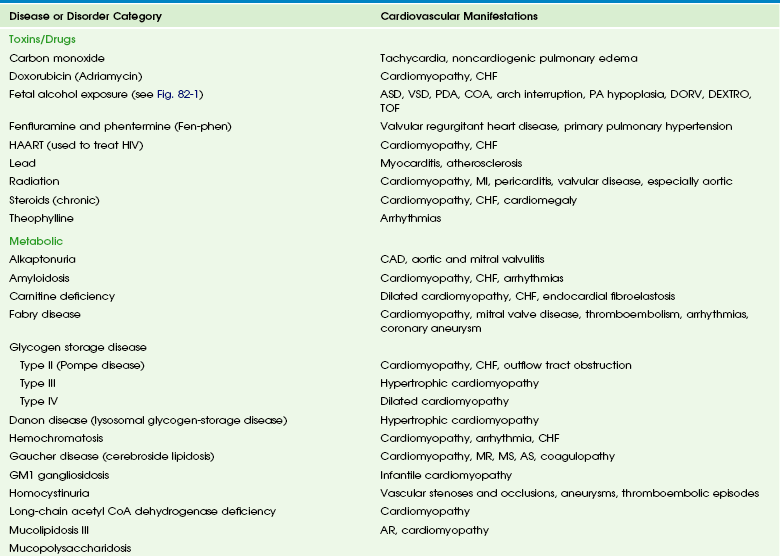
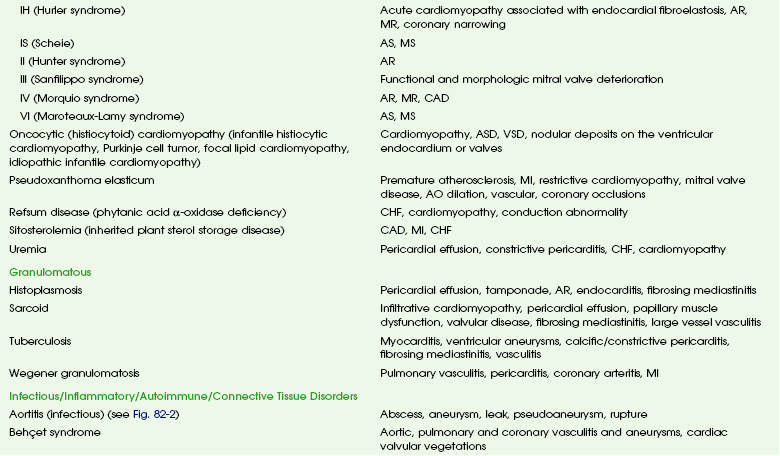
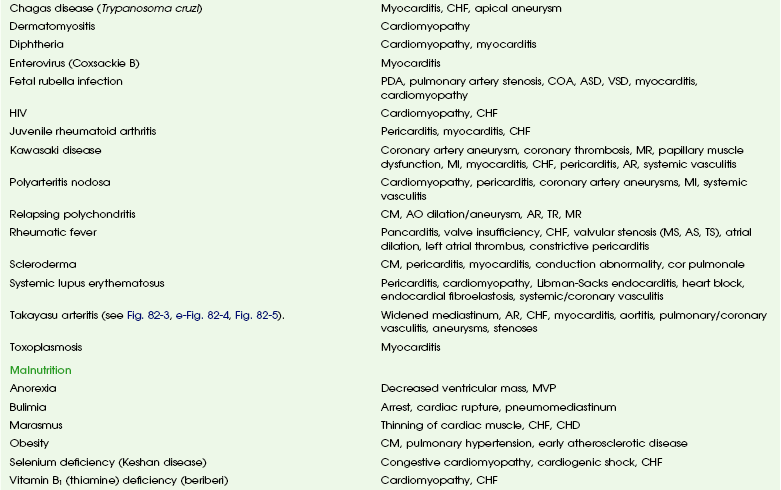
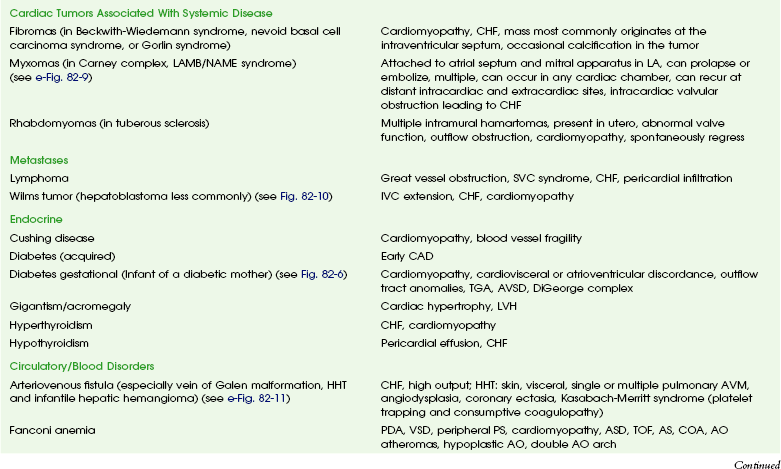
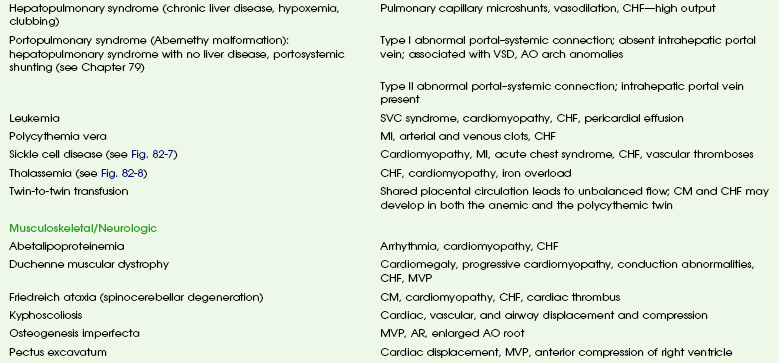
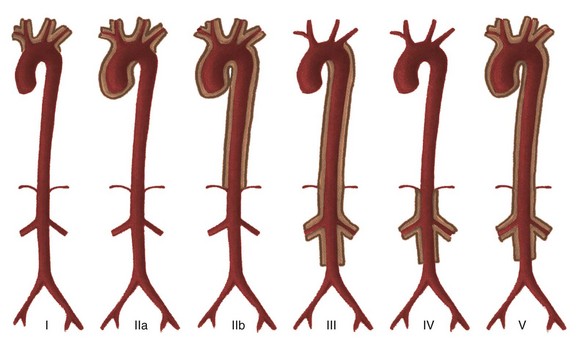
Chapter 82 These entities and the spectrum of their cardiac effects are outlined in Table 82-1. We have included both common diseases that have cardiovascular features and uncommon lesions in which cardiovascular manifestations are prominent. A small number of selected entities are discussed in the following sections. Many of the lesions outlined in Table 82-1 overlap with other chapters and thus are not specifically discussed here. Some well-known syndromes, such as Marfan syndrome, have both cardiac and other organ manifestations, but because they are covered in other chapters, further discussion is omitted here (see Chapter 79). Fetal alcohol syndrome is a common disorder affecting 0.5 to 2.0 per 1000 live births. Affected infants have moderate to severe growth retardation both in the prenatal and postnatal period, along with a characteristic facies. Most children with fetal alcohol syndrome have associated neurologic problems including mental retardation and learning disabilities, as well as altered behavior.1,2 Cardiac malformations are common with fetal alcohol exposure; the most frequent is ventricular septal defect. Other cardiac anomalies include pulmonary artery hypoplasia, coarctation or interruption of the aortic arch, atrial septal defect, patent ductus arteriosus, and tetralogy of Fallot (Fig. 82-1).3 Figure 82-1 Fetal alcohol syndrome and aortic coarctation in a 4-year-old boy. Overview: Acute infectious aortitis in children often is caused by bacterial septicemia originating from infected lines and intravascular devices and from valvular endocarditis or occasionally by direct spread from an adjacent infection or abscess (Fig. 82-2).4 Staphylococci and streptococci are the organisms most frequently responsible for acute infectious aortitis.4,5 Predisposing conditions include congenital heart disease and an immunocompromised state. Once they are in the bloodstream, virulent organisms may adhere to and invade the aortic wall. The resulting inflammation leads to suppurative necrosis that weakens the aortic wall and forms an aneurysm (see Fig. 82-2, A). A contained leak may lead to pseudoaneurysm formation (see Fig. 82-2, B). Staphylococcal aortitis is particularly prone to overt rupture of the aneurysm or pseudoaneurysm and is the most serious complication of infectious aortitis. Fungal agents, especially Aspergillus or Candida, also may be the causative agent of infectious aortitis, especially in immune-compromised individuals.6 Syphilitic and tuberculous aortic aneurysms are rare complications of chronic infection by those organisms and are very uncommon in children. Figure 82-2 Infectious aortitis. Diagnosis of infectious aortitis is difficult because many children with infected aneurysms are asymptomatic or they present with nonspecific complaints, such as fever and abdominal or back pain. Commonly used laboratory markers of infection can be normal. One adult study showed that blood cultures were negative in 28% of cases and white blood cell counts were normal in 42% of cases; however, an elevated erythrocyte sedimentation rate, a nonspecific finding of inflammation, was found in 92% of patients.5 Imaging: Few clinical studies have evaluated the imaging appearance and distribution of infected aortic aneurysms in children. Experience from adult patients suggests that these aneurysms are more often saccular (93%) than fusiform (7%) and can be distributed throughout the course of the aorta: 6% in the ascending aorta, 23% in the descending thoracic, 19% in the thoracoabdominal aorta, 10% in the juxtarenal aorta, and 32% in the infrarenal aorta.7 Periaortic fluid, stranding, or a soft tissue mass was present in 48% of patients with infectious aortitis. Periaortic gas, a specific sign, was present in only 7%. Rapid progression of aneurysm size was found in infected aneurysms in both adults and children.7 Computed tomographic angiography (CTA) and magnetic resonance angiography (MRA) imaging have largely supplanted conventional angiography in the diagnosis of aortic aneurysms and their complications (see Fig. 82-2). Ultrasound may be an initial screening examination but usually is not definitive enough to support management decisions. Treatment: Antibiotic treatment with the goal of eradicating the offending organism is the first step in the treatment of infectious aortitis.5 At the same time, imaging to document stability of the aortic lumen is necessary. If an aneurysm has formed, it should be surgically repaired after an adequate period of antibiotic treatment.4,5 Deployment of endovascular stent grafts in infected aortic aneurysms has been attempted.8 Although this deployment is not considered a treatment of choice, it may be useful to act as a bridge to open surgical repair, especially in the presence of low-virulence organisms or rapidly expanding aneurysms. Overview: Takayasu arteritis, also known as pulseless arteritis, is a chronic inflammatory arteritis of large vessels.9 The aorta is the artery that is most commonly involved, with the abdominal aorta involved in 59% to 75% of cases and the thoracic aorta involved in 40% to 56% of cases. Takayasu arteritis involvement is more common in the systemic arteries than in the pulmonary arteries.10 Takayasu arteritis is a rare disease, occurring in 2.6 per 1 million people in North America.11 It is more common in patients of Asian descent, and females make up 80% to 90% of patients. Diagnosis of Takayasu arteritis is based on patient symptoms, physical findings, clinical laboratory values, serologic markers, and vascular findings.9 The American College of Rheumatology criteria include arm or leg claudication, age younger than 40 years, a blood pressure difference between extremities of greater than 10 mm Hg, subclavian or aortic bruit, decreased brachial artery pulse, and aortic or branch narrowing.12 Three of these criteria provide a diagnosis of Takayasu arteritis with a sensitivity of 90.5% and a specificity of 97.8%.11 Other clinical manifestations of Takayasu arteritis that are not involved in diagnosis include fever, headache, neurologic symptoms including stroke, postural dizziness, arthralgias, weight loss, myalgias, and systemic or pulmonary hypertension.11,13 Takayasu arteritis has a triphasic pattern: a systemic nonvascular phase, a vascular inflammatory phase, and a quiescent “burnt out” phase, although the inflammatory and fibrotic changes often overlap.10,11 In children, a long delay often occurs before Takayasu arteritis is diagnosed, especially when systemic symptoms predominate.11,13,14 The lesions of Takayasu arteritis are segmental with a patchy distribution. The vasculitis can lead to stenosis, occlusion, and aneurysm formation.10 Severe stenosis or occlusive thrombosis of the pulmonary vasculature may lead to pulmonary infarction and pulmonary hypertension.15 Cardiac symptoms include aortic regurgitation, dilated cardiomyopathy, myocarditis, pericarditis, congestive heart failure, and myocardial ischemia. Etiology and Classification: The specific cause of Takayasu arteritis is unknown, but it is probably a T-cell–mediated autoimmune process. Infection, particularly tuberculosis, has been linked to the development of Takayasu arteritis, especially in children.13 The diseased vessel wall is thickened and shows granulomatous changes from the adventitia to the media. Giant cell (or temporal arteritis) has an identical pathologic appearance to Takayasu arteritis but affects an older population and typically involves the temporal artery.16 Takayasu arteritis currently is divided into six types depending on the location of aortic involvement. Coronary (C+) or pulmonary (P+) involvement may occur in all types (Fig. 82-3).10
Cardiovascular Involvement by Systemic Diseases
Toxins/Drugs
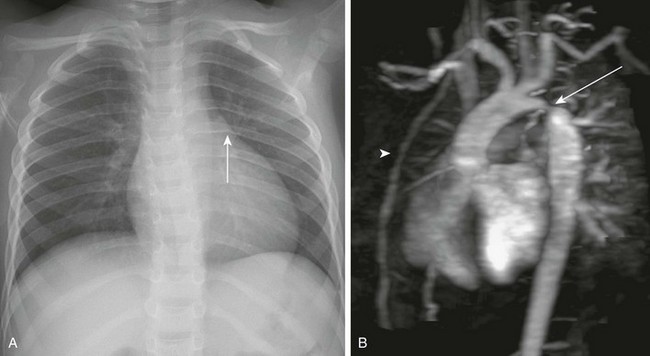
A, A chest radiograph shows a prominent aortic arch and descending aorta. Notching of the posterior left sixth rib (arrow) from an intercostal aortic collateral vessel is present. B, Oblique sagittal three-dimensional magnetic resonance angiography image demonstrates marked coarctation of the aorta (arrow) distal to the left subclavian artery. Multiple large intercostal collateral vessels are present, as well as enlarged internal mammary collaterals (arrowhead).
Infectious, Inflammatory, and Autoimmune Disorders
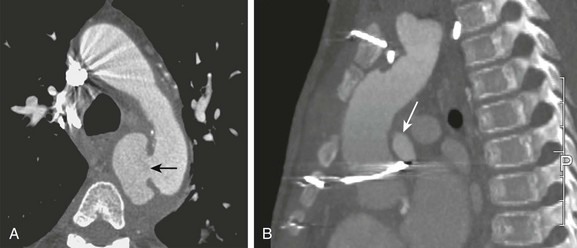
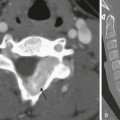
A, Axial image from a computed tomography angiogram (CTA) shows a thick-walled saccular aneurysm communicating with the aortic arch through a narrow opening (arrow). B, An 8-year-old child after repair of aortic coarctation and aortic stenosis with prosthetic aortic valve replacement whose postoperative course was complicated by Staphylococcus aureus mediastinitis. A sagittal maximal intensity projection image from a gated CTA demonstrates a small posterior aortic pseudoneurysm (arrow) adjacent to the aortic valve. Note diffuse anterior soft tissue edema/inflammation.
Takayasu Arteritis