Chapter 65 A systematic approach to evaluation of the chest film consists of an assessment of heart size, shape, and position; pulmonary vasculature; the airway and mediastinum; visceral situs; and skeletal abnormalities. Applying such an approach often results in a diagnosis of a cardiovascular disease category such as a shunt or a right- or left-sided obstructive lesion, which in turn leads to a differential diagnosis and the identification of the likely etiology of nonspecific clinical findings, such as congestive heart failure or cyanosis (Box 65-1). As in all medical imaging, attention to detail is necessary to optimize the examination and its interpretation. Proper exposure, centering, collimation, patient positioning, and inspiration are necessary (e-Fig. 65-1). e-Figure 65-1 A normal chest examination in an infant. One of the challenges in evaluating the chest radiograph of younger children is their variable anatomy and physiology. For example, the thymus is variable in size and position and may mimic cardiomegaly, abnormally positioned vessels, pericardial fluid, or a mediastinal mass (e-Fig. 65-2). e-Figure 65-2 A normal chest examination in an infant. Newborn infants have physiologic pulmonary hypertension, and as a result, large shunt lesions do not appear until the pulmonary vascular resistance falls, which usually occurs by 4 to 6 weeks (Fig. 65-3). Similarly, newborn infants may not show the expected changes of severe pulmonary stenosis or atresia if the ductus arteriosus is patent. Figure 65-3 Complete transposition of the great arteries in a neonate. The physiology of small airways in infants and young children (up to approximately 2 years of age) results in unique manifestations of pulmonary edema. Specifically, infants show hyperinflation as a response to interstitial edema, as would happen in the presence of airway inflammation with bronchiolitis (Figs. 65-3 and 65-4). Figure 65-4 Total anomalous pulmonary venous return with obstruction in an infant. The size of the heart can be difficult to assess in the frontal projection of infants and young children because of the presence of the relatively large thymus and poor inspiration (see e-Figs. 65-1 and 65-2
Chest Radiography in Pediatric Cardiovascular Disease
Technique
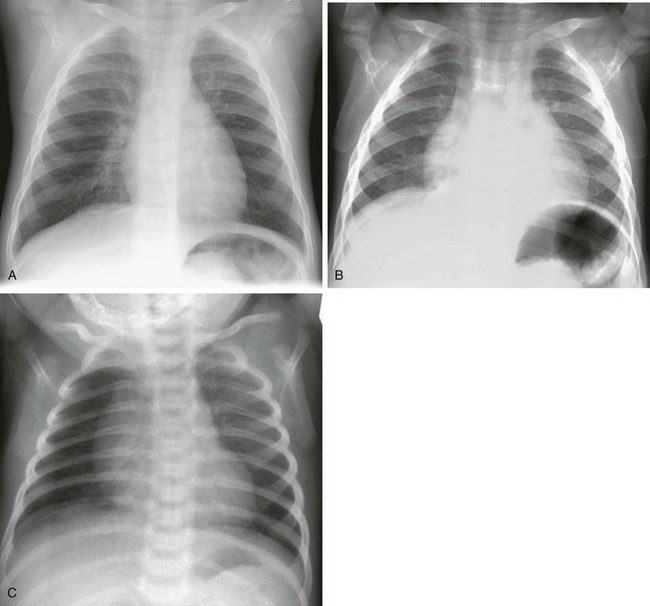
Frontal radiographs in inspiration (A) and expiration (B) show the profound impact of an expiratory film on the appearance of the heart and lungs. In another example (C), a lucent right lung reflects patient rotation to the right rather than asymmetrical pulmonary blood flow.
Systematic Interpretation
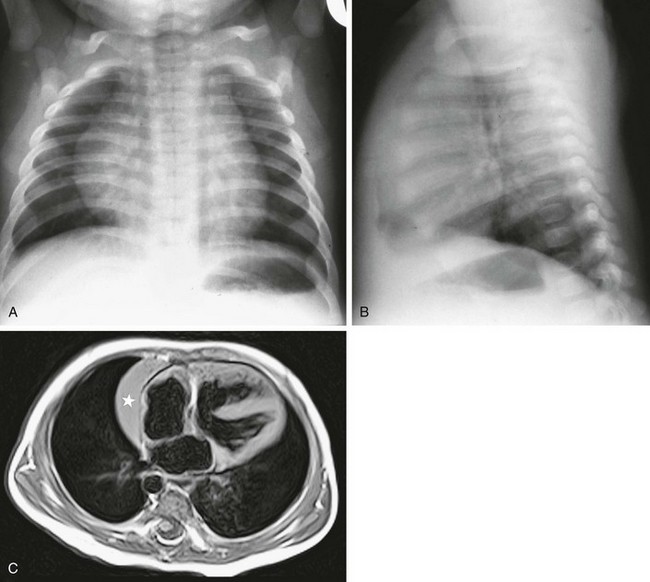
A frontal chest radiograph (A) shows a large cardiomediastinal silhouette, which on lateral view (B) reflects a normal heart and a large retrosternal thymus. In another child, a T1-weighted axial magnetic resonance image of the chest (C) shows the right lobe of the thymus (star) beside the right atrium. Note also the ventricular septal defect.
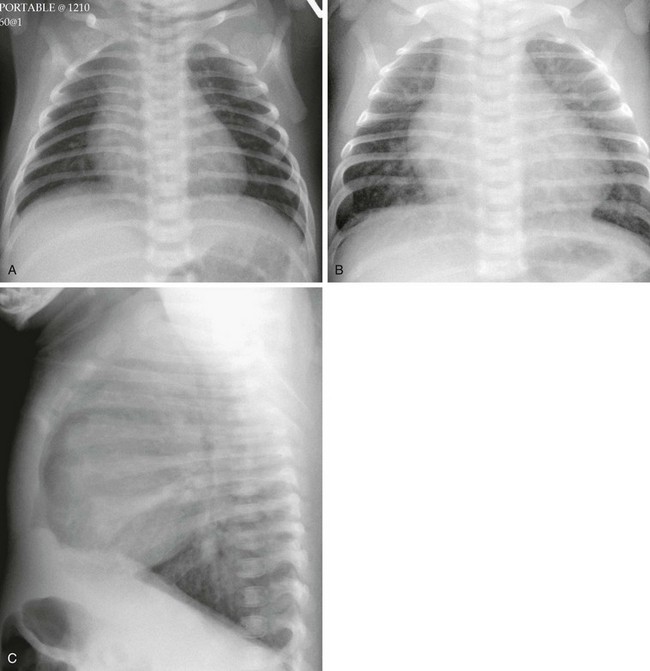
A frontal radiograph (A) on day 1 of life shows a heart that is within normal limits in size and shows normal pulmonary vascularity. The same child at 7 weeks of age (B and C) has an enlarged heart and increased pulmonary vascularity. Volume loading of the heart and pulmonary circulation has occurred as pulmonary vascular resistance has dropped.
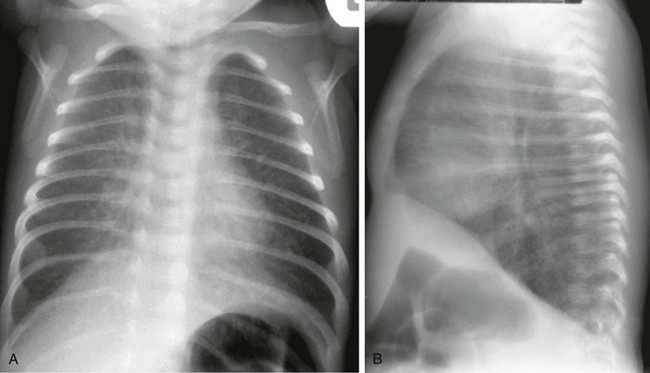
Frontal (A) and lateral (B) radiographs show normal heart size, hyperinflation, and interstitial thickening consistent with pulmonary edema.
Heart Size
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Chest Radiography in Pediatric Cardiovascular Disease





