Fig. 1
Diagram of a lateral view of the chest showing the three mediastinal compartments and the anatomic structures they contain. A Anterior compartment, M Medium compartment, and P Posterior compartment (Reprinted with permission from Moënne and Ortega 2012)
2.1.1 Thymus
Normal mediastinum is particularly prominent in small children due to the characteristic prominent thymus at this age.
The thymus is usually visible in chest radiographs of children under 3 years of age, and occasionally beyond that age. Size and growth pattern of the thymus has been matter of many studies. Classically, it has been considered that the thymus increases in size until puberty, and then involutes progressively. It has also been postulated that its prominence in small children is more related to the smaller body mass of children, rather than to a real absolute large volume. According to a study performed by Steinmann the thymus attains its maximum size during the first few months of life and does not grow any larger beyond that age (Nasseri and Eftekhari 2010).
Normal thymus has soft contours and does not compress adjacent structures. In chest radiographs it has a similar density to the adjacent heart and vascular structures. As a result, delineation of the borders of these structures is difficult and diagnostic errors can occur if the radiologic characteristics of the thymus are not considered.
Three classical radiological signs have been described regarding the radiologic representation of the thymus: (Enríquez et al. 2009; Nasseri and Eftekhari 2010).
Wave sign: wavy contour of the thymus caused by indentation of its soft tissue by the anterior costal arches (Fig. 2).

Fig. 2
The wave sign: note the wavy contour of the thymus on the left side, caused by indentation of its soft tissue by the anterior costal arches
Sail sign: triangular and usually slightly convex appearance of the right lobe of the thymus delineated inferiorly by the minor fissure of the right lung (Fig. 3). It is present in approximately 5 % of children and is seen both in frontal and lateral views (Nasseri and Eftekhari 2010).

Fig. 3
The sail sign: the right lobe of the thymus has a triangular shape with its inferior border limited by the horizontal fissure of the right lung
Cardiothymic incisure: small indentation seen in frontal views in one or both sides of the mediastinum (Fig. 4).

Fig. 4
The cardiothymic incisure: the arrow shows a small indentation where the thymus contacts the cardiac border
In patients under stress (acute respiratory illness, surgery, steroid therapy, radiotherapy and others), significant decrease in the size of the thymus can be seen, as well as changes in its configuration. Once stress is over, the thymus can grow up to 50 % more of its original size. This “thymic rebound” occurs mainly in children, though it can also be seen in adults (Nasseri and Eftekhari 2010).
It is important to remember the role of ultrasound (US) in characterizing normal thymus parenchyma. In cases of uncertain radiological images, US, using the anterior chest wall as acoustic window, is extremely helpful to identify the thymus and define its participation in mediastinal size and shape (Han et al. 2001).
2.1.2 Heart
Changes in the size and configuration of the heart can also affect the radiological representation of the mediastinum. When analyzing the heart the position in which the child was examined must be considered. In supine position the heart appears more prominent than in standing position. It is important to remember that a supine frontal view is routinely used in infants, whereas toddlers and older children are generally examined in standing position (Enríquez et al. 2009). Lateral views are useful to evaluate posterior cardiac enlargement and, in absence of a large thymus, right ventricular size by noting the area of contact of the heart with the sternum (Fig. 5a, b).
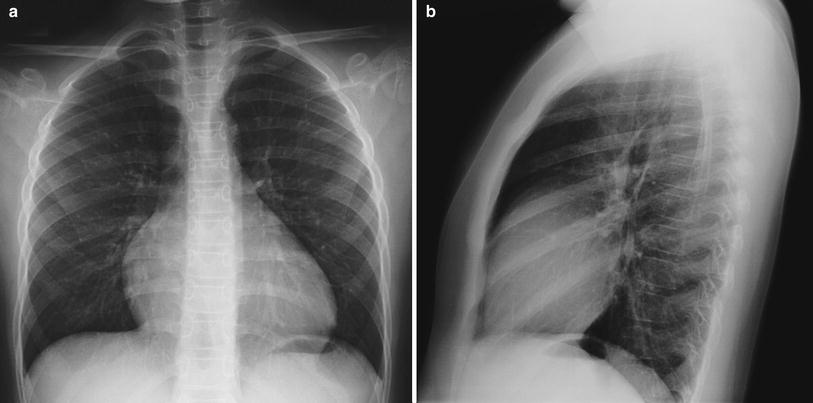
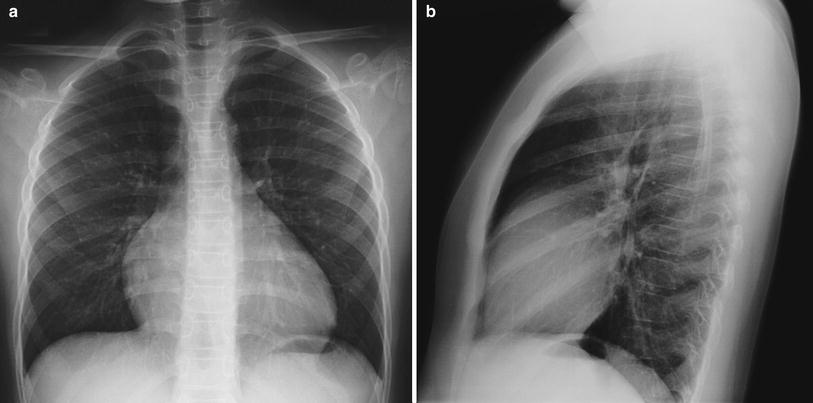
Fig. 5
Frontal chest radiograph of a prominent heart (a). Lateral view shows wide contact of the anterior border of the heart with the sternum, indicating right ventricular enlargement (b)
Frontal views obtained in expiratory phase are a frequent cause of wrong diagnosis of mediastinum widening and heart enlargement (Fig. 6) (Enríquez et al. 2009).


Fig. 6
Frontal under-inspired chest radiograph of a normal child. Note the apparent widening of the mediastinum and enlargement of the heart. The radiograph was repeated with adequate degree of inspiration and both the mediastinum and the heart showed a normal appearance
2.1.3 Trachea
The trachea is represented in chest radiographs throughout all its extension, especially when digital technique is used. A careful analysis of the tracheal air column has to be done, both in frontal and lateral views. If a tracheal tube is present, proper position must be confirmed.
In the frontal view the proximal subglottic trachea shows bilateral symmetric convexities, a finding described as “shouldering” of the air column (Fig. 7). Distal to this the diameter of the trachea remains constant and its walls are parallel, except where the aortic arch causes a localized indentation. Occasionally in asymptomatic children an anomalous innominate artery or, less frequently, the common carotid artery can produce an anterior indentation of the trachea at the level of the sternal manubrium. This finding is only seen in small children, in whom there is proportionately less space in the upper mediastinum and therefore a greater possibility that these arteries indent the trachea. A frequent associated finding in these cases is tracheomalacia, believed to be the cause of symptoms, such as stridor and respiratory distress, present in some of these children (Swischuk 1971).


Fig. 7
Frontal view of the proximal trachea. Note the bilateral symmetric convexities of the normal subglottic trachea, known as “tracheal shouldering”
2.2 Pitfalls and Abnormalities
Due to the greater flexibility and relatively larger size of the trachea it is frequent to see in children less than 5 years of age lateral tracheal deviations and even angulations. This finding is more pronounced with cervical flexion and in under-inspired images (Fig. 8) (Moënne and Ortega 2012). This physiologic tracheal deviation is usually toward the right, opposite direction to the aortic arch, which “anchors” the trachea avoiding lateral deviation toward its side.
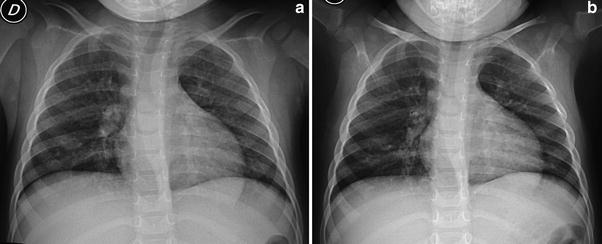
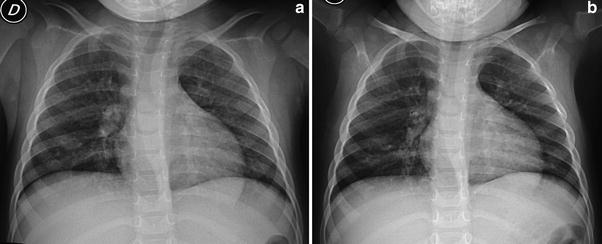
Fig. 8
Under-inspired (a) and well-inspired frontal chest radiographs (b) of a 2-year-old boy. Note the right-sided lateral deviation of the trachea that is completely straight in the well-inspired radiograph
Any anterior displacement of the intrathoracic trachea must be considered abnormal (Fig. 9), as well as any lateral deviation in children over 5 years of age (Chang et al. 1970).
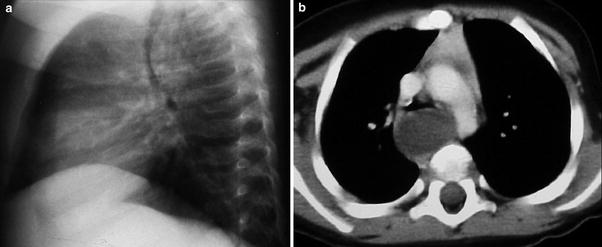
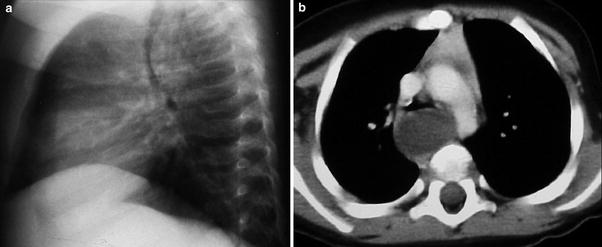
Fig. 9
Lateral chest radiography showing anterior deviation of the trachea (a) secondary to a bronchogenic cyst, demonstrated on CT (b)
Recognizing “physiological” tracheal deviations is important to prevent performing unnecessary studies in healthy children.
When tracheal inflammation is present, underlying edema causes narrowing of the subglottic trachea with loss of the normal tracheal “shouldering” (Fig. 10). The inverted V configuration of the trachea under these circumstances is called the steeple sign. It is a non-specific sign most frequently cause by croup or laryngotracheobronchitis. Even if the diagnosis of croup is clinical, radiographs may be requested to exclude other causes of stridor, such as foreign body aspiration, an esophageal foreign body, congenital subglottic stenosis, epiglottitis or a subglottic hemangioma. In these cases the steeple sign helps to define croup as the cause the symptoms (Salour 2000).
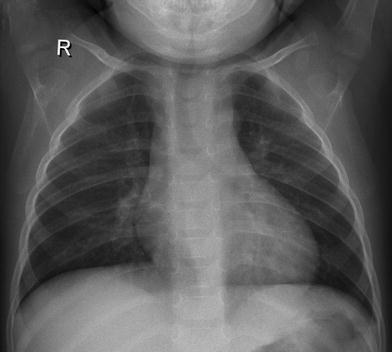
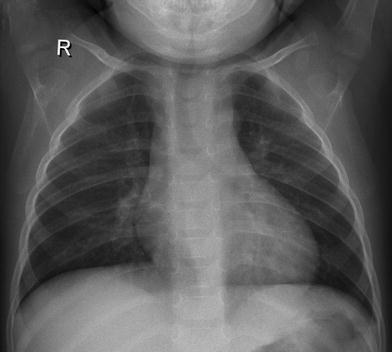
Fig. 10
The steeple sign. Note the inverted V shape of the subglottic trachea representing underlying inflammation and edema in a child with croup. The normal “shouldering” of the trachea at this level is lost
Any tracheal indentation or narrowing, other than those previously mentioned has to be considered abnormal. Diffuse narrowing is usually congenital, due to complete cartilaginous tracheal rings (Fig. 11a, b) Focal narrowing is more frequently a complication of tracheal intubation. Tracheal compressions caused by vascular structures can be detected in radiographs, however CT or magnetic resonance (MR) imaging is mandatory to define the exact vascular anatomy and its relation to the airway. Tracheomalacia, defined as the dynamic collapse of the trachea during the expiratory phase, can be isolated or associated to vascular rings or tracheoesophageal fistula. Stridor and occasionally dyspnea are the clinical manifestations.
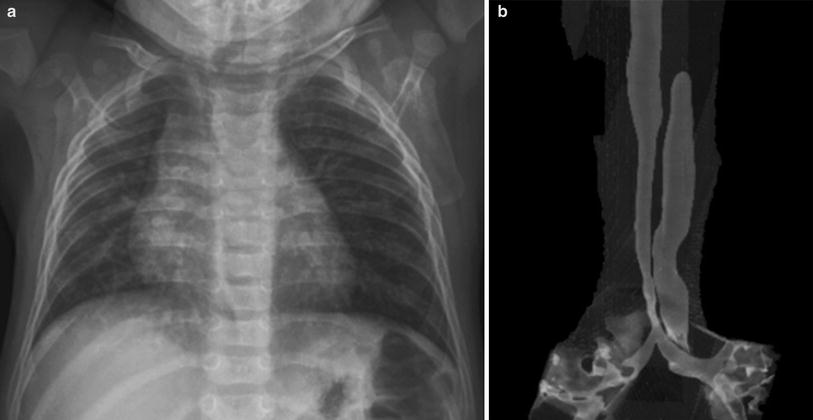
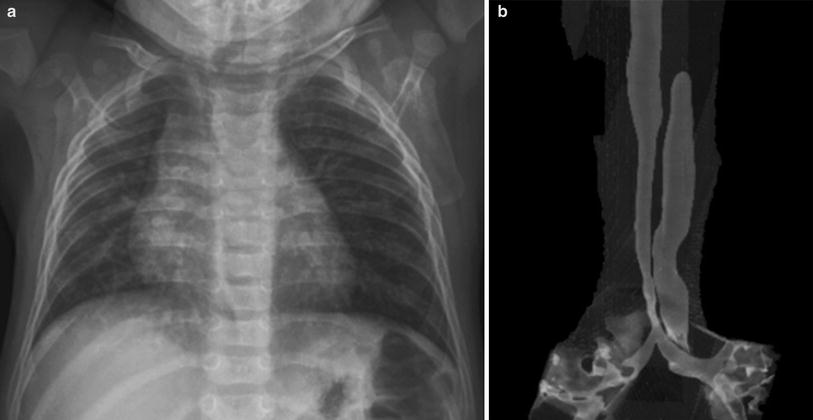
Fig. 11
Frontal chest radiograph (a) and CT coronal volume rendering image of the trachea (b) in a child with type II pulmonary sling. Note the low T-shaped carina and the long segment narrowing of the intrathoracic trachea
Masses, either congenital or tumoral, can originate in any mediastinal compartment. Chest radiographs can show compression or displacement of adjacent structures (Fig. 12), however, their characterization requires imaging with CT or MRI (Zylak et al. 2000).


Fig. 12
A huge anterior mediastinal mass produces lateral deviation of the heart and trachea. CT showed a mediastinal teratoma
If a chest radiograph shows signs of mass effect over mediastinal structures, CT or MR studies are mandatory to complete imaging investigation.
Pneumomediastinum can result from a variety of causes that may be either intra or extrathoracic, and that vary with age (Zylak et al. 2000). While occasionally it can be secondary to intrathoracic spread of air from the cervical region or from the abdomen, most cases are secondary to alveolar over distension and rupture due to high intra-alveolar pressure. (Chalumeau et al. 2001). A variety of conditions have been described in relation to pneumomediastinum in children, including trauma, medical illnesses, and iatrogenic. Although in some children it may occur spontaneously, a trigger can be found in up to 70–90 % of cases; the most frequent are asthma, vomiting of any cause, situations involving repetitive Valsalva maneuver, and intense sport activities. In newborns respiratory effort can be the sole cause of pneumomediastinum.
Radiographic signs of pneumomediastinum reflect the free air dissecting different anatomic mediastinal structures (Zylak et al. 2000). The main radiological signs in children are:
Retrosternal and precardiac hyperlucency: collection of air in the anterior mediastinum compartment (Fig. 13).
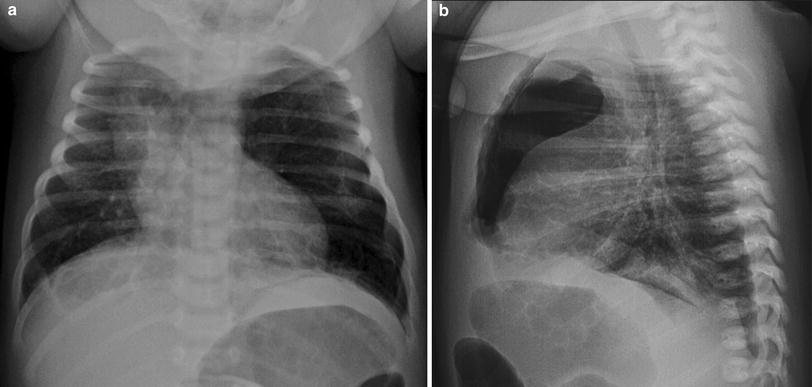
Fig. 13
Pneumomediastinum: a large collection of air is seen in the retrosternal and pre cardiac region of the anterior mediastinum, in frontal (a) and lateral (b) chest views. Note elevation of the thymus lobes
Periaortic and peritracheal lucent streaks: dissection of air into the mediastinum or the mediastinal recesses (Fig. 14).
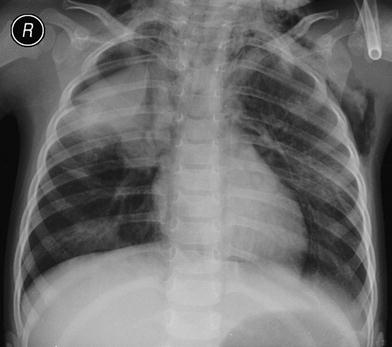
Fig. 14
Frontal chest radiograph in a child with pneumomediastinum and right pneumothorax. Note streaks of air dissecting the upper mediastinal structures. The medial pleural line is also seen as well as subcutaneous emphysema
Angel–wing sign, or spinnaker sail sign: elevation and lateralization of the lobes of the thymus by air in the mediastinum (Fig. 15).
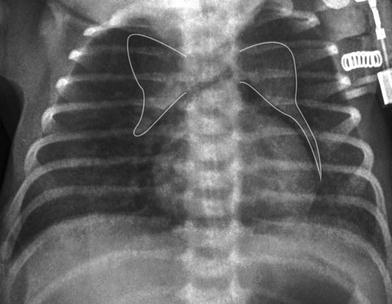
Fig. 15
The “angel sign” elevation and lateralization of both thymic lobes that are separated by air from the adjacent mediastinal structures
Ring around the artery sign: radiolucent line surrounding the right pulmonary artery, seen on the lateral view (Fig. 16).

Fig. 16
Lateral chest radiograph showing the “ring around the artery sign” in a 15-year-old girl with spontaneous pneumomediastinum. Note the radiolucent line surrounding the right pulmonary artery (arrow)
Continuous diaphragm sign: interposition of air between pericardium and diaphragm making visible the central part of the diaphragm in continuity with the diaphragmatic domes (Fig. 17).

Fig. 17
Frontal chest radiograph of an infant with pneumomediastinum showing the “continuous diaphragm sign”
Indirect signs of pneumomediastinum are subcutaneous emphysema, usually present in infants and older children but not in newborns, and pneumopericardium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








