Fig. 20.1
Occult fracture of the third finger. X-rays (a, b) showed no evidence of a fracture, but a small sliver could be seen in the proximal phalanx of the second finger. Ultrasound (c) revealed a fracture of the third metacarpal head (arrow), a hematoma surrounding the fracture, and conflict with the extensor tendon (Est ten)
In patients with pain and swelling after trauma to the extremities, ultrasound examination of the bone surfaces is important for diagnosing occult or undetected fractures [1].
20.2 Intersection Syndrome with Fluid in the Sheaths of the Second and Third Compartments
A 38-year-old patient presented with pain in the distal portion of the dorsal forearm, where the musculotendinous junction of the abductor pollicis longus and extensor pollicis brevis crosses over the extensor tendons of the second compartment. Ultrasound revealed an effusion within the sheaths of the second and third compartments (Fig. 20.2). The fluid in the latter compartment may have been the result of communication between the second and third compartment sheaths.
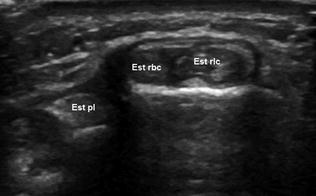
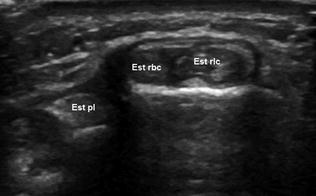
Fig. 20.2
Intersection syndrome. Ultrasound shows fluid within the sheaths of the second compartment (Est rlc—Est rbc) (intersection syndrome) and the third (Est pl) compartment (The third compartment effusion may reflect communication between the second and third compartment sheaths)
The sheaths of the dorsal extensor tendons begin above the upper edge of the extensor retinaculum. Each compartment usually contains a single synovial sheath, but areas of communication may exist between the sheaths of the second, third, and fourth extensor tendon compartments [2].
20.3 Allergic Tenosynovitis of the Extensor Tendons
A 32-year-old patient was operated on for a ganglion of the radiocarpal joint and developed an allergic reaction to the sutures. Clinically, he presented with pain and swelling on the volar side of the wrist. Ultrasound showed tenosynovitis of the extensor digitorum communis, extensor indicis proprius, and extensor carpi radialistendons (Fig. 20.3).
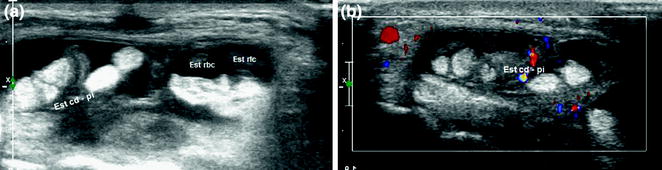
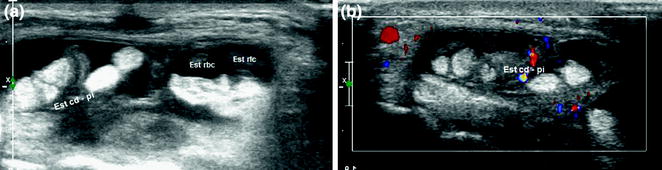
Fig. 20.3
Allergic tenosynovitis of the extensor digitorum communis, extensor indicis proprius (Est cd-pi), and extensor carpi radialis brevis and longus (Est rbc and Est rlc) tendons. Sonography shows fluid within the tendon sheaths (a) and hypervascularization (b)
Tenosynovitis is characterized by inflammation of the synovial sheath. Sonography is a valuable tool for diagnosing and evaluating damage to the extensor tendons and their sheaths [3].
20.4 De Quervain’s Disease in a 9-Year-Old Girl
A 9-year-old ballet dancer presented with pain over the right radial styloid that was exacerbated by movement of the thumb. Sonography showed hypoechoic thickening of the retinaculum, fluid within the sheath of the extensor pollicis brevis tendon, and fibrous septation of the first compartment. The abductor pollicis longus tendon had multiple terminal laminae (Fig. 20.4).
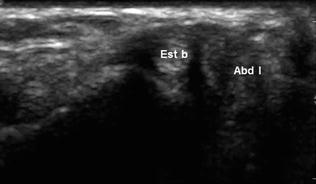
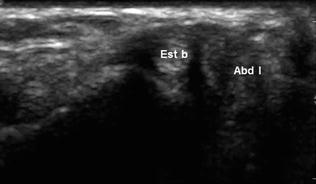
Fig. 20.4
De Quervain’s disease. Sonography shows hypoechoic thickening of the retinaculum and fluid within the sheath of the extensor pollicis brevis tendon (Est b) in a patient with fibrous septation of the first compartment. The abductor pollicis longus tendon (Abd l) has multiple terminal laminae
Anatomic studies have documented the existence of variations in the number of tendons and the division of the first extensor compartment. Sonography can be used to identify several types of anatomic variations in patients with de Quervain’s disease [4].
20.5 Intersection Syndrome in a Patient with Tenosynovitis Involving Only the Extensor Carpi Radialis Brevis
In this patient with left distal forearm pain, ultrasound disclosed an effusion within the sheath of the extensor carpi radialis brevis tendon (Fig. 20.5).
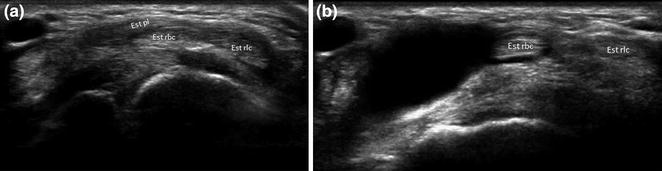
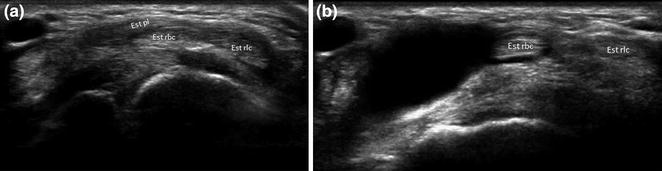
Fig. 20.5
Intersection syndrome in a patient with tenosynovitis involving only the extensor carpi radialis brevis (est rbc). Ultrasound shows fluid distal to the point of decussation (a) in the sheath of the extensor carpi radialis brevis (Est rbc) tendon (b)
Intersection syndrome is an overuse disorder of the dorsal distal forearm.It presents with pain and tenderness in the area where the musculotendinous junctions of the abductor pollicis longus and extensor pollicis brevis cross over the extensor tendons of the second compartment, or where the extensor pollicis longus tendon passes over the extensor tendons of the second compartment [2]. The sheath of the radial carpal extensors originates above the upper edge of the extensor retinaculum, 0.5–1 cm from the insertion; it then divides into two separate sheaths, one for each tendon [5].
20.6 Wartenberg’s Syndrome After Cephalic Vein Cannulation
A 72-year-old patient developed pain and paresthesias over the lateral aspect of the wrist after cephalic vein cannulation. Sonography showed enlargement and hypoechogenicity of a branch of the radial nerve (Fig. 20.6).
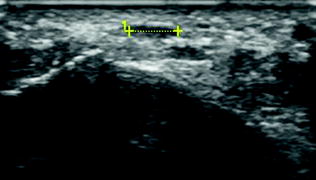
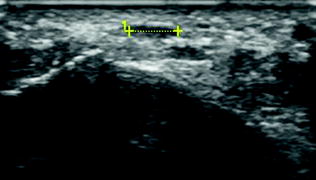
Fig. 20.6
Wartenberg’s syndrome. On sonography a branch of the radial nerve appears enlarged and hypoechoic (caliper)
The superficial branch of the radial nerve divides into three separate branches at the level of the proximal intersection. Nerve injury at this level can be caused by Colles’ fractures, penetrating trauma, or cephalic vein cannulation [6].
20.7 Flexor Carpi Radialis Tenosynovitis in a Patient with Reversed Palmaris Longus
This 21-year-old patient with volar wrist swelling from birth presented with sudden-onset radial pain. Clinical diagnosis: carpal tunnel syndrome. Sonography revealed reversal of the palmaris longus (Fig. 20.7a) and flexor carpi radialis tenosynovitis (Fig. 20.7b).
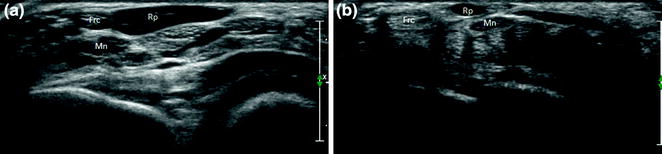
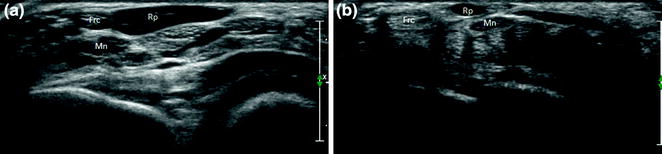
Fig. 20.7
Flexor carpi radialis tenosynovitis in a patient with reversed palmaris longus. Sonography shows the reversed palmaris longus (Rp) and flexor carpi radialis (Frc) tenosynovitis. There is no median nerve (Mn) enlargement
A reversed palmaris longus may cause a compartment syndrome in the wrist area, carpal tunnel syndrome, and Guyon’s canal syndrome [7].
20.8 Carpal Tunnel Syndrome in a Patient with a Bifid Median Nerve
A 34-year-old patient with symptoms of median nerve compression in the carpal tunnel. Ultrasonography showed tenosynovitis of the flexor tendons and an anatomic variation of the median nerve (bifid median nerve) (Fig. 20.8).
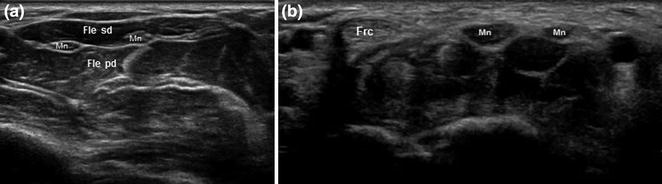
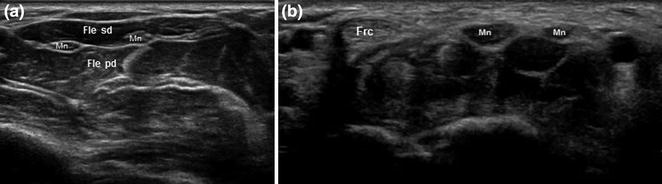
Fig. 20.8
Carpal tunnel syndrome in a patient with a bifid median nerve. Ultrasonography shows an anatomic variation of the median nerve (Mn) (bifid median nerve) (a) and tenosynovitis of the flexor tendons (Fle sd, Fle pd, Frc) (b). The median nerve appears enlarged and hypoechoic
High division of the median nerve proximal to the carpal tunnel (bifid median nerve) has an incidence rate of 2.8 %. Bifid median nerves can cause carpal tunnel syndrome because of their larger cross-sectional area, but other causes should be considered in patients with unilateral symptoms [8].
20.9 Post-traumatic Palmar Cutaneous Nerve Encasement
A 36-year-old patient presented with volar wrist pain several days after experiencing penetrating trauma. Sonography revealed scar tissue encasement of the palmar cutaneous branch of the median nerve (Fig. 20.9).
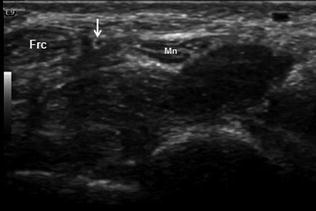
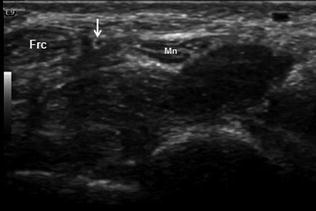
Fig. 20.9
Palmar cutaneous nerve encasement after trauma. Sonography reveals encasement of the palmar cutaneous branch (arrow) of the median nerve (Mn) by scar tissue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree