Cardiac Magnetic Resonance Imaging
Objectives
At the completion of this chapter, the student should be able to do the following:
Key Terms
Heart disease is one of the leading causes of death in America for both men and women. Any improvement in early diagnosis would surely improve survival and quality of life.
Advances in magnetic resonance imaging (MRI) system hardware and pulse sequence development are resulting in significant advances in cardiac MRI, and it is now becoming an accepted method for a number of cardiac diseases. The types of tissue involved and the variation of motion in the heart make it tough on MRI. Nevertheless, cardiac MRI is helpful in evaluating both congenital and acquired heart disease.
There are three types of tissue in the heart: muscle of the myocardium, fat, and rapidly flowing blood. Each of these tissues has sufficiently different values of T1, T2, and proton density (PD) that cardiac imaging should be easy (Table 26-1).
However, motion gets in the way to complicate MRI. Movement of the diaphragm, the beating heart, and flowing blood result in very complex motion.
Flowing blood within the coronary arteries can be imaged with the techniques of magnetic resonance angiography (MRA). However, the gold standard remains x-ray coronary angiography because it has better spatial resolution and contrast resolution.
Myocardial perfusion can be imaged with the contrast agent gadopentetate dimeglumine (Gd-DTPA) or with the endogenous BOLD (blood oxygen level dependent) technique, although the BOLD technique is largely restricted to research. Cardiac MRI contrast studies are also useful for determining which part of the myocardium is dead, or infarcted.
Radioisotope imaging with thallium (210Th) and/or technetium (99mTc) under stress remains the diagnostic test of choice for assessing myocardial ischemia, but MRI studies are increasing as SPECT studies become less common. Furthermore, MRI can be used to acquire multiple images with good spatial resolution in a heartbeat.
Wall motion imaging with spatially selective presaturation radiofrequency (RF) pulse techniques called myocardial tagging shows great promise for evaluation of myocardial ischemia. Wall position displacement as little as 1.0 mm can be detected, and wall motion abnormalities under stress occur before changes in the electrocardiograph (ECG) or development of chest pain.
The main obstacle to adequate cardiac MRI is respiratory motion. With every breath, the heart moves up 3 cm vertically. Fortunately, breathhold images with good signal intensity and high resolution can be obtained with short breathholds of up to 16 seconds.
When attempting breathhold imaging, the technologist should carefully instruct the patient and direct the patient to practice. Breathholding at the end of inspiration results in considerable variability in heart positioning; breathholding at the end of expiration is preferred. Because not all patients can hold their breath, even for a short time, other methods have been developed to reduce artifacts caused by respiratory motion.
The navigator echo is acquired immediately after each triggering of the ECG. If the diaphragm has moved more than a predefined distance, the signal is rejected and another signal is acquired at the same phase-encoding step.
Although navigator echoes allow good cardiac images to be obtained while the patient is breathing freely, a lot of signals are rejected. The total image time can take two to four times longer than it otherwise would.
Imaging System Requirements
The rapid motion of heart tissue and the movement of blood place exceptional demands on the function of all components of the MRI system. Fast image acquisition requires precisely tuned electronics, robust gradient coils, and a high B0 field intensity.
Several manufacturers have developed MRI systems specifically for cardiac MRI. These systems have short bore design, high B0 field intensity, and strong, fast gradient coils.
Although most MRI systems advertise cardiac MRI capacity, several hardware features are necessary for good cardiac MRI. The following characteristics are essential if the full ability for cardiac MRI is to be achieved.
Static Magnetic Field.
Although cardiac MRI can be done at B0 as low as 0.2 T, 1.5 T is probably the minimum that should be used. The improved signal-to-noise ratio (SNR) at 1.5 T allows for faster imaging and high temporal resolution, even at high heart rates. The temporal resolution at lower field intensity is too low for state-of-the-art physiologic evaluation.
Field of View (FOV) and RF Coils.
A surface coil complement should be available. Dedicated phased array cardiac coils, typically with four to six elements, allow for further improvements in SNR and contrast resolution. Also, in selected instances, they allow use of a small FOV (down to 10 cm) for detailed imaging, though there is reduced coverage because only selected elements of the array are used.
Gradient Coil Capacity.
The gradient coils must be fast and intense. Switching times of not more than 200 µs are required. When energized, the coils must produce a gradient magnetic field of at least 15 mT/m but even higher is better for most applications.
The fastest gradients now allow imaging with repetition time (TR) as low as 2 ms. With single-shot echo planar imaging (EPI) techniques, a 64 × 64 matrix image can be acquired in approximately 50 ms. This limitation is due to the T2 of the myocardium being only approximately 40 ms. Multishot EPI may be used for better spatial resolution.
Imaging Techniques
There are two general approaches to cardiac MRI. ECG-gated, spin echo (SE), and gradient echo (GRE) techniques were the first applications for cardiac imaging and continue to be the standard.
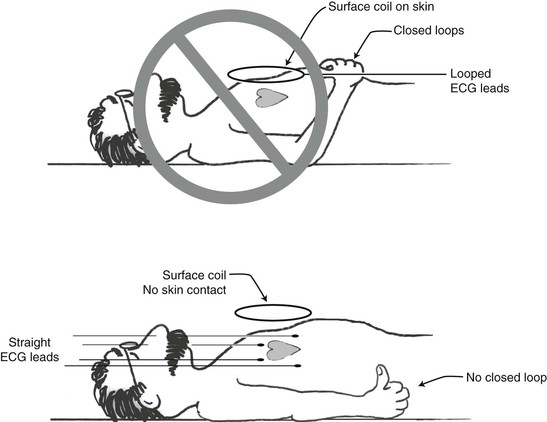
The quality of the ECG gating signal must ensure quality images. Proper placement of the ECG electrodes and the positioning of the ECG cables are necessary. No loops are allowed. Figure 26-1 illustrates proper ECG electrode placement.
Pulsing gradient fields can significantly distort the ECG signal during imaging. It is recommended that the three or four ECG lead wires be braided to reduce these effects. Also, check to ensure that the signal is gating on the R-wave and not the T-wave for optimal image quality.
ECG gating allows the periodic heart motion to be stopped, like a strobe light at a disco dance. In conventional multislice imaging, TR is long and echo time (TE) sufficiently short so that a single acquisition for each slice is obtained within one TR. ECG-gated imaging is similar except the TR approximates the cardiac cycle length.
Most patients have heart rates between 60 and 120 beats/min. These rates correspond to TRs of 1000 ms and 500 ms, respectively.
Because of the short TR, such images are heavily T1 weighted (T1W). A common approach is to make the images more T2 weighted (T2W) by skipping one or more heartbeats and increasing the TR accordingly. Of course, the TE also needs to be lengthened; otherwise, we will have a long TR, short TE sequence that results in a proton density–weighted (PDW) image.
Pulse Sequence Selection
The type of cardiac pulse sequence chosen for a given patient is determined by the objective of the study. Cardiac anatomy is best evaluated with SE MRI. Cardiac function is best evaluated with cineradiography (cine) MRI. Myocardial perfusion requires fast GRE or hybrid EPI sequences.
MRA is usually done with time of flight (TOF) techniques, though velocity-encoded phase contrast (PC) is sometimes used to measure blood flow in the coronary arteries or aorta.
Cine MRI.
A cine loop of one or more cardiac cycles uses spoiled GRE or fast imaging with a short TR (less than 10 ms), a short TE (2 to 4 ms), and a 20° to 30° flip angle. Images are acquired through the cardiac cycle, but only one signal for each image is acquired per cycle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree