12 The rapid evolution of interventional techniques for the heart, the introduction of new devices, and improvements in adjunctive pharmacotherapy have led to explosive growth in the field of interventional cardiology. Meticulous attention to patient selection, risk stratification, choice of appropriate equipment, and procedural skills is essential for the successful outcome of a percutaneous coronary intervention (PCI). In addition, attention to specific angiographic characteristics is critical for planning of PCIs (Table 12.1). Multislice–multidetector computed tomography (MDCT) can accurately provide anatomic information in a noninvasive manner to improve the planning and outcome of PCI. Estimation of periprocedural risk identifies those patients who are at higher risk for PCI-related complications and allows the implementation of measures aimed at reducing that risk (eg, hemodynamic support, optimizing volume status, surgical standby). Demographic and clinical characteristics (eg, age, gender, diabetes mellitus, renal failure) play an important role in determining risk. MDCT can further refine the risk stratification by providing information on the presence of significant left main disease, multivessel coronary artery disease, and determination of left ventricular (LV) systolic function.1 The purpose of this chapter is to review the role of coronary MDCT imaging in the planning and follow-up of percutaneous and surgical coronary interventions. Patients with severe diffuse peripheral vascular disease, especially those with prior revascularization procedures, require careful assessment of vascular anatomy and access sites. Appropriate selection of percutaneous access is essential in complex interventions requiring the use of large-diameter guiding catheters and high-risk interventions where the use of an intra-aortic balloon pump may be necessary. In such patients, CT angiography (CTA) provides a noninvasive roadmap that can assist the interventionalist in selecting the most appropriate access sites. An appropriate access route should avoid significant obstructive disease in the aortoileofemoral system, as well as excessively tortuous vessels and calcifications that may preclude advancement of interventional equipment. In patients with prior surgical revascularization, such as aortobifemoral bypass surgery, CTA angiography can determine whether the grafts represent appropriate vascular access sites. When upper extremity access (brachial or radial artery) is contemplated, CTA allows evaluation of the aortic arch branches for atherosclerosis and tortuosity. Manipulation of catheters and interventional wires in severely atherosclerotic aortic arch branches may result in cerebral embolization. Calcified coronary artery stenoses pose significant technical challenges to the interventional cardiologist. PCI of calcified lesions is associated with a higher rate of procedural failure and increased risk of periprocedural and long-term major adverse clinical events (eg, death, myocardial infarction, need for repeat target-vessel revascularization).2,3 The presence of coronary calcium makes the stenotic vessel rigid and may affect the ability to deliver interventional devices to the target lesion. Furthermore, calcification of the vessel wall may render the vessel resistant to dilatation by conventional balloon angioplasty (PTCA).4 This occurs more commonly in vessels with circumferential (360-degree) calcification and with intimal–medial (as opposed to adventitial) calcification.3,5,6 In such cases, the use of atheroablative devices such as rotational atherectomy is indicated.4 However, unnecessary atheroablation of long-calcified coronary segments may result in significant embolization of the distal microvasculature, resulting in periprocedural myocar-dial infarction.6 MDCT can accurately identify characteristics of a complex calcified lesion. Specifically, MDCT can demonstrate the presence, location, severity, and length of calcification. In addition, it can display the distribution of calcium in the vessel wall (circumferential versus focal, intimal versus adventitial) (Fig. 12.1). This information is critical in deciding whether to use atheroablative devices and in estimating the risk and likely success of the planned PCI.
Cardiac Interventions
 Multislice–Multidetector CT and Planning of Cardiac Interventions
Multislice–Multidetector CT and Planning of Cardiac Interventions
 Vascular Access
Vascular Access
 Calcified Lesions
Calcified Lesions
Aortic root size |
Selection of guiding catheters |
Vessel characteristics in native coronaries |
Presence of coronary anomalies |
Location of the coronary ostia |
Spatial orientation of the proximal segment of the vessel |
Vessel diameter |
Vessel tortuosity |
Vessel calcification |
Amount of myocardium supplied by vessel |
Vessel characteristics in bypass grafts |
Proximal anastomosis site |
Vessel course (anterior to the aorta versus retroaortic) |
Type of graft (single, sequential, Y-graft) |
Degenerated saphenous vein graft |
Graft size |
Amount of myocardium supplied by grafted vessel |
Lesion characteristics |
Location |
Length |
Vessel diameter |
Bifurcation |
Severity of stenosis |
Calcification (severity, pattern of vessel involvement) |
Vessel angulation at the stenosis |
Plague characterization |
High-risk lesions |
Left main |
Ostial stenosis |
Bifurcation lesions |
Left ventricular systolic function |
Congenital heart disease |
Atrial and ventricular septal defects |
Coronary fistulae |
 Vessel Tortuosity and Angulated Lesions
Vessel Tortuosity and Angulated Lesions
Target-vessel tortuosity is a known complicating angiographic variable for PCI.7 Tortuosity complicates the delivery of interventional devices and can result in incomplete stent apposition in an angulated segment.8 Incomplete stent apposition is associated with increased risk of stent thrombosis and with drug-eluting stents, with incomplete elution of drug to the vessel wall, and a potentially increased rate of restenosis.9
Adequate PCI outcomes in tortuous vessels frequently require the use of more “aggressive” devices, such as larger-caliber guides and stiffer guidewires. The use of such devices may result in vascular injury, such as dissection, acute closure, or perforation.10 MDCT can accurately define the severity of tortuosity, demonstrate the presence of angulation at the target lesion, and guide the interventional cardiologist in the choice of appropriate equipment (Fig. 12.2).
 Chronic Total Occlusions
Chronic Total Occlusions
PCI of chronic total occlusions (CTO) is associated with lower success (recanalization) rates, mainly related to the difficulty of crossing the occlusion with a guidewire.11 PCI of a CTO may be a relatively lengthy procedure, resulting in increased radiation exposure and use of contrast. Several angiographic characteristics may be identified by MDCT to assist in predicting the recanalization success rate. Chronic total occlusions with a tapered vessel stump, the absence of side branches at the site of the occlusion, and the lack of significant bridging collateral circulation are favorable angiographic predictors.12 MDCT may also serve as a roadmap for recanalization of occluded vessels, as it provides information on vessel tortuosity, length of occlusion, and the presence and pattern of calcification (Fig. 12.3). Yokayama et al reviewed the utility of MDCT imaging for lesion and plaque characterization before attempting PCI of a CTO in 22 patients. They report that the use of MDCT resulted in procedural success in 21 CTOs (91.3%). The ability to identify the various components of the atherosclerotic plaque and obtain three-dimensional renderings of the occluded segment plays a significant role in the ability to recanalize the stenosis. They also suggest that presence of calcified plaque in the proximal and distal portions of the CTO may reduce the success rate of the procedure.13
 Bifurcation Lesions
Bifurcation Lesions
The success rate of PCI of bifurcation lesions has improved significantly over the past decade. The development of drug-eluting stents and improved stent designs have led to the development of effective bifurcation stenting techniques.14 The pattern of atheromatous involvement and the morphology of bifurcation lesions can be extremely variable. In bifurcation lesions with a small side branch or without significant ostial disease, initial stenting of the main branch with provisional stenting of the side branch may represent a reasonable approach. For lesions with extensive plaque burden involving both the parent vessel and a larger side branch, stenting of both branches will decrease the possibility of plaque shifting with potential side branch loss or suboptimal angiographic result.
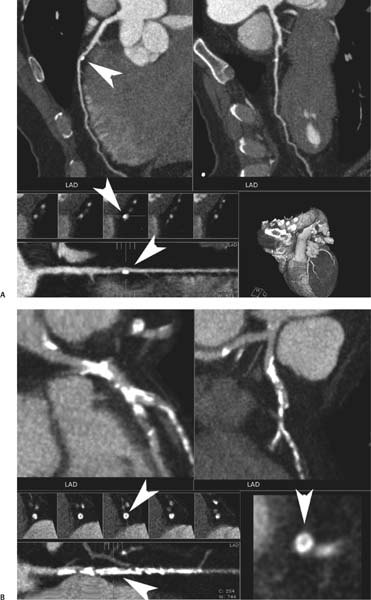
Fig. 12.1 Coronary calcification. (A) Curved maximum intensity projection (MIP) images demonstrate focal calcification of the left anterior descending artery (LAD) with positive remodeling. The calcium involves the adventitia of the vessel (arrowhead) without involvement of the intima. (B) Curved MIP images in a different patient demonstrate diffuse calcification of the left anterior descending artery. Straightened lumen and orthogonal views confirm luminal narrowing with involvement of all layers of the vessel wall (arrowhead).
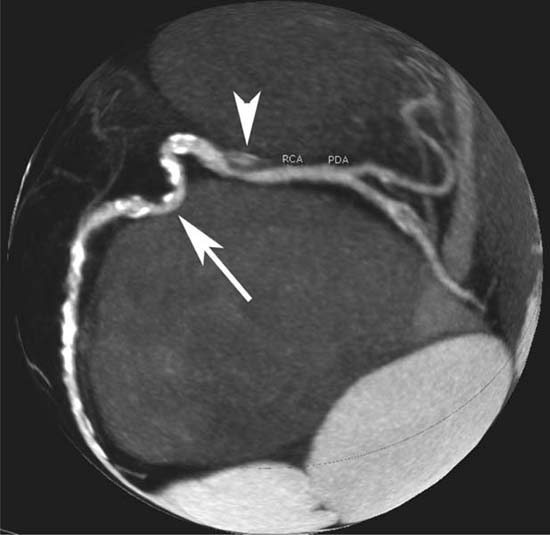
Fig. 12.2 Globe maximum intensity projection of the right coronary artery (RCA). There is eccentric stenosis of the distal RCA with associated ulceration (arrowhead). A segment with severe tortuosity and calcification is identified just proximal to the eccentric stenosis (arrow).
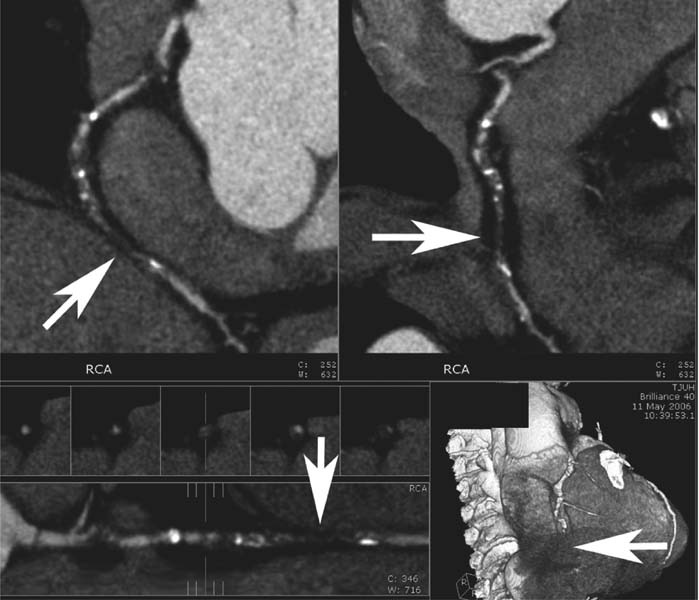
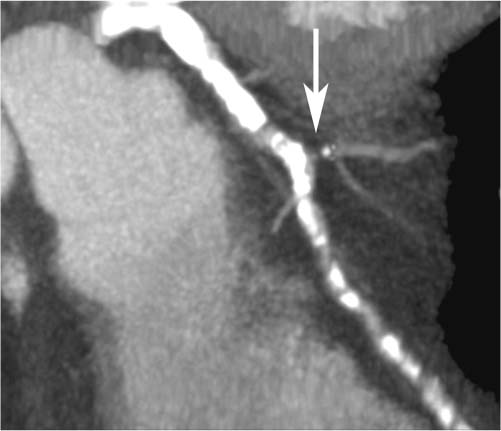
Fig. 12.3 Orthogonal curved maximum intensity projection images demonstrate chronic total occlusion of the mid right coronary artery (RCA) (arrow), with moderate proximal calcification and tortuosity.
For bifurcation lesions, the interventional cardiologist will decide which bifurcation stenting technique is most appropriate based on the diameter of the parent vessel and side branch and the angle between the two vessels. If the diameters of the two vessels are similar and the angle is acute, “culotte” stenting will provide good coverage of the bifurcation without overexpansion of the side-branch stent in the parent vessel. If the side-branch stent is smaller than the main vessel and the angle is acute, “crush” stenting will allow adequate coverage of the lesion without overexpansion of the sidebranch stent. The “kissing” stent technique is ideal for lesions with mild angulation in which the bulk of the plaque involves the parent and side-branch vessels just distal to the bifurcation, especially if the parent vessel proximal to the bifurcation is larger. In situations where continuous control of both branches of the bifurcation is required, such as left main PCI, the crush stent and kissing stent techniques allow bifurcation stenting without leaving one of the two branches temporarily unprotected. If the angle between the parent vessel and the side branch is obtuse or at a right angle, T-stenting will provide adequate coverage of the bifurcation. An important limitation of this technique is the potential for incomplete coverage of the side-branch ostium, which may result in ostial restenosis.15
An important decision faced by the interventional cardiologist when treating bifurcation lesions is to determine whether side-branch protection is necessary. This is an important issue because side branch protection with stenting results in increased PCI complexity, thrombosis, and restenosis. Leaving the side branch unprotected may be a reasonable approach if the vessel is small in diameter and supplies a small amount of myocardium (Fig. 12.4). Side-branch protection is advisable when the side-branch diameter is greater than 2.0 mm, when the side branch originates from a diseased segment of the parent vessel, and when there is greater than 50% ostial stenosis (Fig. 12.5).
Assessment of the presence and severity of calcification in bifurcation lesions is essential because calcified vessels are less compliant. Calcification may interfere with the delivery and deployment of interventional devices (Fig. 12.1). In such cases lesion modification with rotational atherectomy will result in improved lesion compliance. MDCT can provide the interventional cardiologist with all the necessary angio-graphic information (eg, vessel size, angulation, plaque distribution pattern, calcification) to select the appropriate stenting technique and assess the need for debulking.
 Aorto-Ostial Lesions
Aorto-Ostial Lesions
The performance of PCI in aorto-ostial lesions is associated with unique challenges that are not encountered in other coronary segments.16 These lesions are frequently calcified, less compliant, and more difficult to dilate. In addition, because of the ostial location of the stenosis, the ability to engage selectively the vessel in a coaxial manner and maintain a stable guiding catheter position is limited.17 The presence of an anomalous origin of the vessel ostium may further increase the complexity of the PCI and require the use of guiding catheters with a special tip shape. Because of the large amount of myocardium in jeopardy with aortoostial lesions, complications resulting in dissection or acute closure can lead to significant myocardial injury and hemo-dynamic instability.
MDCT allows accurate assessment of aorto-ostial lesion severity, the angle of vessel take-off from the aorta, length of stenosis, anomalous origin of the vessel, presence of calcification, and need for plaque debulking. All these angiographic variables are very important in the selection of guiding catheters of appropriate type and size.
 Left Main Disease
Left Main Disease
With the improvement in interventional equipment, advent of stents, introduction of drug-eluting stents, potent antiplatelet agents, and improved operator technical skills, unprotected left main PCI is being performed with increasing frequency.18 This is a high-risk interventional procedure, the success of which relies on optimal visualization of the vessel and meticulous planning. MDCT can identify all the functional and angiographic characteristics that will allow the interventional cardiologist to assess the level of risk, to determine the feasibility of the procedure, and to select the appropriate equipment. Patients with impaired LV systolic function and severe atherosclerosis of the remaining vessels are at increased risk for periprocedural complications.19 Other important characteristics include vessel size and length, presence and severity of calcification, and the location of stenosis (ostial, mid or, distal) (Fig. 12.6). The complexity and risk of left main PCI are greater for distal left main bifurcation lesions involving the left anterior descending, left circumflex, and ramus intermedius branches.
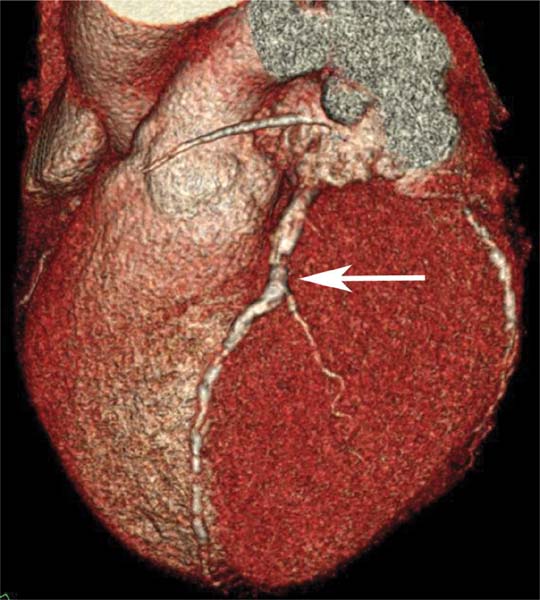
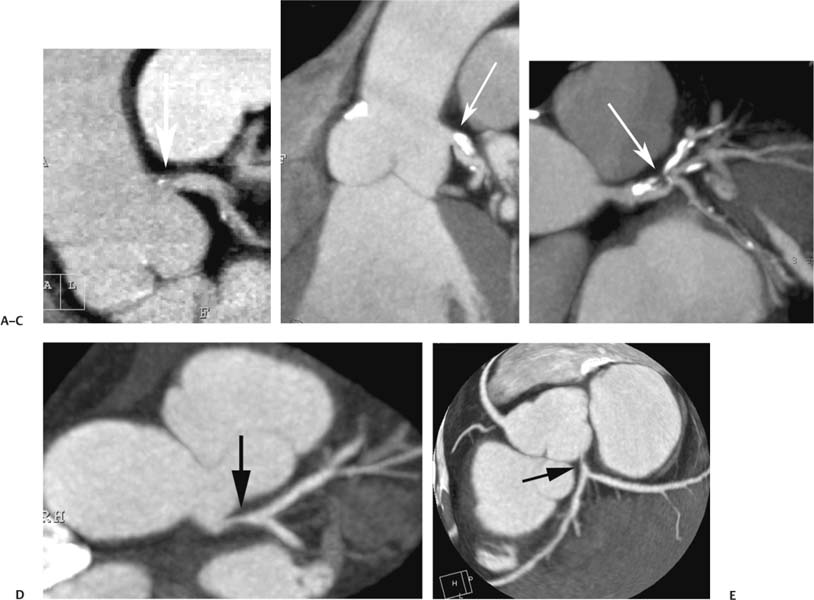
Fig. 12.4 Surface volumetric rendering in the left anterior oblique projection. A bifurcation lesion involves the left anterior descending artery and a small diagonal branch (arrow).
Fig. 12.5 Slab maximum intensity projection of a diffusely calcified left anterior descending artery (LAD). A high-grade ostial stenosis is present in a medium-size diagonal branch originating at a right angle from the LAD (arrow).
In the era before stents, left main PCI was performed with balloon angioplasty and was associated with inferior angio-graphic and clinical outcomes. The application of stents to left main PCI improves procedural success by decreasing the risk of dissection, acute closure, spasm, and elastic recoil.20 Unfortunately, in-stent restenosis (ISR) remains a potential problem, even with the use of drug-eluting stents. ISR is the result of neointimal hyperplasia within the stent that results in reduction of the vessel lumen. ISR in the left main places a large amount of myocardium at risk and may lead to adverse clinical events. Routine angiographic follow-up is currently recommended for patients treated with left main PCI.20 As the ability of MDCT to image stented segments improves, MDCT may become an alternative to invasive angiography in these patients.
 In-Stent Restenosis and Stent Thrombosis
In-Stent Restenosis and Stent Thrombosis
The advent of coronary stents has led to excellent acute angiographic results and significantly lower rates of angio-graphic and clinical restenosis compared with balloon angioplasty. However, the use of stents is associated with the potential risk for development of ISR and stent thrombosis. ISR is caused by neointimal hyperplasia and, in most patients, presents with symptoms of recurrent ischemia. ISR is seldom associated with an acute coronary syndrome. Conversely, stent thrombosis commonly results in an ST-elevation myocardial infarction and is associated with poor short- and long-term outcomes. The development of drug eluting stents has led to a significant reduction in the incidence of ISR. However, drug-eluting stents are associated with delayed endotheliazation, which may account for a reported increased incidence of stent thrombosis.21
Fig. 12.6 Left main disease in four different patients. (A)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree