, Gaorav P. Gupta1, Nadeem Riaz1, Sean McBride1 and Nancy Y. Lee1
(1)
Department of Radiation Oncology, Memorial Sloan Kettering Cancer Center, New York, NY, USA
1 Anatomy and Patterns of Spread
The hypopharynx extends from the level of the hyoid bone to the inferiormost level of the cricoid cartilage. Anteriorly, the border is formed by the connection of the two pyriform sinuses at the postcricoid region and with the posterior extent defined by the posterior pharyngeal wall.
The three subdivisions and their distribution of tumor involvement according to the SEER database, from 2000 to 2008, are the pyriform sinuses (83 %), posterior pharyngeal wall (9 %), and postcricoid region (4 %).
Pyriform sinus
“Pear-shaped” structure that begins superiorly at the glossoepiglottic fold with its apex extending inferiorly to the level of the cricopharyngeus. It is laterally bound by the thyroid cartilage and medially defined by the cricoid cartilages, arytenoids, and the lateral surface of the aryepiglottic fold.
Superiorly, cancers can invade the arytenoids and aryepiglottic folds as well as the paraglottic and preepiglottic space.
Involvement of thyrohyoid membrane, which surrounds the pyriform sinuses superiorly and where internal branch of superior laryngeal nerve passes through cause referred otalgia.
Laterally, tumors can invade into the segments of the thyroid cartilage and then further into the lateral neck compartments.
Medially, intrinsic laryngeal muscles can be involved causing vocal cord fixation.
Inferiorly, extension past the apex can involve the thyroid gland.
Posterior pharyngeal wall
Formed by the constrictor muscles and directly contacts the paravertebral fascia. Extends from hyoid bone to the inferior aspect of the cricoid.
Tumors can extend to involve the oropharynx superiorly, the prevertebral fascia and retropharyngeal space posteriorly, and the cervical esophagus inferiorly.
Postcricoid region
Extends from the posterior surface of the aryepiglottic fold and arytenoids to the cricoid cartilage.
Anteriorly, tumors can invade the larynx causing vocal cord fixation.
Radially, the cricoid cartilage can be involved.
Other areas at risk from advanced local extension are the esophagus, trachea, and pyriform sinuses.
Dosimetric coverage of the primary site can be a challenge because hypopharyngeal cancers have a propensity for submucosal spread. Approximately 60 % microscopic spread of about 10 mm (superiorly), 20 mm (laterally and inferiorly), and 25 mm (medially) (Ho et al. 1993).
The rich lymphatic network of the hypopharynx drains primarily into the jugulodigastric lymph nodes and middle jugular chains (see Fig. 1).

Fig. 1
Distribution of nodal metastases by neck level based on radical neck dissections in 104 patients (Candela et al. 1990)
Pyriform sinuses drain primarily to the upper and middle jugular nodes, posterior cervical nodes, and retropharyngeal lymph nodes.
Posterior pharyngeal wall empties into the jugular nodes and retropharyngeal nodes (Allen et al. 2007).
Postcricoid region drains to the middle and lower jugular nodes and to the paratracheal nodes.
2 Diagnostic Workup Relevant for Target Volume Delineation
Clinical examination with a thorough laryngoscopic evaluation is critical in defining the mucosal extent of hypopharyngeal cancers, particularly for those arising in the pyriform sinus.
MRI may better delineate primary tumor borders, inform regarding potential cartilage or esophageal invasion, and may also facilitate identification of abnormally enhancing lymph nodes (Castelijns et al. 1988; Roychowdhury et al. 2000; Rumboldt et al. 2006; Wenig et al. 1995).
The sensitivity and specificity of PET are superior to CT alone (Di Martino et al. 2000). FDG-PET provides metabolic information and may identify hypermetabolic cancer cells within morphologically normal-appearing lymph nodes (Adams et al. 1998; Schwartz et al. 2005), which should be included within the high-dose PTV.
3 Simulation and Daily Localization
CT simulation using 3-mm slice thickness with IV contrast is used (unless medically contraindicated) to delineate the primary tumor, gross lymphadenopathy, and additional regions at risk. The simulation scan should extend from the top of the skull to the carina with the isocenter generally placed immediately above the arytenoids.
The patient should be immobilized with a 5-point thermoplastic head and neck mask or with a 3-point thermoplastic head and neck mask and a shoulder pull board. The neck should be maximally hyperextended to pull as much of the oral cavity and mandible out of the field as possible, and the shoulders should be pulled inferiorly to minimize the risk of beam interference.
4 Target Volume Delineation and Treatment Planning
Due to concerns regarding treatment-related late toxicities, hypofractionation and/or simultaneous integrated boost with IMRT is not recommended for this disease site.
We utilize dose-painting IMRT (Lee et al. 2007) and prescribe to 70 Gy in 2 Gy fractions to sites of gross disease, 59.5 Gy in 1.7 Gy fractions to high-risk subclinical regions, and 56 Gy in 1.6 Gy fractions to lower-risk subclinical regions. Additional fractionation regimens as well as cone-down IMRT approaches are also appropriate.
We routinely use all-in-one IMRT for hypopharynx cancers, as a match line to a low anterior neck field would frequently fall in the region of the primary tumor or involved lymph nodes.
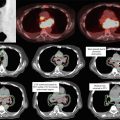
Suggested treatment target volumes for gross disease (Table 1), high-risk subclinical (Table 2), and lower-risk subclinical regions (Table 3) are described in the following tables. The principles of target delineation are similar for early and advanced stages (Figs. 2 vs 3, 4, and 5). Shown here are examples of each subsite: pyriform sinus (Figs. 2 and 3), posterior pharyngeal wall (Fig. 4), and postcricoid region (Fig. 5).
Table 1
Suggested target volumes at the gross disease region
Target volumes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access