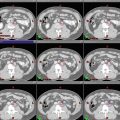
Fig. 1
Potential sites of occult primary tumor in SQCUP. The red circle represents the level of the isocenter for an intensity modulated radiation therapy plan for squamous cell carcinoma of unknown primary. The red dotted lines delineate the anatomical divisions between the nasopharynx, oropharynx and larynx and hypopharynx, respectively
The most common primary sites that are eventually identified upon workup for patients with SQCUP are the tonsils and base of the tongue (~90 %) (Cianchetti et al. 2009).
The distribution of lymph node metastases from a SQCUP of the head and neck is shown in Fig. 2. The most common sites of involvement are levels II and III.
2 Diagnostic Workup Relevant for Target Volume Delineation
A thorough workup is necessary to rule out a site of origin before proceeding with a diagnosis of an unknown primary. At a minimum, this should consist of a careful physical examination including testing of the cranial nerves; fiberoptic examination visualizing the nasopharynx, oropharynx, larynx, and hypopharynx; and cross-sectional imaging with at least a high-resolution CT scan with contrast. Obtaining a careful patient history, including a smoking history, is also critical to determine risk factors for cancer and to consider possible infraclavicular primary sources (e.g., thoracic, gynecologic, or gastrointestinal). Panendoscopy may also be useful.
HPV and EBV testing should be performed to help determine possible primary locations.
Directed biopsies of all suspicious lesions in the pharyngeal axis are mandatory; blind biopsies of normal-appearing mucosa have tradiationally been recommended but are only occasionally helpful in identifying the primary tumor.
PET/CT is able to identify the primary site in 25 % of tumors that are undectected by other modalities, with a sensitivity, specificity, and accuracy of 88.3, 74.9, and 78.8 %, respectively (Rusthoven et al. 2004).
PET/CT should be performed before biopsy when possible to decrease the incidence of false-positive findings.
The chapter on lymph node contouring in the head and neck contains further details of diagnostic imaging to assess lymphatic involvement.
3 Simulation and Daily Localization
Set up the patient in supine position with head extended. The immobilization device should include at least the head and neck. If possible, shoulders should also be immobilized to ensure accurate patient setup on a daily basis especially when an extended-field IMRT plan is used.
CT simulation using 3 mm thickness with IV contrast should be performed to help guide the GTV and CTV targets, particularly for the lymph nodes. We typically recommend a simulation scan from the top of the head including the brain to the carina. Five millimeter thickness can be reconstructed below the clavicle to the level of the carina.
Image registration and fusion applications with MRI and PET scans should be used to help in the delineation of target volumes, especially for regions of interest encompassing the GTV, skull base, brainsteam, and optic chiasm. The GTV and CTV and normal tissues should be outlined on all CT slices in which the structures exist.
4 Target Volume Delineation and Treatment Planning
Treatment to the bilateral neck and areas of pharynx at risk for harboring a primary is typically recommended.
Generally, cervical lymph nodes (levels IB-V) and retropharyngeal nodes should be included for the node-positive neck. For the contralateral neck, nodal levels II–IV and the retropharyngeal nodes should be targetted to a prophylactic dose (50–54 Gy). Inclusion of level IB and V can be considered on a case-by-case basis.
Irradiation of the ipsilateral neck alone is controversial. Several single institutional reports have shown a low risk of contralateral neck failure and no difference in disease-free or overall survival when an ipsilateral approach is used (Grau et al. 2000; Ligey et al. 2009; Lu et al. 2009; Perkins et al. 2012; Weir et al. 1995), whereas other studies have demonstrated improved outcomes with more extensive treatment volumes (Reddy and Marks 1997).
The extent of the pharynx to irradiate must be determined on a case-by-case basis and remains an area of active investigation. The pattern of lymph node spread can further help guide decisions on how much of the pharynx to treat.
Some authors have advocated sparing the larynx when there are no low lymph nodes involved (Barker et al. 2005) (see Fig. 7).
Irradiating the oropharynx alone may be sufficient for an HPV + patient; however, the nasopharynx should be included if there is any suspicion of a nasopharyngeal primary, as recent data demonstrated poor outcomes for patients with HPV + nasopharyngeal carcinoma (Stenmark et al. 2013).
EBV + patients may only need treatment to the nasopharynx.
When in doubt, the entire pharynx should be treated.
In the postoperative setting, concurrent chemotherapy should be considered when extracapsular extension is present (ECE). In the definitive setting, advanced nodal disease is a consideration for concurrent chemotherapy.
Table 1
Suggested target volumes
Target volumes | Definition and description |
|---|---|
GTV70 a (The subscript 70 denotes the radiation dose delivered) | All lymph nodes ≥1 cm in short axis, significantly FDG avid, or positive on biopsy. Contour any lymph nodes in doubt as GTV |
PTV70 a | GTV70 + 3–5 mm depending on institutional accuracy of daily patient positioning |
CTVnasopharynx b | Extends from the base of skull superiorly to the soft palate inferiorly. Anteriorly extends from the posterior choana to the posterior pharyngeal wall. Laterally ensure adequate coverage on the fossa of Rosenmüller |
CTVoropharynx b | Extends superiorly from the surface of the soft palate to the floor of the vallecula inferiorly (or hyoid bone). Anteriorly, the base of tongue should be covered; however, an additional margin covering the oral tongue is not necessary. Laterally, the tonsils should be covered adequately. Posteriorly, the entire pharyngeal wall should be covered |
CTVlarynx&hypopharynx b | Extends superiorly from the hyoid bone to the bottom of cricoid cartilage |
PTVmucosa b | A 3–5 mm expansion on the mucosal surface CTVs depending on institutional accuracy of daily patient positioning |
CTVneck nodes c | RPN, levels IB-V in the node-positive neck. RPN, levels II–IV on the node-negative neck |
PTVneck nodes c | A 3–5 mm expansion on the neck node CTVs depending on institutional accuracy of daily patient positioning |