10 Cardiac Tumors Primary cardiac tumors are extremely rare, with a reported prevalence of 0.001–0.3% in autopsy studies. Approximately 75% of primary cardiac tumors are benign, while malignancies account for just 25% of cases. The most common benign tumor is myxoma, which constitutes ~50% of all benign cardiac tumors.1–3 Although benign tumors are not locally invasive and do not metastasize, they may cause significant morbidity and mortality due to arrhythmias, embolism, or obstruction of blood flow. Malignant primary cardiac tumors are almost always sarcomas, consisting mainly of angiosarcomas and rhabdomyosarcomas. Metastatic tumors to the heart and pericardium are ~20–40 times more common than primary cardiac tumors and are detectable in 0.6–1.5% of patients with an underlying malignant disease. Metastases occur chiefly in the pericardium and myocardium; valvular and endocardial involvement is extremely rare. The first step in the differentiation of cardiac tumors is to characterize the tumor as a paracardiac, pericardial, myocardial, or intracavitary mass. Fig. 10.1 illustrates various sites of tumor occurrence, and Table 10.1 reviews the sites of the most common benign and malignant cardiac tumors. Table 10.2 lists diagnostic criteria that have proved useful in differentiating between benign and malignant tumors. Three-fourths of all cardiac tumors are benign, and the most common benign tumor is myxoma. Among malignancies, metastases are 20–40 times more common than primary cardiac tumors.
 Essential Point
Essential Point
| Malignant | Benign |
Endocardial, intracavitary | • Angiosarcoma • Other sarcomas • Metastases • Rhabdomyosarcoma* | • Thrombus • Myxoma • Lipoma • Papillary fibroelastoma • Hemangioma |
Intramyocardial | • Metastases • Angiosarcoma • Other sarcomas • Rhabdomyosarcoma* | • Lipoma • Hemangioma • Rhabdomyoma* • Fibroma* |
Pericardial | • Metastases • Mesothelioma • Lymphoma | • Pericardial cyst • Lipoma • Hemangioma • Lymphangioma • Pheochromocytoma • Teratoma* |
Paracardiac | • Lymphoma • Bronchial carcinoma • Pleural mesothelioma • Malignant teratoma | • Bronchogenic cyst • Hemangioma • Teratoma* |
a Tumors marked with an asterisk occur predominantly in children.
| Benign | Malignant |
Internal structure | Homogeneous | Inhomogeneous owing to necrosis and intratumoral hemorrhage |
Attachment to myocardium | Pedunculated | Sessile |
Extent | Limited to one chamber | Involves multiple chambers, extends beyond the heart |
Pericardial effusion | Absent | Frequent, occasionally hemorrhagic |
Other |
| Vascular invasion, pulmonary meta-stases |
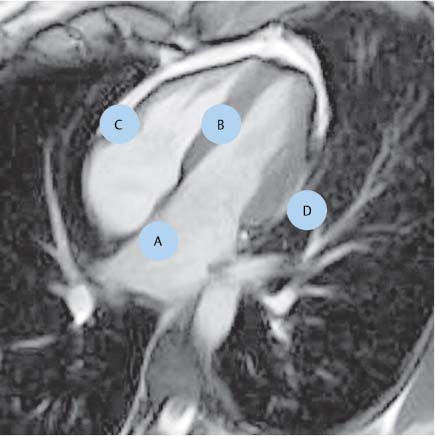
Fig. 10.1 Localization of cardiac tumors: intracavitary (A), intramyocardial (B), intrapericardial (C), and paracardiac (D).
Diagnostic Techniques
The clinical presentation of cardiac tumors is usually nonspecific and is often more suggestive of a systemic disease than a cardiovascular problem. As a result, cardiac tumors were extremely difficult to diagnose before the modern imaging era, and in many cases the diagnosis was only made post mortem. On the other hand, cardiac tumors may present with symptoms such as heart failure, arrhythmias, or arterial emboli that suggest a cardiovascular problem.
Echocardiography, including transesophageal echocardiography, is the current imaging modality of first choice in patients with a suspected cardiac mass. Echocardiography has serious limitations, however, owing to its inability to clearly define mediastinal and paracardiac structures and the potential for poor image quality in patients with obesity or pulmonary emphysema.
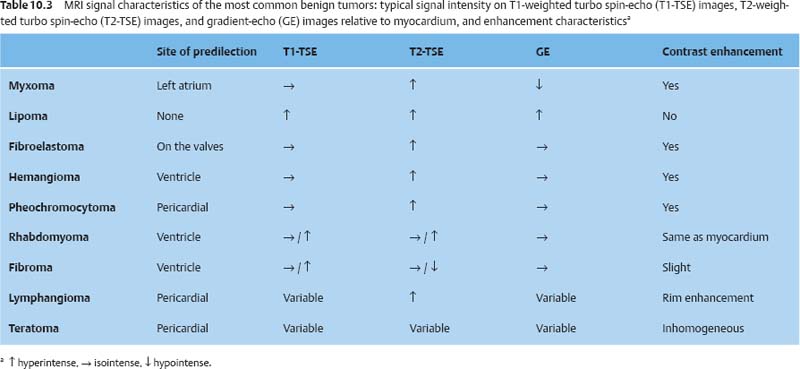
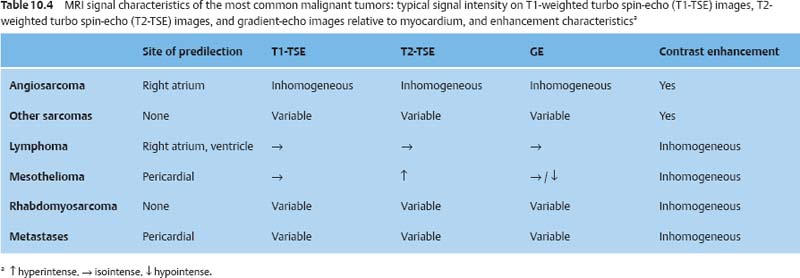
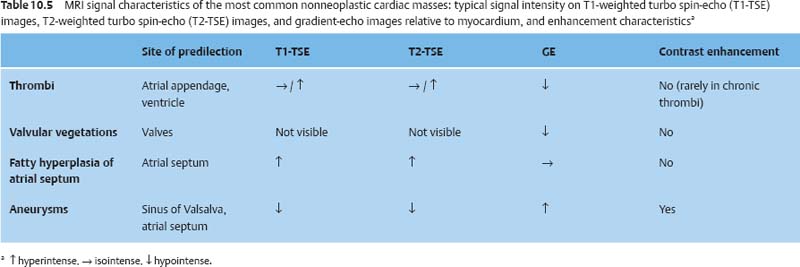
For these reasons, sectional imaging techniques such as CT and MRI are routinely employed for the further investigation of cardiac tumors. Both modalities can evaluate the heart, mediastinum, and lung, but MRI is particularly useful for tissue characterization owing to its excellent soft-tissue contrast. The protocol for cardiac masses includes T1- and T2-weighted sequences, with and without fat suppression, and T1-weighted sequences after intravenous contrast administration (see Chapter 6). The signal characteristics of the most common cardiac tumors are summarized in Tables 10.3–10.5.
 Essential Point
Essential Point
Following administration of Gd-based contrast agents, some tumors can be excellently visualized using inversion-recovery gradient-echo sequences. But if the signal from the tumor is inadvertently nulled, it can mimic an absence of enhancement. For this reason, the protocol for cardiac tumors should always include T1-weighted sequences without an inversion pulse before and after contrast administration.
Benign Primary Cardiac Tumors
Myxoma
Myxomas are the most common primary cardiac tumors and comprise ~50% of all primary cardiac masses. Ninety percent of patients are between 30 and 60 years of age, with a slight female preponderance.4,5 Myxomas tend to occur sporadically, but rarely they occur in the setting of Carney complex—an autosomal dominant condition that includes myxomas, hyperpigmentation of the skin, and extracardiac tumors (pituitary adenomas, fibroadenomas of the breast, schwannomas).
Myxomas often become symptomatic by embolizing to the central nervous system or causing hemodynamic obstruction. Myxomas of the left atrium may produce symptoms of mitral stenosis, while right atrial tumors can mimic the features of tricuspid stenosis on clinical examination.
Additionally, patients with myxomas often have nonspecific clinical symptoms such as fatigue, joint pain, weight loss, and anemia. The cause of these systemic manifestation is unknown.
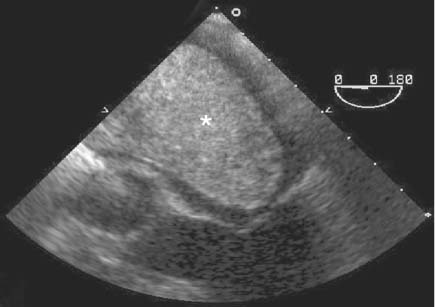
Cardiac myxomas typically arise from the interatrial septum, with 75% of tumors occurring in the left atrium and ~20% in the right atrium.5 Echocardiography typically demonstrates mobile tumors attached to the interatrial septum by a pedicle. Large tumors may occupy almost the entire atrium, however, and may be in broad contact with the atrial wall (Fig. 10.2). Some tumors prolapse through the AV valve into the ventricle during diastole.
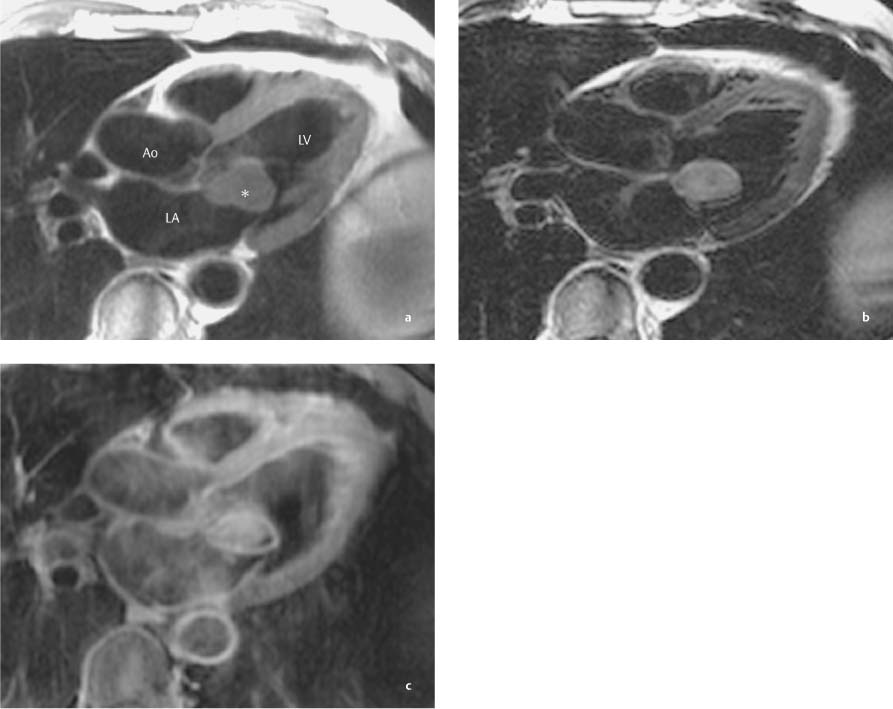
Myxomas often present a homogeneous internal structure on echocardiography, but intratumoral hemorrhage, necrosis, or calcifications may produce an inhomogeneous internal echo pattern. Calcifications are best demonstrated by CT and are found in ~20% of all myxomas. On MRI, myxomas appear iso-intense to myocardium on T1-weighted images. Normally they are hyperintense to myocardium on T2-weighted images, but heterogeneous lesions may rarely have lower signal intensity than the myocardium. Intratumoral hemorrhage in particular may shorten the T2 relaxation time of the mass, causing it to appear hypointense to myocardium. Myxomas show marked, often inhomogeneous enhancement after intravenous contrast administration (Fig. 10.3). Cine MRI can demonstrate tumor mobility in much the same way as echocardiography.
Fig. 10.2 Echocardiogram of a giant myxoma (asterisk) that occupies almost the entire left atrium.
Cardiac Lipoma
There is considerable variation in published reports on the incidence of cardiac lipomas. Some authors call it the second most common tumor in adults,6 while others describe it as extremely rare.7 A potential reason may be the difficulty of detecting small epicardial lipomas. Moreover, some authors do not distinguish between lipomas and lipomatous hypertrophy of the interatrial septum. Cardiac lipomas may occur in any age group but are most prevalent in middle-aged and elderly individuals. Cardiac lipomas are generally asymptomatic and are not associated with clinical syndromes, although there have been a few published cases of multiple cardiac lipomas in children with tuberous sclerosis.
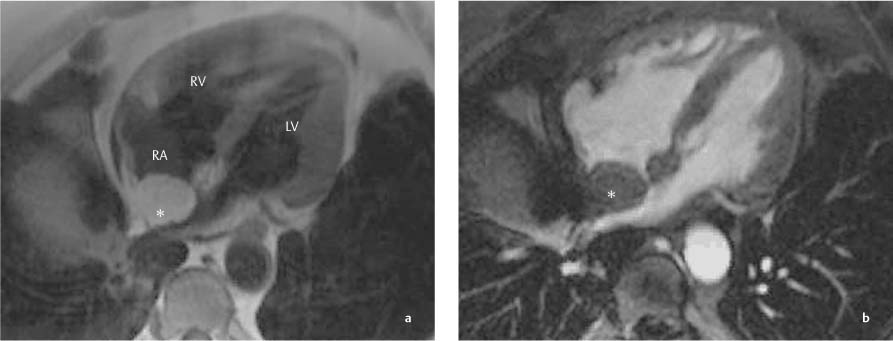
Lipomas are most commonly located in the right atrium or atrial septum but may occur in any heart chamber. Echocardiograms typically show a sharply circumscribed, hypoechoic mass that is broadly apposed to the adjacent wall. Lipomas have a homogeneous CT appearance with an attenuation of approximately –50 HU. Lipomas have high signal intensity in T1-weighted sequences and intermediate signal intensity on T2-weighted images. Cardiac lipomas do not contain foci of calcification, hemorrhage, or necrosis. Lipomas can be positively identified on fat-suppressed MR images (Fig. 10.4). They do not enhance after IV contrast administration.
Fig. 10.3a–c Myxoma (asterisk) that prolapses into the left ventricle in diastole. T1-weighted image (a), T2-weighted image (b), and fat-suppressed T1-weighted image after intravenous contrast injection (c).
Fig. 10.4a, b Lipoma in the right atrium (asterisk). T1-weighted image before contrast administration (a
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree