Chest: Nontrauma
Bruce E. Lehnert
Eric J. Stern
GENERAL CONSIDERATIONS
Imaging plays a critical role in evaluating nontraumatic pathology in the chest because physical exam findings may not be reliable and the patient’s symptoms are often not specific to a particular disease state. The chest radiograph remains the first-line imaging modality for evaluating the chest and often allows for rapid clarification or confirmation of clinically suspected pathology such as pneumonia, edema, and pleural gas or fluid or may suggest the need for cross-sectional imaging such as in the setting of an abnormal mediastinum in a patient with chest pain.
The clinical presentation of acute vascular pathology in the chest is often nonspecific, and an accurate evaluation of emergent vascular disease in the chest is typically not possible with clinical exam and chest radiography. The recent widespread availability of multidetector computed tomography (MDCT), which allows rapid, detailed imaging of the chest, has revolutionized the imaging workup of acute chest pathology, particularly in the setting of suspected acute aortic syndrome (AAS), pulmonary embolus, and most recently in suspected acute coronary syndrome (ACS). Magnetic resonance imaging (MRI) technology has also advanced significantly; however, the use of this modality in evaluating chest pathology in the emergency room is generally limited to a problem-solving role, particularly in the evaluation of AAS.
The current chapter reviews both the radiographic and cross-sectional imaging features of thoracic pathology germane to the evaluation of patients presenting with signs and symptoms of nontraumatic disease of the chest. The radiographic and MDCT features of acute lung pathology including aspiration, infection, exacerbation of chronic obstructive airway disease, edema, and alveolar damage, as well as pleural pathology and mediastinitis, are reviewed. MDCT applications to vascular imaging in the setting of AAS, pulmonary embolus, and ACS are reviewed as well as potential emergent complications of aortic stent grafting.
Lungs
A comprehensive review of diseases affecting the lungs is beyond the scope of the current discussion; however, acute pathology relevant to the emergency department (ED) setting is addressed. Recognizing and accurately diag nosing acute nontraumatic pathology in the chest can be instrumental in directing appropriate therapy. The imaging features associated with aspiration, pulmonary infection in immunocompetent and immunocompromised patients, tuberculosis (TB), pulmonary abscess, atelectasis, foreign body aspiration, edema, and alveolar damage are reviewed.
Aspiration
Aspiration pneumonitis refers to the pulmonary reaction to a foreign substance aspirated into the tracheobronchial tree and is a common problem in patients presenting to the ED. Gastric contents
and oral secretions are the most commonly aspirated substances and risk factors include neurologic deficit, decreased level of consciousness, alcoholism, seizure, esophageal disease, and nasogastric or endotracheal intubation. Aspiration pneumonitis may present clinically with fevers, shortness of breath, and hypoxemia, which can be clinically difficult to differentiate from infectious pneumonia.
and oral secretions are the most commonly aspirated substances and risk factors include neurologic deficit, decreased level of consciousness, alcoholism, seizure, esophageal disease, and nasogastric or endotracheal intubation. Aspiration pneumonitis may present clinically with fevers, shortness of breath, and hypoxemia, which can be clinically difficult to differentiate from infectious pneumonia.
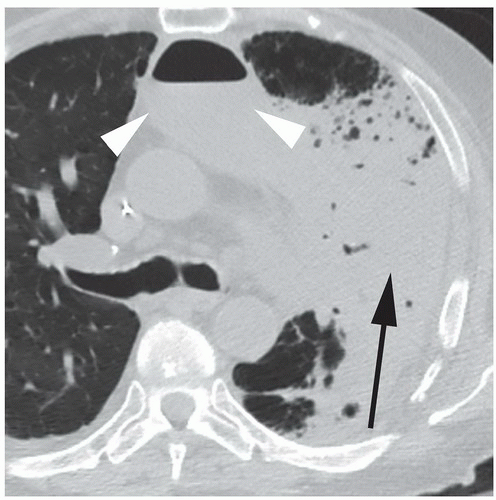
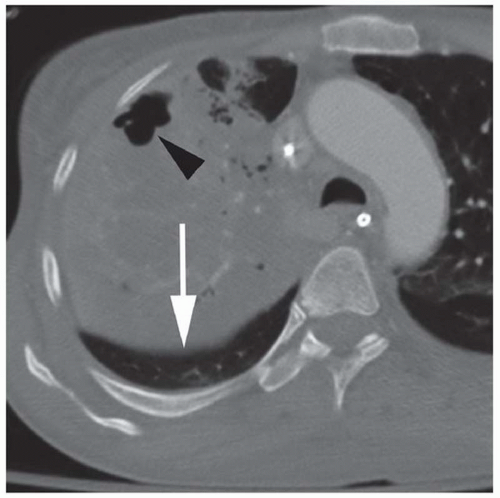
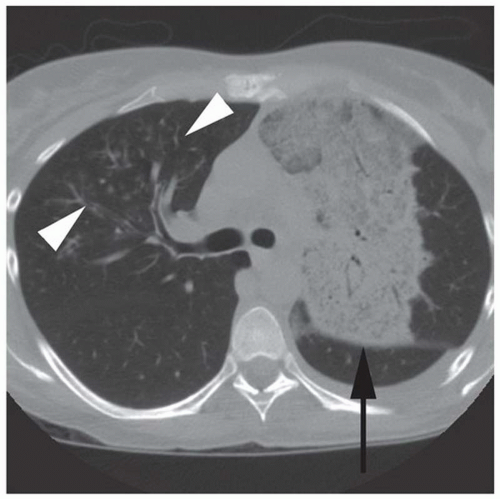
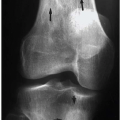
The distribution of imaging abnormalities resulting from aspiration are typically gravitationally dependent. In a supine position, this includes the right upper lobe apical and posterior segments, the left upper lobe apical posterior segment, and the superior segments on the lower lobes (Fig. 12.1).
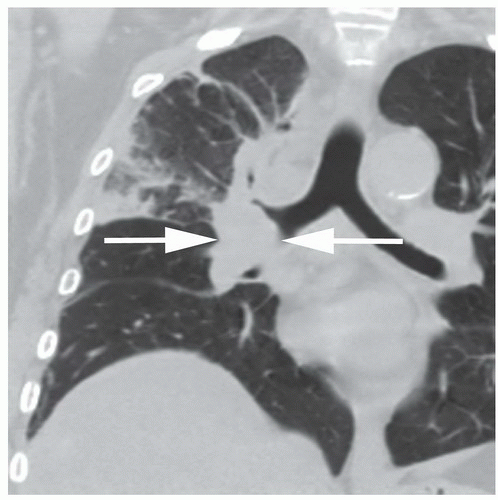
The radiographic appearance of aspiration is also dependent on the type of aspirated material, volume of the aspirate, and on the time interval since the aspiration event. Aspiration of nonirritating substances such as neutralized gastric contents, secretions, blood, and water does not incite an inflammatory response. This so-called bland aspiration results in a gravitationally dependent segmental or subsegmental distribution of patchy opacities that clear rapidly with coughing or ventilation. Aspiration of acids, caustic material, vegetable matter, fatty acid, or hyperosmolar material may result in an inflammatory response manifesting as gravitationally dependent hazy nodules or confluent consolidation in a bronchovascular distribution (Fig. 12.2).
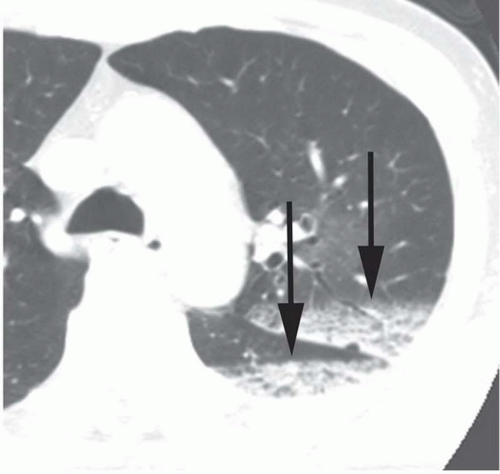 Figure 12.1. Aspiration. Axial CT image illustrates the dependent “settling” of aspirated material into the left upper lobe and the left lower lobe (arrows). |
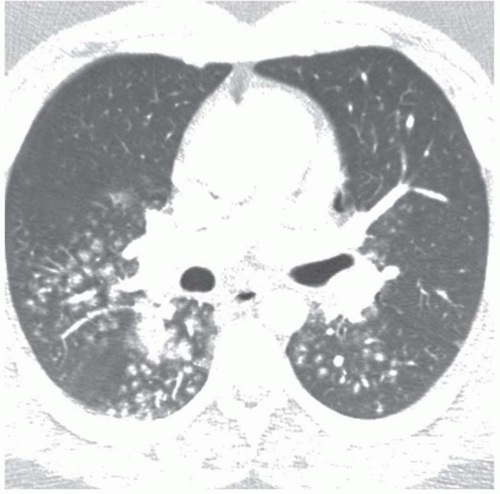 Figure 12.2. Aspiration pneumonitis. Rounded, hazy nodules in a bronchovascular distribution in lower lobes and dependent segments of the right upper lobe are typical of aspiration pneumonitis. |
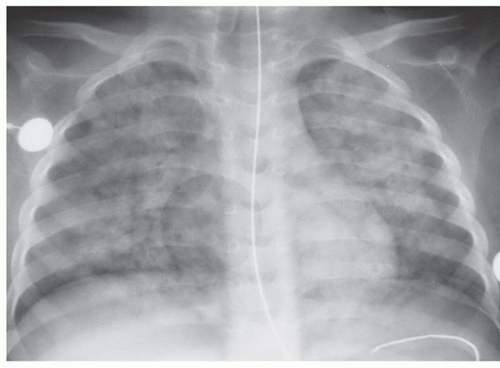
Another form of aspiration is seen in patients who suffer near-drowning events, which results in water filling alveoli. The clinical significance of water aspiration is more closely related to volume than to whether the aspirate is freshwater or saltwater. The radiographic features of mild near drowning are similar to those of aspiration, such as patchy, irregular perihilar opacities with relative sparing of the periphery. More severe radiographic manifestations of near drowning include diffuse, confluent fluffy opacities similar in appearance to pulmonary edema (Fig. 12.3). Computed tomography (CT) findings in near- drowning patients include bilateral patchy or diffuse areas of ground-glass attenuation as well as ill-defined centrilobular nodularity.
Smoke inhalation is the primary cause of death in victims of indoor fires, with approximately 50% to 80% of fire deaths demonstrating burns to the upper respiratory system. Inhalation injury also contributes significantly to the morbidity of burn survivors because it can result in acute lung injury and the development of acute respiratory distress syndrome (ARDS). The golden standard for diagnosing acute smoke inhalation injury remains bronchoscopy. Acute smoke inhalation typically produces no recognizable changes on the initial chest x-ray (CXR), even with blood carboxyhemoglobin levels as high as 50%. CT may
show ground-glass opacities in a peribronchial distribution and/or patchy peribronchial consolidations as early as a few hours after the inhalation injury.
show ground-glass opacities in a peribronchial distribution and/or patchy peribronchial consolidations as early as a few hours after the inhalation injury.
Obstructive Lung Disease
The most common obstructive lung diseases include asthma, emphysema, and chronic bronchitis. These conditions are among the leading causes of mortality and morbidity in the United States and are frequently treated in the emergency setting.
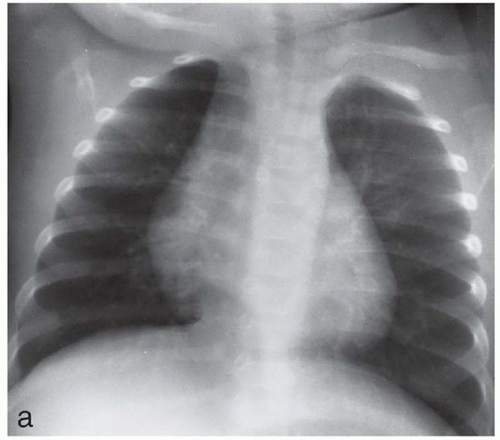
Asthma affects up to 5% of the US population. The disease is characterized by increased airway reactivity to a variety of stimuli, airway inflammation with associated increased mucus exudate, and episodes of at least partially reversible smooth muscle-mediated bronchospasm resulting in small airway obstruction. The radiographic appearance of asthma predominantly includes increased lung volumes with the various manifestations of air trapping such as horizontal positioning of the posterior portions of the upper ribs and visible, bulging intercostal spaces; flattening and depression of the diaphragms; and an increase in the anteroposterior (AP) diameter of the chest. In infants and young children, a radiograph that appears to have been taken during deep inspiration is tantamount to air trapping (Fig. 12.4). Alternatively, asthma may present radiographically with a mix of air trapping and multifocal atelectasis or, less commonly, may mimic foreign body aspiration with unilateral hyperinflation (Figs. 12.5 and 12.6). At CT, manifestations of asthma may include bronchial wall thickening, luminal narrowing, regions of decreased lung parenchyma attenuation, and decreased vascularity during inspiration. Areas of air trapping may be present if the examination is taken during expiration (Fig. 12.7).
The National Heart, Lung, and Blood Institute defines emphysema as “abnormal permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of the alveolar walls, and without obvious fibrosis.” Centrilobular, panlobular, and paraseptal subtypes exist; however, centrilobular emphysema, typically seen in long-term cigarette smokers, is the most common form encountered in clinical practice. Chest radiographs are insensitive for detecting and grading emphysema; however, depression and flattening of the diaphragms, irregular radiolucency within the lungs caused by a heterogeneous distribution of parenchymal destruction, and increased retrosternal lucency on the lateral view may assist in making the diagnosis radiographically (Fig. 12.8). At CT, centrilobular emphysema typically manifests as numerous small foci of decreased attenuation without definable walls scattered in a background of relatively normal, homogeneous lung parenchyma. The lobular arteries may be visible in the center of the lucent regions, assisting in differentiating centrilobular emphysema from panlobular emphysema and cystic lung disease (Fig. 12.9). Exacerbation of chronic obstructive lung disease symptoms typically does not have a radiographic or CT correlate; however, patients may present with other complications including pneumothorax, pneumonia, and bulla infection (Figs. 12.10, 12.11, and 12.12).
Pneumonia
In the United States, pneumonia is among the leading causes of death and is very commonly evaluated and treated in the ED. Along with careful clinical and laboratory evaluation, radiography plays an important role in diagnosing, localizing, and characterizing pulmonary infections. Multiple pathogens can result in pulmonary infection, including bacteria, viruses, parasites, and fungi. The wide differential diagnosis for causative organisms can be narrowed by classifying pulmonary infections into clinical subsets such as community acquired, nosocomial, immunocompromised, pediatric, and so forth.
The most common pathogens found in community-acquired pneumonia are Streptococcus pneumoniae (40% of patients admitted to the hospital with pneumonia), Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila. Gram- negative organisms, especially Klebsiella pneumoniae, are also common causative organisms in persons at risk for aspiration, such as elderly patients and alcoholics.
Numerous viruses are implicated in lower respiratory tract infections of both immunocompetent and immunocompromised hosts and are commonly evaluated in the ED. Pulmonary viral infections can be classified into those occurring in immunocompromised patients and those occurring in patients with normal immune systems; however, there is considerable overlap in their radiographic appearance, and a specific imaging diagnosis is usually not possible. Most viral pneumonias in immunocompetent adults are the result of influenza types A and B infection, whereas immunocompromised patients are susceptible to a multitude of viruses such as parainfluenza, cytomegalovirus (CMV), herpes viruses, measles virus, and adenovirus.
The chest radiograph is typically the first line of imaging in the workup of a suspected lower respiratory infection. CT can be used for further characterization in the setting of complex pneumonia, suspected complication (such as pulmonary abscess or empyema), or to evaluate for an underlying disease process in the lung or mediastinum predisposing to pulmonary infection, such as an obstructing mass or lymphadenopathy (Fig. 12.13).
Pulmonary infection can be roughly classified into several radiologic patterns: lobar pneumonia, bronchopneumonia, and interstitial pneumonia. These patterns of infection tend to be associated with different organisms; however, significant overlap exists.
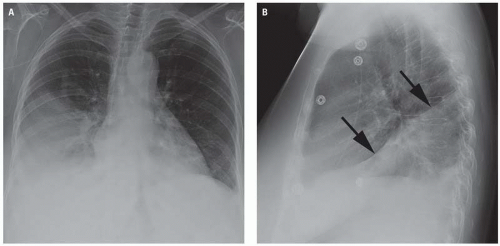
Lobar pneumonia typically appears as homogeneous consolidation involving predominantly a single lobe (Figs. 12.14, 12.15, 12.16, and 12.17). Multiple lobes may be involved; however, this is less common (Fig. 12.18). The lobar and segmental airways often remain patent within the region of consolidation, resulting in air bronchograms at chest radiography and CT.
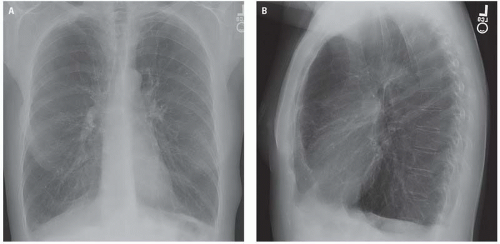
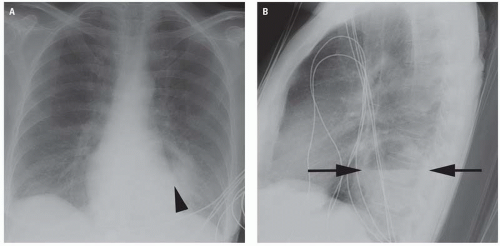
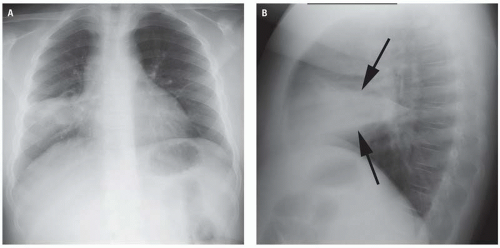 Figure 12.15. Right middle lobe pneumonia. Lobar pneumonia presenting with complete opacification of the right middle lobe on the frontal (A) and lateral (B) radiographs (arrows). |
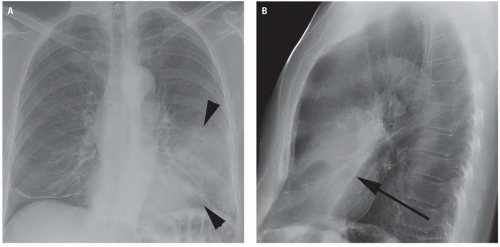
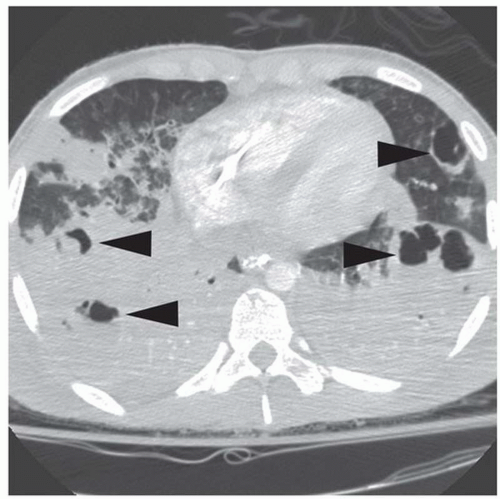
Bronchopneumonia is often the result of infection with Staphylococcus aureus or gram- negative bacteria. Patchy parenchymal consolidation, usually surrounding a segmental or subsegmental airway, is a common radiographic appearance (Fig. 12.19). The spectrum of radiologic severity of bacterial bronchopneumonia ranges from peribronchial thickening and poorly defined bronchovascular nodules (Figs. 12.20 and 12.21) to multi focal irregular regions of consolidation involving multiple lobes (Figs. 12.22, 12.23, and 12.24).
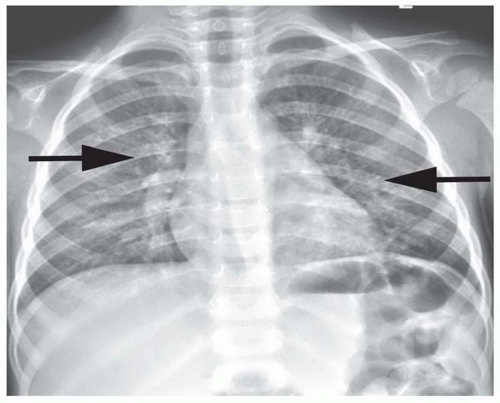
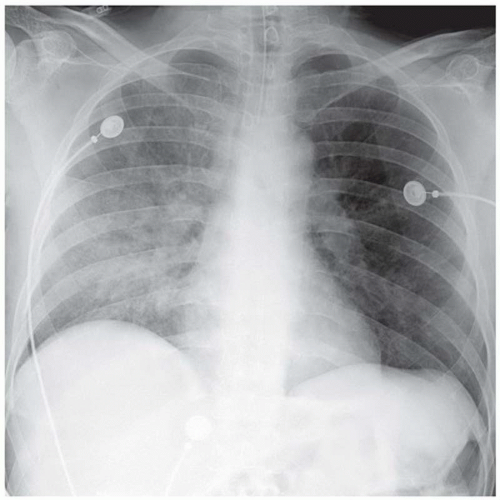
Infectious pneumonias involving predominantly the interstitium of the lung are commonly caused by viruses, M. pneumoniae, and Pneumocystis jiroveci. These organisms incite an interstitial cellular inflammatory infiltrate, resulting in the typical radiographic appearance of bilateral linear and reticular opacities (Figs. 12.25 and 12.26).
At CT, viral pulmonary infections typically manifest as multiple poorly defined nodules measuring up to 10 mm, patchy peribronchial ground-glass opacities, and airspace consolidation. Bronchiolar inflammation is also a common feature of viral pneumonia, resulting in air trapping and hyperinflation. Air trapping is most pronounced in pediatric patients, who also commonly demonstrate peribronchial infiltrates radiating from the hila.
Pulmonary Abscess
Pulmonary abscess occurs when a region of parenchymal infection undergoes tissue necrosis. The inciting organisms are most commonly mixed anaerobes, particularly in the setting of aspiration. Other causative organisms include S. aureus and Pseudomonas aeruginosa (Fig. 12.27). Multiple bilateral pulmonary abscesses may be seen secondary to septic emboli.
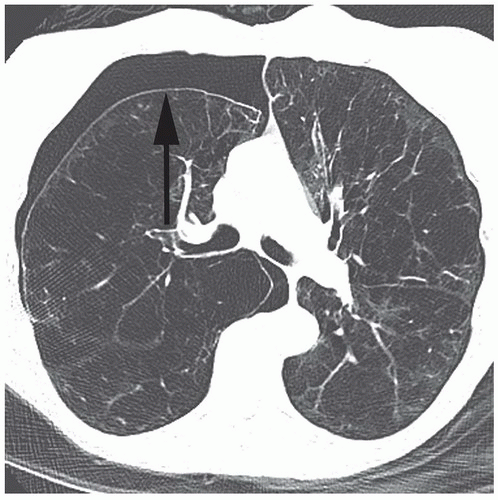
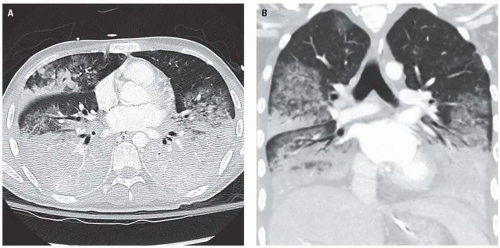
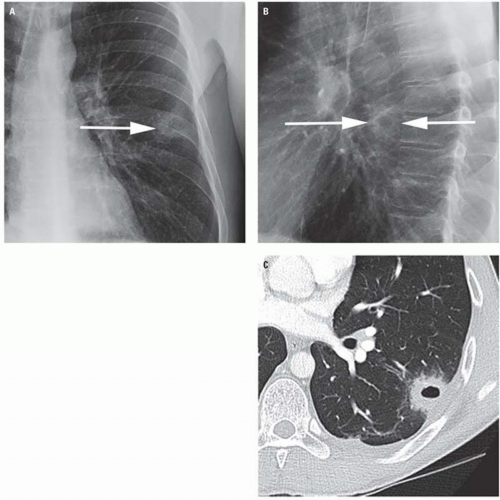
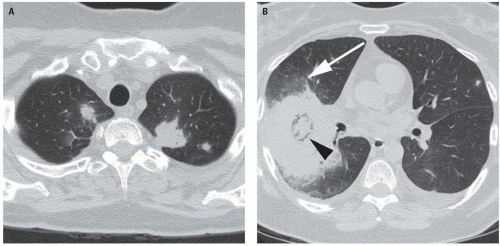
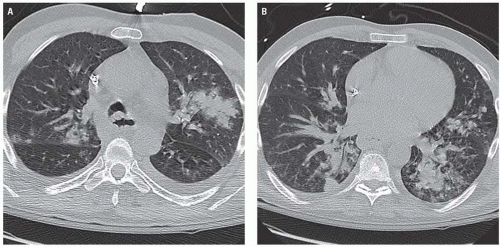 Figure 12.22. Severe bronchopneumonia. Axial CT images demonstrate patchy, irregular dense nodular opacities in the upper lobes (A) and in the lower lobes (B) along a bronchovascular distribution. The size and density of these nodules is greater than the fine “tree in bud” nodules seen in mild to moderate cases of bronchopneumonia (see Figs. 12.20 and 12.21). In the left upper lobe and in the medial lower lobes, the bronchovascular nodules are becoming confluent airspace consolidations in roughly segmental distributions. |
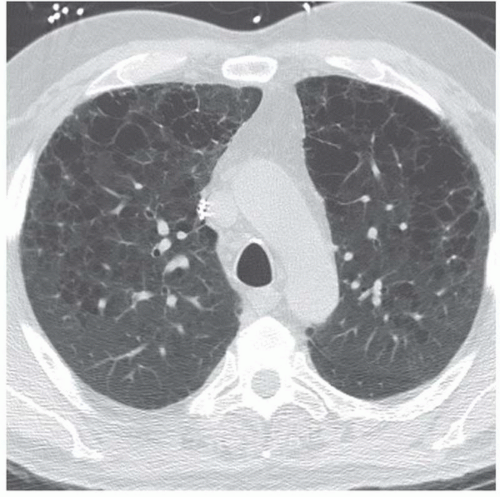
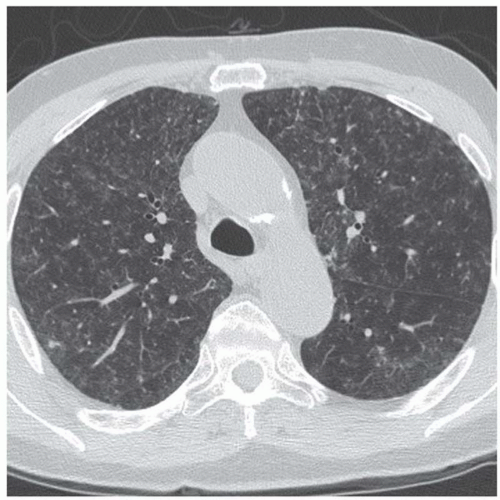 Figure 12.25. Varicella pneumonia. Ill-defined scattered small pulmonary nodules and mild peripheral interlobular septal thickening suggest a viral infection. |
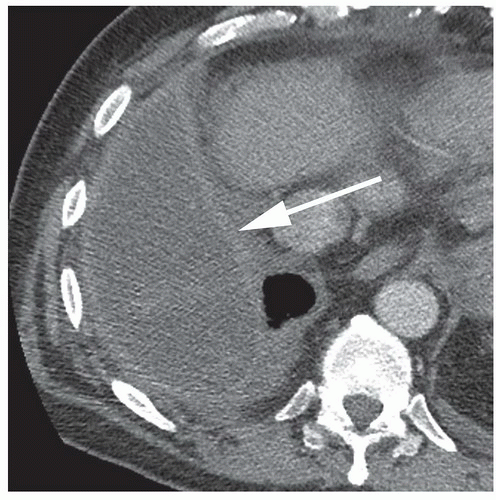
Differentiating an intrapulmonary abscess from an empyema can be difficult; however, the distinction is important for clinical management. The shape of a pulmonary abscess on radiographs and CT examinations tend to be round, whereas empyemas tend to appear ovoid or lenticular (Fig. 12.28). Pulmonary vessels may be observed to terminate abruptly at the margin of a pulmonary abscess while they tend to appear compressed or distorted along the margin of an empyema. The walls of a parenchymal abscess are typically, although not exclusively, more irregular and shaggy than those of an empyema (Fig. 12.29).
If a pulmonary abscess does not communicate with the bronchial tree, its radiographic appearance is that of a homogeneous density. Communication with the bronchus permits expulsion of necrotic material into the airways, resulting in cavitation and an air-fluid level.
The radiographic appearance of a cavitating pulmonary lesion typically does not allow for reliable differentiation between cavities caused by common bacterial pathogens, TB, vasculitis, or cavitating neoplasm. Although in many instances, the clinical findings, the location of the lesion, and the imaging appearance may suggest the etiologic agent, the correct diagnosis can be established only
by appropriate clinical evaluation and laboratory studies (Fig. 12.30).
by appropriate clinical evaluation and laboratory studies (Fig. 12.30).
Immunocompromised Patients
Immune compromise has multiple etiologies including HIV infection, solid organ transplantation, bone marrow transplantation, bone marrow suppression or replacement, and nonspecific reductions in immunity such as poorly controlled diabetes, alcoholism, and underlying malignancy. The various forms of iatrogenic and infectious immunosuppression are associated with unique time courses of susceptibility and unique opportunistic infections, and a comprehensive discussion of this complex topic is beyond the scope of this text.
The radiologic appearance of pulmonary infection in an immunocompromised patient is often nonspecific; however, there are three main radiologic patterns of pulmonary infection seen in immunocompromised patients: focal consolidation (patchy, segmental, or lobar), nodules (with or without cavitation), and diffuse or interstitial opacities.
A focal wedge-shaped opacity in an immunocompromised patient most likely represents a bacterial infection with a community-acquired pathogen. Infection with Mycobacterium tuberculosis (see later
discussion) should be considered in the setting of severely compromised immunity, particularly in advanced HIV infection.
discussion) should be considered in the setting of severely compromised immunity, particularly in advanced HIV infection.
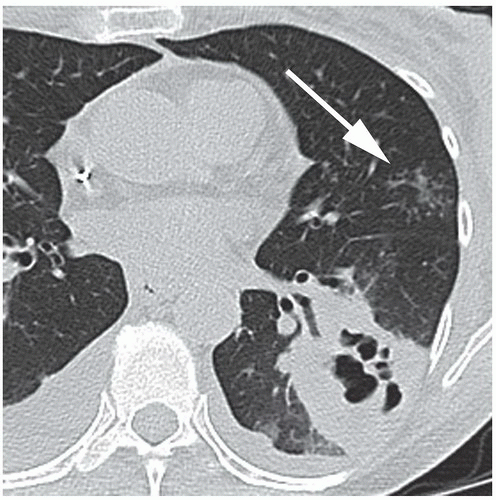
Pulmonary nodules (single or multiple) are commonly due to septic emboli, fungal infection (particularly Cryptococcus neoforman and Aspergillus fumigates), Nocardia, or mycobacteria (Fig. 12.31). Cavitation of nodules or associated parenchymal consolidation is concerning for angioinvasive aspergillosis or septic emboli. Cavitary lesions secondary to invasive Aspergillus may demonstrate a crescent of air between the infarcted, necrotic lung centrally and the rim of surrounding viable lung tissue (Fig. 12.32).
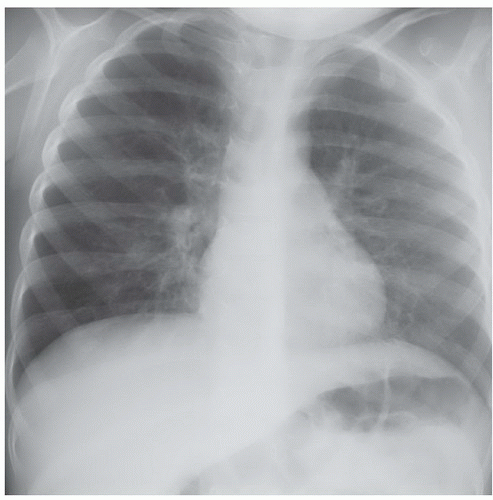
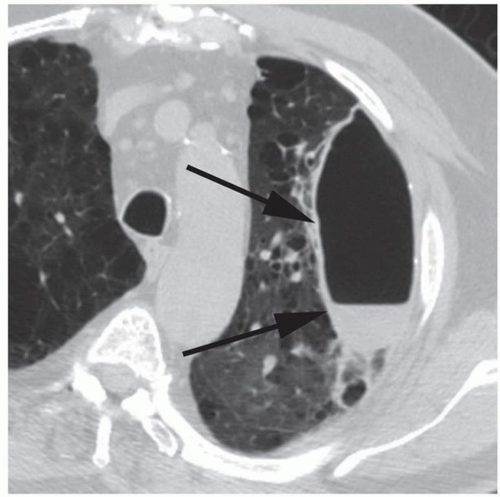
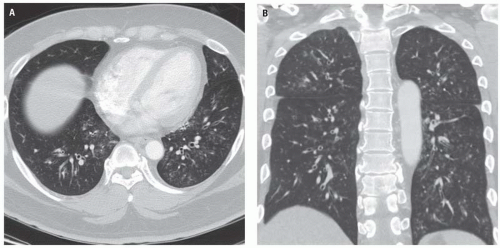
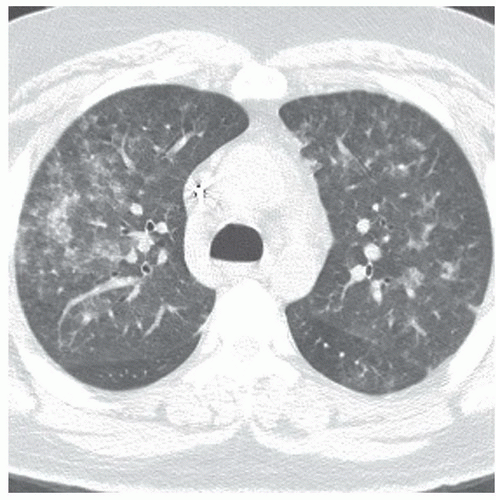
Diffuse pulmonary opacities in an immunocompromised host are often secondary to viral infection such as CMV and varicella zoster or to the fungus P. jiroveci (particularly in advanced HIV infection). CMV pneumonia often manifests on chest radiograph as diffuse, bilateral reticular, and ground-glass opacities; however, the CXR may be normal despite significant clinical symptoms. CT may demonstrate multifocal ground-glass opacities, centrilobular nodules, and regions
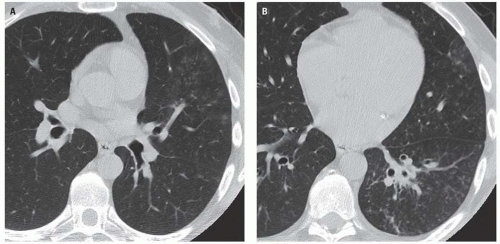
of focal consolidation (Fig. 12.33). P. jiroveci infection manifests as bilateral perihilar ground-glass opacities and interstitial prominence during the early course of the disease (Fig. 12.34). CT demonstrates multifocal ground-glass opacities in a mid and upper lung distribution, often with mild interlobular septal thickening (Fig. 12.35). The infection may progress to more focal parenchymal consolidation (Fig. 12.36). Multiple small pneumatoceles may develop, predisposing the patient to develop a pneumothorax (Fig. 12.37).
of focal consolidation (Fig. 12.33). P. jiroveci infection manifests as bilateral perihilar ground-glass opacities and interstitial prominence during the early course of the disease (Fig. 12.34). CT demonstrates multifocal ground-glass opacities in a mid and upper lung distribution, often with mild interlobular septal thickening (Fig. 12.35). The infection may progress to more focal parenchymal consolidation (Fig. 12.36). Multiple small pneumatoceles may develop, predisposing the patient to develop a pneumothorax (Fig. 12.37).
Tuberculosis
The emergency radiologist can play a crucial role in diagnosing a patient with active TB. It is therefore important for the radiologist to have a high level of awareness of the various imaging features of this disease and alert the emergency physician to the possibility of active TB so that proper public health precautions can be instituted until the diagnosis is excluded or established. The radiologic presentation of TB depends on patient factors including age, immune status, and prior exposure.
 Figure 12.33. Cytomegalovirus (CMV) pneumonia. CT demonstrates multifocal and confluent ground-glass opacities, interlobular septal thickening, and regions of developing focal consolidation. |
 Figure 12.34. Diffuse ground-glass and fine reticular opacities represent P. jiroveci infection in a patient with AIDS. |
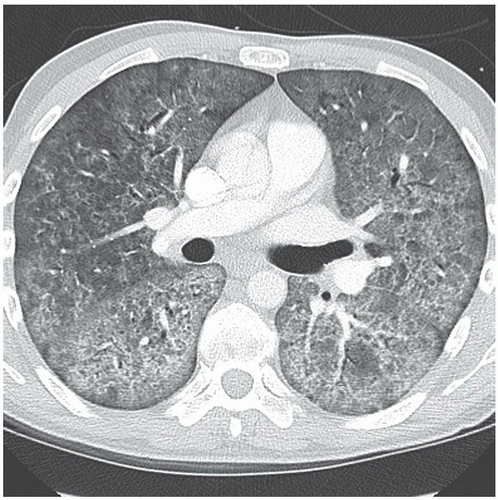 Figure 12.35. Severe infection with P. jiroveci in a patient with advanced HIV disease. There are extensive ground-glass opacities and interlobular septal thickening. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree