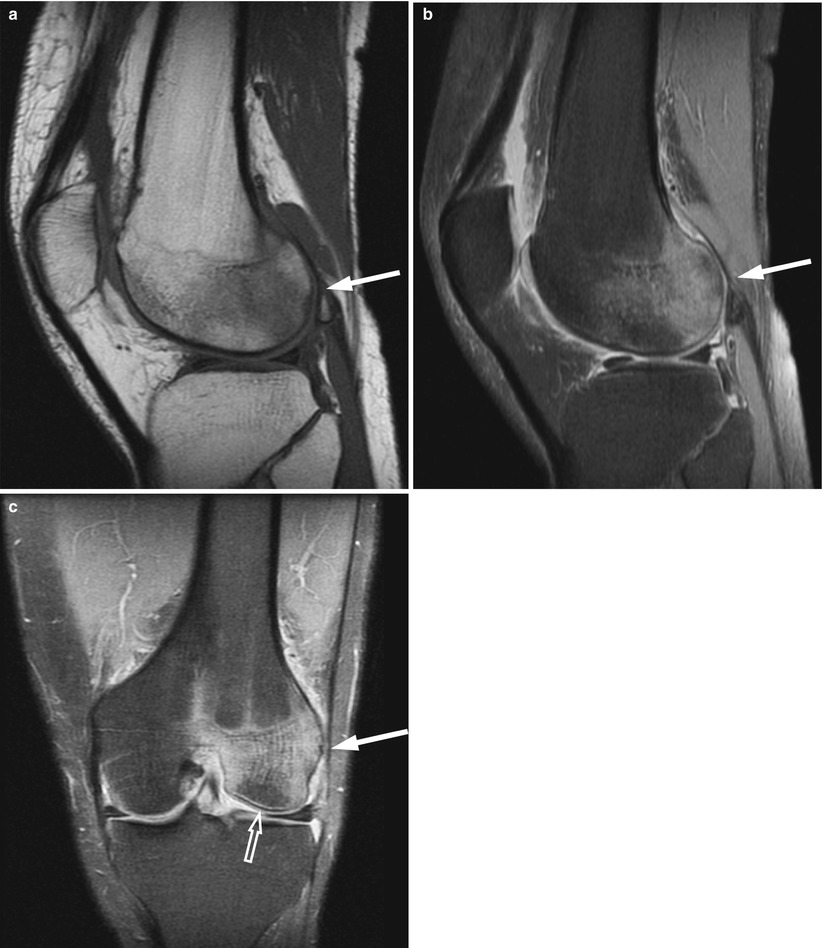
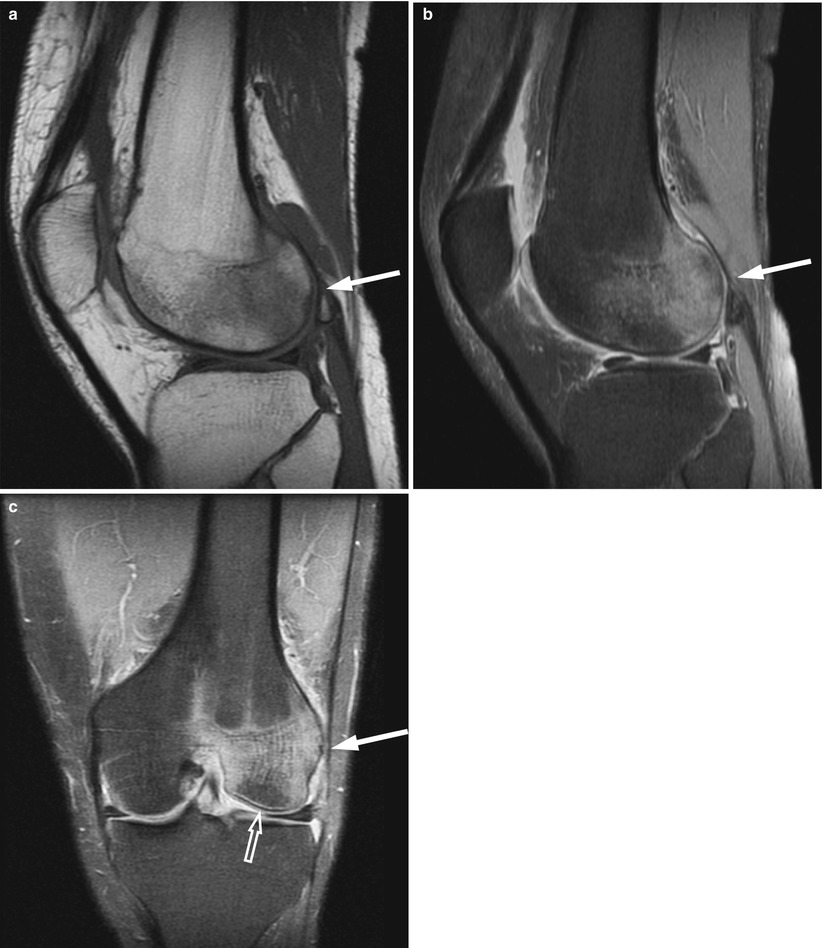
Fig. 7.3
Transient osteoporosis of the knee, MR imaging.
Sagittal T1-weighted image (a) of a 50-year-old man with acute knee pain shows low-intensity marrow abnormality involving the non-weight-bearing area of the lateral femoral condyle (arrow). On the sagittal (b) and coronal (c) fat-suppressed proton density images, the signal intensity of the abnormal marrow is markedly increased (arrow). Note sparing of the subchondral region (open arrow in c) which, when present, is characteristic of transient osteoporosis
Spontaneous osteonecrosis of the knee (SONK), first described by Ahlback in 1968, may present with acute bone marrow edema [26]. It mostly affects elderly women, has no known cause, and is not associated with any of the known risk factors for osteonecrosis. Development of microfractures in osteoporotic bone which then lead to osteonecrosis is the most popular theory for the development of SONK [25, 27]. Patients with SONK present with symptoms similar to those of osteoarthritis or meniscal injury. Indeed, osteonecrosis of the knee is present in 10 % of patients with osteoarthritis [28]. On MR images, SONK presents with diffuse bone marrow edema. It affects mostly the weight-bearing surface of the medial femoral condyle (in contrast to transient osteoporosis which often involves the non-weight-bearing parts of the knee). Articular collapse at presentation or during the evolution of the disorder is characteristic of SONK and excludes the diagnosis of transient BME [24]. Furthermore, generalized osteopenia is present in patients with SONK, but it is unusual in a patient with transient BME.
Treatment of transient osteoporosis of the hip includes analgesic drugs and restricted weight bearing. Bisphosphonates are routinely used as they may reduce pain and duration of symptoms [29]. The use of core decompression to expedite recovery and for patients with debilitating pain is controversial considering the self-limiting nature of this disorder [30]. In pregnant women with transient osteoporosis, restriction of weight bearing until reconstitution of normal bone density is strictly recommended to avoid fractures of the hip, which have, occasionally, been reported [31].
7.3 Regional Migratory Osteoporosis
Regional migratory osteoporosis (RMO), first described by Duncan in 1969, manifests with arthralgia migrating to a neighboring joint or, more rarely, to another site within the same joint. It affects almost exclusively the lower extremities [32]. Although rare, RMO is more common than reported in the literature. Many patients, initially diagnosed with transient osteoporosis, suffer recurrence of the disorder in the same or other joints and therefore actually represent cases of RMO. In fact, 5–41 % of patients with transient osteoporosis initially involving the hip joint will develop RMO [33].
RMO mostly affects middle-aged men. There are no known predisposing factors for this disorder, although an increased incidence of smoking or low dietary calcium intake among patients with RMO has been observed [34]. Increased serum alkaline phosphatase and hypophosphatemia have occasionally been reported in patients with RMO [8]. The disorder typically proceeds from proximal to distal joints [35]. Rarely migration of bone marrow edema occurs within the same joint, from one femoral condyle to the other in the knee or to adjacent bones of the foot and ankle (Fig. 7.4). Time intervals between episodes of arthralgia range from 2 to 12 months, with a second episode occurring even before complete resolution of pain.
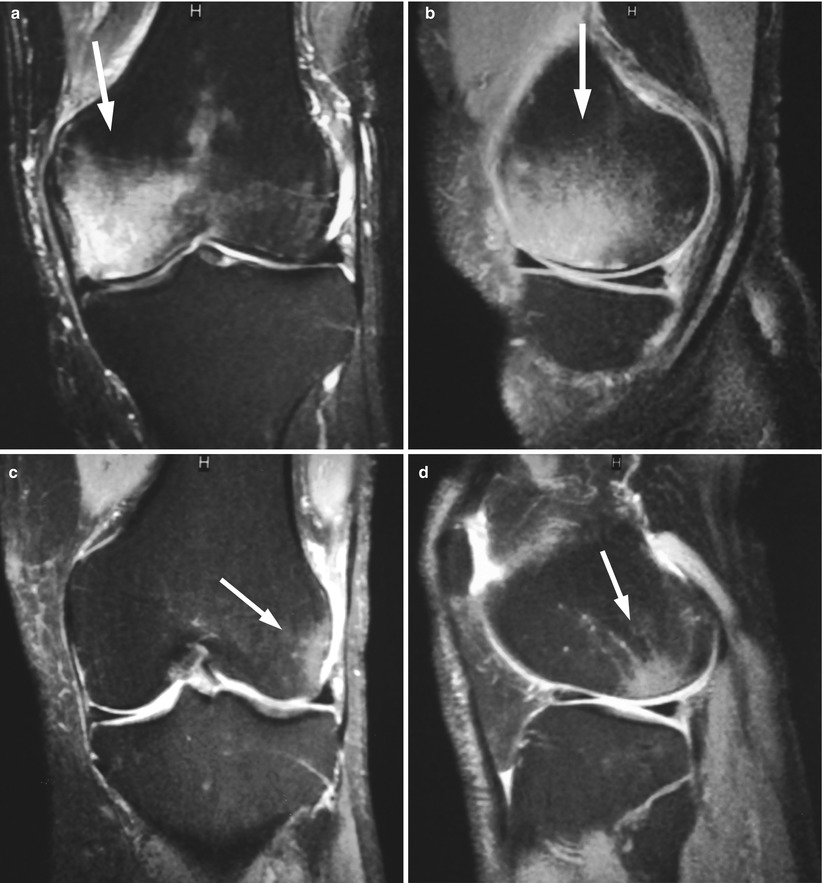
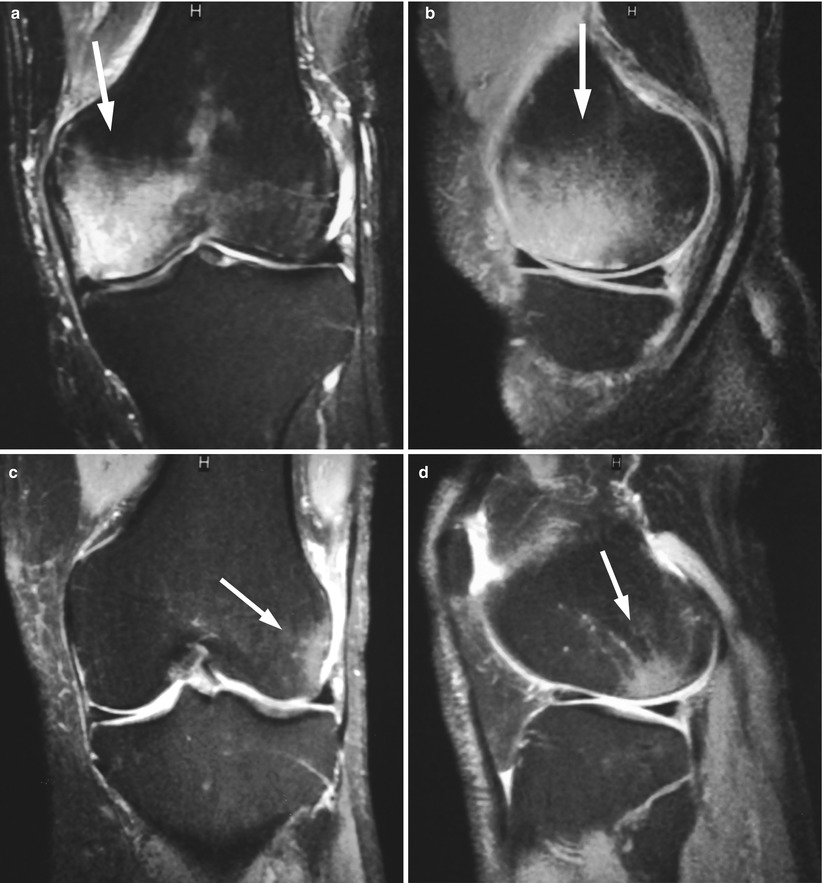
Fig. 7.4
Regional migratory osteoporosis, MR images.
Coronal (a) and sagittal (b) fat-suppressed proton density images of the knee of a 52-year-old man with acute knee pain show hyperintense bone marrow edema involving the medial femoral condyle (arrow). On follow-up MRI 3 months later (not shown), there was complete resolution of the edema. Nine months after the initial MRI, the patient presented with new-onset pain of the same knee. Coronal (c) and sagittal (d) fat-suppressed proton density images of the knee show intra-articular migration of the bone marrow edema to the lateral femoral condyle (arrow)
The imaging findings of RMO are similar to those of TO; it is the migratory feature which establishes the diagnosis of RMO. Because of their similar behavior and imaging manifestations, both RMO and transient osteoporosis of the hip are believed to belong to the same spectrum of disease. It has been suggested that systemic osteoporosis may play a causative role in RMO, and, therefore, bone densitometry is recommended in these patients [33, 36].
Key Points
Regional migratory osteoporosis
Typical transient BME pattern
Affects almost exclusively the lower extremities
Migration occurs to a neighboring joint or within the same joint
May be associated with systemic osteoporosis
7.4 Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS), also known as reflex sympathetic dystrophy, algoneurodystrophy, or Sudeck’s atrophy, has been grouped together with transient osteoporosis and regional migratory osteoporosis since all three entities manifest with arthralgia and osteopenia/osteoporosis. Due to difficulties in diagnosing this disorder, the incidence of CRPS is hard to determine. In a large population-based study, the overall incidence rate of CRPS was 26.2 per 100,000 person/years with a female to male ratio of 3.4:1 [37].
CRPS occurs after trauma or surgery and rarely, it may be idiopathic. It is divided to CRPS-1 where no neural damage is evident and CRPS-2 where pain is related to an identifiable nerve injury. This syndrome involves the small bones and soft tissues of the hands and, less frequently, the feet. The early (inflammatory, 1–7 weeks) phase of CRPS is characterized by burning pain which usually affects the entire limb, trophic changes of the skin (redness, swelling, thickening, warmth, hair growth), as well as sensory-motor and autonomic disturbances; symptoms are disproportionate to the triggering event, and they have been attributed to dysregulation of the central and autonomic nervous system [38]. In the second (dystrophic, 2–24 months) phase of the disorder, pain diminishes, skin temperature drops, and there is loss of hair and perhaps tremor of the affected limb. In the chronic (atrophic) phase, the skin may become cyanotic and cold with muscle atrophy.
Typical radiographic changes of CRPS consist of patchy, initially periarticular, osteoporosis of the affected extremity together with subperiosteal bone resorption. Changes on radiographs appear about 2 weeks after onset of pain. Three‐phase bone scintigraphy is highly sensitive for the diagnosis of CRPS. Different scintigraphic diagnostic criteria, both qualitative and quantitative, have been described. The most suggestive pattern of CRPS consists of increased flow on the angiographic phase, increased blood pool activity, and diffusely increased periarticular uptake on delayed images. Many authors have found that the diffuse increased activity in the delayed images is the most sensitive scintigraphic finding in CRPS [39, 40].
At the early phase of CRPS, MRI shows increased T2 signal and contrast enhancement of the periarticular soft tissues. Small joint effusions may be present. MRI findings of muscle atrophy indicate irreversibility of the disease. Results on the presence of bone marrow edema on MRI studies of patients with CRPS are conflicting. In one study of patients with CRPS of the foot, bone marrow edema was described in almost half of patients during the early inflammatory phase of the disease, but in none during the later, dystrophic phase (Fig. 7.5) [41]. Other investigators, however, reported only soft-tissue changes on MR images of patients with CRPS [38, 42]. Results of a recent meta-analysis study support the use of three-phase bone scan to rule out CRPS because of its high negative predictive value and greater sensitivity compared to both MRI and bone radiographs [43].
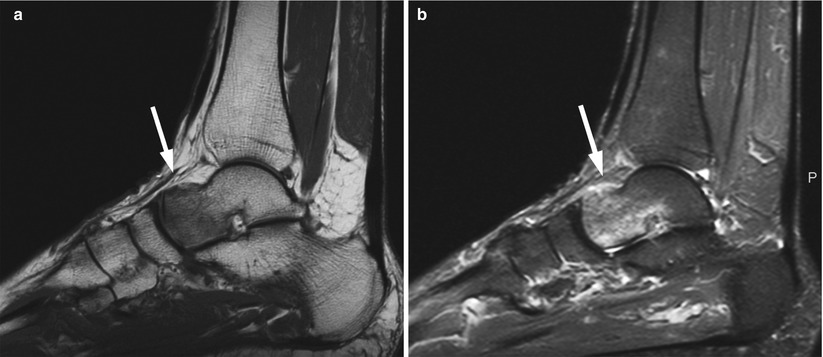
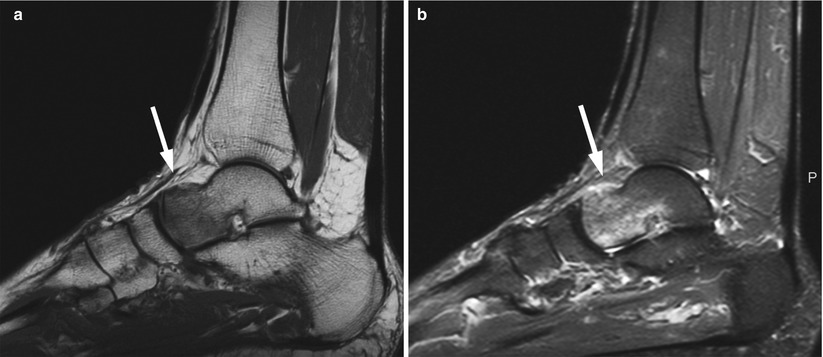
Fig. 7.5
Complex regional pain syndrome of the ankle, MR images.
Sagittal T1-weighted (a) image of the ankle of a 45-year-old man with intense burning ankle pain and a history of blunt trauma to the foot shows heterogeneous hypointense bone marrow edema at the anterior aspect of the talus (arrow). Sagittal fat-suppressed proton density image (b) shows hyperintense signal of the affected marrow with minimal adjacent soft-tissue edema (arrow)
Key Points
Complex regional pain syndrome
Affects the hands and less frequently the feet
Manifests with excruciating pain and skin changes
Plain radiographs show periarticular osteoporosis
A triple phase bone scan has a high negative predictive value for CRPS
MRI shows soft-tissue changes and less often bone marrow edema
7.5 Calcineurin Inhibitor Pain Syndrome
Calcineurin inhibitor pain syndrome (CIPS), also known as posttransplant distal limb syndrome, is a rare, self-limiting bone marrow edema syndrome of the lower extremities which affects mostly renal but also other organ transplant patients receiving calcineurin inhibitor drugs (tacrolimus and cyclosporine) for immunosuppression. Grotz et al. reported CIPS in nine solid (eight renal, one heart) transplant patients, an incidence of 1 % of their study population [44]. It is now known that this syndrome may occur with solid organ or hematopoietic stem cell transplantation. It has also been reported in a patient with adult-onset Still’s disease who was under treatment with calcineurin inhibitor drugs [45].
CIPS affects the joints of the lower extremities, and it is almost always bilateral and symmetric. It manifests with severe pain, 3 weeks to 14 months after the transplant, and symptoms may last for over a year. Pain is preceded by intolerable pruritus without a skin rash. The levels of the immunosuppressive drugs in the serum of patients with CIPS may or may not be elevated; pain, however, subsides within 2 weeks from discontinuation of the calcineurin inhibitors.
The pathogenesis of BME related to calcineurin inhibitors is not known. It is hypothesized that these drugs, through a vasogenic or neurotoxic effect, cause alterations in vascular permeability and perfusion. Bone scintigraphy shows uptake at the affected joints accentuated at the tarsus [46]. MRI shows findings of bone marrow edema which involve the joints of the lower extremities and are strikingly symmetric [47, 48].
Key Points
Calcineurin inhibitor pain syndrome
Affects transplant recipients (mostly renal)
Manifests with severe pain preceded by pruritus without skin changes
MRI shows bilateral, symmetric bone marrow edema in the lower extremity joints, especially of the feet
7.6 Trauma
Bone bruises were first described by Mink in 1987, on MR images of the knee [49]. They are manifestations of occult injury to the bone, resulting from direct or indirect trauma or from altered stress, which cause microfractures of bony trabeculae without disruption of the cortical bone. Limited histopathological studies of posttraumatic bone bruises have shown microfractures of cancellous bone, edema, hemorrhage, and fragments of cartilage and trabecular bone in between intact lamellar bone [50]. Bone bruises are associated with protracted pain [51]. Their incidence in a large study involving 434 patients with acute injury to the knee was 20 %, most of them associated with anterior cruciate ligament injury [52]. In a more recent study of 664 patients with subacute knee complaints, the incidence of bone bruises on MR images was 18.7 % [53]. In the ankle, a 27 % incidence of bone bruises, affecting mostly the medial part of the talus, was reported in 95 patients with inversion injuries [54].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree