Fig. 8.1
The carpal tunnel is an osseofibrous channel (a) located in the volar portion of the wrist. The floor of the tunnel is formed by the carpal bones; the roof by the flexor retinaculum (B, D: Axial T1-weighted MRI scan; C, E: ultrasound). The tendons of the flexor pollicis longus (Flp), the superficial (Fs) and deep (Fp) flexors of the fingers, and the median nerve (Nm) all run through the carpal tunnel. The retinaculum (arrows) extends from its proximal insertions on the scaphoid tuberosity and pisiform bone (b, c) to its distal insertions on the trapezium and the hook of the hamate (arrows) (d, e). The sonographic appearance is that of a hypoechoic ribbon-like structure (C, E); on T1-weighted MRI sequences the band appears hypointense (B, D). Right above the roof of the carpal tunnel (B, C) lie the tendon of the flexor carpi radialis (Frc), which inserts into the scaphoid, the tendon of the flexor carpi ulnaris, the ulnar artery (Au), and the ulnar nerve (Nu)
Nine tendons and one nerve—the median—run through this tunnel (Fig. 8.1). The flexor pollicis longus tendon has its own sheath, but the superficial and deep flexors of the fingers share a common sheath.
Outside the carpal tunnel (Fig. 8.1b, c)—but in close contact with it—is the flexor carpi radialis tendon, which inserts into the scaphoid, the flexor carpi ulnaris tendon, which inserts into the pisiform, and the tendon of the palmaris longus, which is continuous with the palmar fascia or inserts into the flexor retinaculum.
Ultrasound examinations of the carpal tunnel are generally done along the short axis of the tendons. The examination normally begins with exploration of the median nerve at the level of the forearm. Here, the median nerve lies between the superficial and deep flexors of the fingers and presents the fasciculated appearance typical of nerves. As it proceeds peripherally, the nerve becomes more superficial and intimately associated with the flexor carpi radialis tendon. It then passes through the carpal tunnel in a superficial position, right beneath the flexor retinaculum [1, 2] (Fig. 8.1). At this level, the median nerve lies above the flexor pollicis longus and the laminae of the flexor digitorum superficialis that insert into the index and middle fingers. Dynamic studies are also useful for assessing nerves. Nerve movement can be classified as active or passive. Under normal conditions, when the patient moves his/her fingers, the median nerve moves passively and adapts to the free space, and movements that involve the brachial plexus result in active movement of the median nerve as well. The small palmar cutaneous branch of the median nerve (Fig. 8.2) arises at the level of the wrist, passes over the flexor retinaculum, continues on toward the flexor carpi radialis tendon, and innervates the cutaneous and subcutaneous tissues of the palm. Exploration of this nerve branch is important, particularly when surgery is being planned, because in some individuals it arises from the ulnar side of the median nerve, and its course toward the flexor carpi radialis tendon is extremely superficial. In this configuration, the palmar cutaneous branch of the median nerve is at risk for accidental resection during surgical incision of the flexor retinaculum.
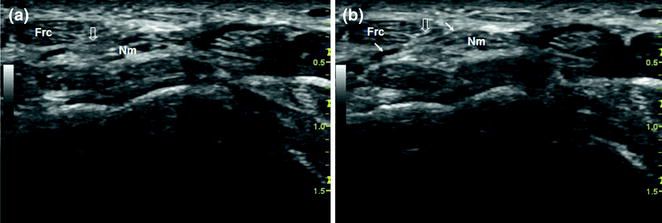
Fig. 8.2
The median nerve and its palmar cutaneous branch. At the level of the wrist, the median nerve (Nm) divides, giving rise to a small palmar cutaneous branch (a) (open arrow) that crosses over the flexor retinaculum (b) (arrows), proceeds on toward the flexor carpi radialis tendon (Frc), and ultimately innervates the cutaneous and subcutaneous tissues of the palm
The second structure that needs to be examined is the flexor pollicis longus tendon. It is easy to recognize because of its position within the carpal tunnel (at the radial most border) and its oval-shaped cross section (Fig. 8.1). Its identification is facilitated by having the patient flex his/her thumb.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree