(1)
Department of Radiation Oncology, National University Cancer Institute, Singapore (NCIS), National University Health System (NUHS), 1E Kent Ridge Road, NUHS Tower Block Level 7, Singapore, 119228, Singapore
(2)
Shanghai Proton and Heavy Ion Center (SPHIC), 4365 Kangxin Road, Pudong, Shanghai, 201321, China
1 Anatomy and Patterns of Spread
The stomach begins at the gastrooesophageal junction and ends at the pylorus. The greater curvature forms the left and convex border of the stomach, and the lesser curvature forms the right and concave border of the stomach (Fig. 1a). It is divided into four parts: the cardia, fundus, body and antrum. The gastric wall is divided into five layers: mucosa, submucosa, muscularis externa, subserosa and serosa.

Fig. 1
Regions of stomach (a) and relations of the stomach (b)
The stomach is covered with peritoneum and is closely related to the left lobe of the liver, spleen, left adrenal gland, superior portion of the left kidney, pancreas, transverse colon and major blood vessels including the coeliac axis and superior mesenteric artery (Fig. 1b).
Probability of gastric carcinoma varies according to the primary location: ~35 % of tumours arise from the gastroesophageal junction, cardia and fundus. ~25 % of tumours arise from the body. ~40 % of tumours arise from the antrum and distal stomach.
Local extension
The tumour can invade locally with direct involvement of the liver, duodenum, pancreas, transverse colon, omentum and diaphragm.
Proximal tumours may spread upwards to involve the oesophagus.
Perineural invasion can occur.
Regional lymph node metastases (Fig. 2, Table 1)

Fig. 2
Lymph node groups surrounding the stomach
Table 1 Lymph node stations commonly involved in gastric cancer (Japanese Research Society for the Study of Gastric Cancer (JRSGC))
1. Right cardial nodes
9. Nodes along the coeliac axis
2. Left cardial nodes
10. Nodes at the splenic hilus
3. Nodes along the lesser curvature
11. Nodes along the splenic artery
4. Nodes along the greater curvature
12. Nodes in the hepatoduodenal ligament
5. Suprapyloric nodes
13. Nodes at the posterior aspect of the pancreatic head
6. Infrapyloric nodes
14. Nodes at the root of the mesenterium
7. Nodes along left gastric artery
15. Nodes in the mesocolon of the transverse colon
8. Nodes along the common hepatic artery
16. Para-aortic lymph nodes
Lymph node involvement is seen in up to 80 % of cases at diagnosis.
Lymph node involvement depends on the origin of primary disease.
Proximal/gastrooesophageal junction tumours may spread to lower paraoesophageal lymph nodes.
Tumours of the body can involve all nodal sites.
Tumours of the distal stomach/antrum may involve periduodenal and porta hepatis lymph nodes.
2 Diagnostic Workup Relevant for Target Volume Delineation
Prior to radiotherapy planning, it is imperative to review surgical and pathology reports and discuss with the surgeon to identify the areas considered to be the highest risk for recurrence; the type of operation, i.e. total vs. partial gastrectomy, needs to be noted.
Preoperative CT scans should be reviewed to identify the location of primary tumour and involved regional lymphatics.
Consider preradiation quantitative renal perfusion study to evaluate relative bilateral renal function.
Postoperative diagnostic CT scan with oral and intravenous contrast is required with the identification of the following:
Oesophagus and gastric remnant
Anastomosis (gastrojejunal, oesophagojejunal)
Duodenal stump
Porta hepatis
Splenic hilum
Pancreas
Coeliac artery and superior mesenteric artery
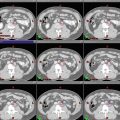
The type of surgery performed depends on the location of tumour, histology pattern (Fig. 3).

Fig. 3
Types of gastric cancer surgery. 3.1 (a) Subtotal gastrectomy, (b) Bilroth II anastomosis. 3.2 (a) Total gastrectomy, (b) Roux-en-Y esophagojejunostomy
3 General Principles of Planning and Target Delineation for Adjuvant Radiation for Adenocarcinomas of the Gastrooesophageal Junction and the Stomach
Patients should fast for 2–3 h before CT simulation and before treatments to ensure an empty stomach and enhance daily treatment reproducibility.
Radiotherapy planning CT scans of 3–5 mm thickness should be obtained with the patient in the supine position with arms overhead, from top of the diaphragm (for stomach) or carina (for tumour of GE junction or cardia) to the bottom of L4.
Immobilisation with a Vac-Lok is recommended for treatment with IMRT.
Intravenous contrast is preferred to demonstrate blood vessels and guide clinical target volume (CTV) delineation, particularly for lymph nodes; preoperative CT scans should be used to aid identification of preoperative tumour volume and nodal groups to be treated.
CTV for adjuvant radiation therapy for gastric cancer depends on the position of the primary disease as well as the status of lymph node metastasis. Suggested target volumes for CTV coverage depending on subsite are detailed in Tables 2, 3, 4, 5 and 6.
Table 2
Target volume definition and description
Target volumes
Definition and description
GTV
Gross residual disease defined by CT imaging and surgical findings
PTV (residual disease)
GTV/positive margins + 1.5 cm. Cone down boost after 45 Gy to a total dose of 50.4 to 54Gy in 1.8Gy/fraction
CTV45
Coverage of nodal groups according to subsite (see Table xx). Also includes remnant stomach, anastomosis (gastrojejunal, oesophagojejunal), duodenal stump
PTV45
CTV45 + 1 cm margin. A larger margin may be required for organ motion and setup uncertainties
Table 3
General considerations for clinical target volume
Target volumes
Definition and description
Duodenal stump
Should preferably be covered in patients who have had a partial gastrectomy for distal/antral tumours
Should not be covered in patients with proximal/cardia tumours who have had a total gastrectomy
Anastomosis
Gastrojejunal anastomosis (partial gastrectomy for tumours of the distal stomach)
Oesophagojejunal anastomosis (total gastrectomy for tumours of proximal stomach or GE junction) should be treated
Para-aortic nodes
Should be included for the entire length of the CTV
Paraoesophageal nodes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access