Fig. 1
Arterial supply and venous drainage of the thyroid gland. The superior and inferior thyroid arteries (STA and ITA) arise from the external carotid arteries and the thyrocervical trunks, respectively. Rarely, the thyroid ima artery, a branch of the brachiocephalic artery, may enter the inferior margin of the thyroid isthmus. The STA is usually the first branch of the external carotid artery, and it has an intimate relationship with the superior laryngeal nerve, making this nerve and its motor branch, the external laryngeal nerve, susceptible to injury during thyroidectomy or from direct compression in patients with locally advanced thyroid cancers. The venous drainage of the thyroid gland is variable as in other organs. Generally, the superior and middle thyroid veins drain into the internal jugular vein, and the inferior thyroid veins drain into the brachiocephalic vein (From Springer reference https://www.springerimages.com/Images/MedicineAndPublicHealth/2-ACE0101-14-001A)

Fig. 2
Thyroid gland and its relations at the level of the thyroid cartilage. Color enhancement demonstrates major arteries (red), veins (blue), and nerves (yellow). The thyroid gland is enhanced with pink. It is important to note the close relationship of the superior pole of the thyroid gland, with the carotid sheath and sympathetic chain (From Springer reference: Oertli and Udelsman 2012. http://link.springer.com/chapter/10.1007%2F978-3-642-23459-0_2/fulltext.html)
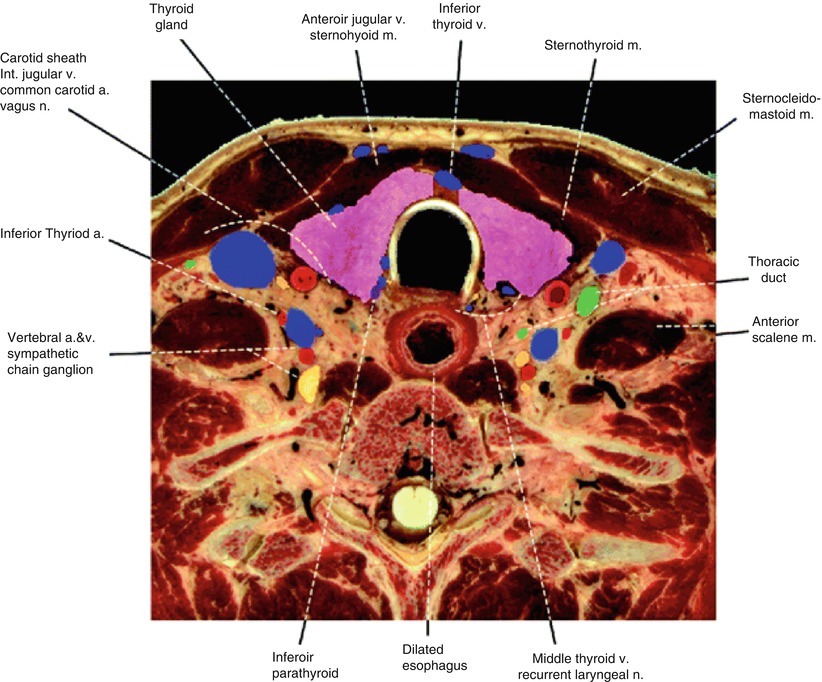
Fig. 3
Thyroid gland and its relations at the level of the third tracheal ring. Note the posteromedial relationships of the thyroid gland with the recurrent laryngeal nerve and the middle thyroid veins. The thoracic duct (green) is atypically dilated close to where it joins the left internal jugular and subclavian veins. The inferior thyroid artery follows a looping course. An inferior right parathyroid gland (purple) is evident near the recurrent laryngeal nerve and middle thyroid veins. Major nerves (yellow), arteries (red), veins (blue), and thyroid (pink) are indicated (From Springer reference: Oertli and Udelsman 2012. http://link.springer.com/chapter/10.1007%2F978-3-642-23459-0_2/fulltext.html)
2 Diagnostic Workup Relevant for Target Volume Delineation
In addition to a focused head and neck examination, radiographic imaging should be obtained for diagnosis, staging, and treatment planning.
All patients should undergo a CT of the neck, preferably with contrast, though this will ultimately delay radioactive iodine therapy if applicable. It is important to include the superior mediastinum in the scan to assess for the presence of superior mediastinal lymphadenopathy.
If there is concern for cervical esophagus involvement, a MR neck with gadolinium may aid in the diagnosis.
Laboratory workup should include complete blood count (CBC), comprehensive metabolic panel (CMP), thyroid-stimulating hormone (TSH), T3, free T4, and thyroglobulin level.
As the definitive treatment for non-anaplastic thyroid carcinomas is surgical resection, all patients should be evaluated by an experienced head and neck surgeon to assess resectability.
3 General Treatment Considerations
Thyroid malignancies constitute the widest range of clinically aggressive tumors. Patients with well-differentiated carcinoma carry an extremely favorable prognosis, whereas anaplastic thyroid carcinoma is among the deadliest of all human cancers.
The role of external beam radiation therapy (EBRT) in the treatment of differentiated thyroid cancer remains controversial but is better established for medullary carcinoma and anaplastic carcinoma.
There is a lack of prospective trials evaluating the efficacy of EBRT in patients with well-differentiated thyroid carcinoma.
Multiple single-institution experiences have demonstrated that EBRT improves locoregional control in patients with microscopic/gross residual disease after surgical resection and those with unresectable disease.
Postoperative radiation therapy for patients with extrathyroid extension or even extranodal extension with well-differentiated histology remains controversial, as alternative adjuvant therapies, such as radioactive iodine (RAI), are often preferred.
Postoperative radiation therapy should be considered for any patient with well-differentiated RAI-refractory disease or medullary carcinoma with concern for microscopic or gross residual disease.
Patients with anaplastic carcinoma require immediate referral to a tertiary cancer center and mandate multidisciplinary care given their poor prognosis.
Intensity-modulated radiation therapy (IMRT) is the recommended technique for definitive or postoperative radiation therapy for thyroid cancer to decrease treatment-related morbidity (Schwartz et al. 2009).
4 Principles of Simulation and Target Delineation
Given the accuracy of IMRT treatment, efficacy is largely dependent on tumor localization.
Imaging may be difficult to interpret as many of these patients have undergone multiple head and neck surgeries.
Fludeoxyglucose positron emission tomography (FDG-PET) can be useful for the delineation of tumor in patients with anaplastic and RAI-refractory-differentiated carcinomas.










