Introduction
The impact of the effects of the neurological damage on the individual and those related to him/her can, however, be minimized. With good management of all aspects of paralysis from the time of the injury, many initially paralyzed patients can make significant neurological recovery and walk again. With ongoing expert monitoring, care, and support, those who do not recover are able to lead fulfilling and fruitful lives, as well as contribute to society.
A thorough assessment of the patient, including full neurological examination, appropriate radiological investigations, and accurate documentation of the findings, is of paramount importance in initiating good management and in monitoring progress.
As spinal cord injury (SCI) affects the physiology of almost all systems of the body, any assessment should encompass more than spinal column or spinal cord functions.
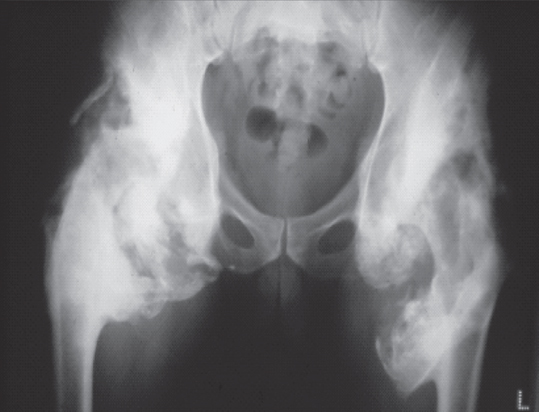
Fig. 1.1 Heterotrophic ossifications in a tetraplegic patient. They can be detected early with an ultrasound scan. Early treatment with biphosphonates and anti-inflammatory medication minimizes the severity of the outcome.
Effects of Spinal Cord Injury
A spinal cord injury results in a generalized physiological impairment that involves most systems of the body either directly or indirectly.
The physiological impairment and the consequent multi-system malfunction caused by SCI are dynamic in nature throughout the patient’s life. The rate of change in the functioning of the various systems of the body is more rapid, though predictable, in the early stages (first 4-6 months) following injury.
Unpredictable changes in functions will inevitably occur throughout the patient’s life, when the condition is likely to be perceived by most clinicians as being stable. The importance of frequent reassessments and repeated documentation at all stages following injury cannot be overemphasized. The only difference in the requirement for monitoring between the acute stage and the lifelong follow-up is the frequency of the monitoring.
In the absence of complete neurological sparing or full neurological recovery, the majority of patients with spinal cord injuries have sensory impairment or sensory loss below the level of their injury. Associated injuries and/or pathological complications can, therefore, develop in the absence of the conventional symptoms and signs, resulting in delay of diagnosis often with unpleasant consequences (Fig. 1.1).
When a complication develops, the interruption of the higher coordinating and moderating functions of the brain at the site of the spinal cord injury usually results in multiple and/or cascading intersystem effects, which are rarely seen in other conditions and which are seldom easy to manage. For example, an anal fissure, while painless, may nevertheless cause excess spasticity, which in turn may cause a fall and fracture of a long bone. Alternatively, excess spasticity involving the pelvic floor muscles may result in urinary retention, autonomic dysreflexia, and possibly a cerebrovascular accident.
The multi-system malfunction caused by the spinal cord injury is not only a source of multiple disabilities, but also a potential source of a wide variety and range of complications. What is perhaps not widely appreciated is that almost all complications following spinal cord injury are preventable.
Fortunately, the incidence of spinal cord injuries is the lowest of all major traumas. However, a combination of low incidence and high complexity necessitates an even more thorough and time-consuming systematic assessment than usual. The management of such patients, once they are stable for transfer, is therefore easier and safer to conduct in spinal injuries centers. These centers are usually equipped with the infrastructure of both the required expertise of adequately trained multidisciplinary teams and the necessary equipment. They are geared to provide comprehensive management, while giving equal attention to details that are necessary to ensure safety, comfort, and a good outcome for the patient, as well as medico-legal protection for the clinician and the institution.
Clinical and Radiological Assessment in the Acute Stage
Missed Spinal injuries
Missed spinal injuries are regularly reported in the literature.1–4 It is probable that in a significant number of patients the diagnosis of a spinal cord injury is delayed without being reported. Delaying diagnosis can result in increased neurological impairment.4,5 This is likely to result in more paresis or paralysis, increased disability, more disturbance of function of the various systems of the body and more complications. It is indeed a disaster to miss a spinal fracture or delay its diagnosis. It can easily be alleged that the neurological impairment has been caused or at best aggravated by failure to diagnose the fracture promptly. A delay in diagnosis is not unusually perceived by some patients and lawyers as having led to delays in ensuring appropriate precautions and adequate treatment. It is therefore paramount that no effort is spared in making as accurate a diagnosis in the accident and emergency department as possible. A high level of suspicion is a major prerequisite to early diagnosis in patients presenting following major trauma. The knowledge that a small group of patients with certain bone conditions, for example ankylosing spondylitis, osteoporosis, osteogenesis imperfecta, is more vulnerable to spinal injuries following minor trauma is at least equally important.
A thorough assessment of the patient including a full neurological examination together with appropriate radiological investigations, and accurate documentation of the findings are of paramount importance for initiating good management and monitoring progress.
Clinical Diagnosis of SCI in the Conscious Patient
A conscious alert patient, who is able to communicate and has symptoms of neck or back pain, rigidity, or tenderness in the spine following trauma is likely to have sustained a spinal column injury.6 There are, however, some rare exceptions. Pain may not be a feature in elderly patients with pure cervical ligamentous injuries without major vertebral damage in spondylotic spines. The author has personally witnessed this in a small number of patients, some of whom successfully pursued litigation. Extreme pain from other associated injuries may also mask pain from a spinal fracture with consequences to the timely diagnosis of a spinal injury.7 Neck pain, loss of consciousness following injury (regardless of duration), and/or neurological deficit are clinical predictors of unstable cervical spinal injuries requiring immediate radiological investigation of the cervical spine.8,9 The clinical diagnosis of a spinal cord injury in the conscious patient, who has no associated major injuries can be made without difficulty. Loss or impairment of motor power, sensation, and reflexes are indicative (individually or in combination) of damage to the spinal cord or the cauda equina depending on the level of impairment. Extra care should be taken in patients with L2 injuries and below. A traumatic injury below the level of S1 without injury to the cauda equina is rare. If present, it can, however, present with normal tendon reflexes and unimpaired motor power.
It is essential to determine at the earliest stage possible both the level and the density of the neural tissue damage.
The level of the injury is defined by the last normal dermatome and myotome. It is now internationally accepted by all experts in the field that the dermatomal and myotomal distributions may be abnormal for three segments below that level. In other words both sensation and motor power could be present but impaired in three segmental distributions below the last normal segment. For example if the last normal sensation is at the dermatomal distribution of C5 but there is hypoesthesia or analgesia in the dermatomal distribution of C6, C7, and C8 the level of the injury should be defined as C5. The impairment of sensation in the dermatomal distribution of C6, C7, and C8 can be explained by the logical assumption that the spinal cord segments C6, C7, and C8 are not completely damaged. Damage of these segments is incomplete; hence these segments represent the “zone of partial preservation.”
The density of the deficit from the damaged area in the spinal cord is defined by the presence or absence of sparing of sensation with or without sparing of motor power below the zone of partial preservation.
Absence of motor power including voluntary contraction of the anal sphincter and loss of sensation including loss of anal sensation below the zone of partial preservation are usually indicative of a clinically complete cord injury at the time of the examination. It is important, however, to appreciate that not all clinically complete injuries in the early hours or days following SCI remain clinically complete.10,11 Spinal shock can also mimic an initially complete injury following which significant recovery can occur.
The presence of sensation, however patchy or impaired, below the level of the zone of partial preservation is indicative of some anatomical sparing of sensory tracts and possibly also of corticospinal tracts which may be dormant in function at the time of the examination. Sensory sparing limited to the anal canal without motor sparing below the zone of partial preservation is also indicative of an incomplete SCI. A number of such patients can subsequently recover significantly. A rectal examination to elicit sensation in the S5 dermatome and voluntary/involuntary contraction of the anal sphincter is therefore an essential component of the neurological examination of patients diagnosed or suspected to have sustained an SCI.
An accurate and thorough neurological examination at an early stage following the injury is paramount for monitoring purposes and for prognosis.
A repeated accurate neurological assessment, with thorough documentation initially at frequent intervals (3-4 hours), is not only essential for the adequate clinical management of any neurological deterioration, it would also help resolve some of the controversies around the indications and effectiveness of the various methods of management of the SCI (conservative versus surgical decompression and/or stabilization).
It is not advisable to rely entirely on the neurological and general examination carried out in the accident and emergency department to make a definitive diagnosis of the density of the spinal cord injury. The patient’s attention can, at this early stage, be distracted by anxiety, confusion, and pain. These may also limit performance of motor functions and responses to sensory testing. It is therefore possible that the neurological examination in the first few hours may not be very accurate with a tendency to underscore the motor power and underscore or overscore the sensory sparing. The documentation of the state of consciousness and cooperation of the patient during the neurological examination is understandably essential.
Clinical Diagnosis in the Semiconscious or Unconscious Patient
Unconscious or semiconscious patients with head injuries and the intoxicated patient present particular problems to the clinician which can result in delays of the diagnosis of a spinal injury.12 It is therefore, in my opinion, imperative that such patients, following major trauma, are nursed as having sustained a spinal injury until otherwise proven clinically and radiologically when the patient becomes alert.
In such patients a clear entry should be made in the medical records that the patient’s neurological assessment could not be made because of the poor level of consciousness. This fact should also be communicated verbally to the nursing staff looking after the patient.
I would strongly advise that a written instruction
“NOT TO SIT THE PATIENT UP IN BED OR OUT OF BED PRIOR TO THE EXCLUSION OF A SPINAL INJURY CLINICALLY AND RADIOLOGICALLY AND UNTIL THE PATIENT REGAINS CONSCIOUSNESS” is clearly documented in the medical records and communicated verbally to the nursing staff.
This simple, logical, and easy documentation can result in the prevention of paralysis or further neurological deterioration as well as the prevention of litigation against the clinician and/or the institution.
The general examination of the unconscious patient can also yield a number of clinical signs that, in combination, can increase the clinician’s level of suspicion regarding the presence of a neurological impairment of spinal cord origin.
During a systematic examination of the patient the following signs can be strongly suggestive of a cervical spinal cord injury:
- Facial or scalp lacerations;
- Miosis of one or both pupil(s);
- Bruising or swelling of the neck;
- Absence of chest expansion during inspiration associated with increasing abdominal girth and retraction of intercostal muscles (diaphragmatic breathing);
- Differences in the pattern of spontaneous movement of the limbs;
- Difference in tone between the proximal and distal muscles in the upper limbs and between the muscles of the upper and the lower limbs;
- Response to painful stimuli by pressure over bony prominences along the segmental dermatomal distribution of the cord throughout the body;
- The combination of hypotension and bradycardia;
- The presence of priapism.
Bruising over the chest or thoracolumbar spine in association with the presence of normal breathing, the absence of responses to painful stimuli applied to the bony prominences of the lower limbs, and the absence of reflexes in the lower limbs, could be indicative of a lower thoracic cord or cauda equina injury.
Unlike a patient with head injury who is likely to be incontinent of urine on presentation at the accident and emergency department, a patient with combined head and spinal cord injury is likely to be dry for some time before developing overflow incontinence. In the author’s experience, a palpable bladder in a semiconscious or unconscious patient following trauma is a highly suspicious sign of a spinal injury with neurological damage.
Associated Injuries
Double injury and occasionally multiple noncontiguous injuries of the spinal axis are not uncommon following major trauma. Following the diagnosis of a primary injury in the spinal axis, the diagnosis of a secondary injury is often delayed. The incidence of multi-level spinal injuries is reported to be as high as 16.7 %.13
Early recognition is important for the assessment and planning of the treatment in order to avoid further neurological damage when the nondamaging second spinal fracture is proximal to the primary injury. In our series, 55% of patients with multi-level injuries had incomplete neurological lesions on admission.14 Although no definite pattern of injury could be identified in terms of the relationship between the primary and the secondary level, the lower cervical and cervicothoracic lesions were the most frequently involved followed by the upper cervical region. Once a spinal injury has been identified we strongly recommend that the whole spine be examined clinically and radiologically.
The incidence of extra-spinal fractures associated with spinal cord injuries is reported to be about 28%.15,16 When all levels of spinal cord injuries were pooled the most common areas of fracture reported were chest followed by lower extremity, upper extremity, head, and pelvis.15
Loss or impairment of sensation below the level of the spinal cord injury presents one of the greatest challenges to the clinician in the diagnosis of the associated injuries. A thorough clinical examination is paramount to the diagnosis.
The importance of bruises, lacerations, or swellings in these patients cannot be overestimated. Facial bruises with or without bruises on the neck in an unconscious patient should heighten the suspicion of a cervical spinal injury with associated facial, dental, or mandibular injuries. Although there could be any combination of associated injuries with the injury of the spinal axis, there are nonetheless certain patterns of association.
Head injuries, facial injuries, dental, and mandibular injuries can be associated with cervical injuries, and vice versa.17 Thoracic injuries can be associated with fractures of the sternum,18 fracture ribs, hemothorax, fracture clavicle, or fracture scapula.19 A case of upper thoracic spine fracture was reported to be associated with tracheo-esophageal perforation.20
Abdominal injuries are not uncommonly associated with thoracolumbar fractures and lumbar fractures.21,22 Children involved in motor vehicle collisions are particularly at high risk. In one series, almost 10 % of adults with blunt trauma of the thoracolumbar spine had associated abdominal injuries.22 Solid organs and viscus injuries (spleen, kidneys, adrenals, liver, small intestine, and mesentery) have been reported. Patients who sustained multi-level vertebral fractures were more severely injured and had a higher number of solid organ injuries.22 Blunt, abdominal, aortic trauma in association with thoracolumbar spine fractures have been reported mainly when the fracture was caused by a distractive mechanism with or without translation.23
Injuries of the upper limbs including shoulders, wrists, and hands are worthy of specific mention. In the paraplegic and tetraplegic patients the upper limbs will also substitute the functions of the lower limbs during transfer and some activities of daily living, personal care, and hygiene.
Radiological Assessment
In the accident and emergency department, AP and lateral radiographs of the spine are still the commonest procedures and probably the most practical for the diagnosis or the exclusion of an injury of the spinal axis. It is important that the transfer and positioning of the patient is supervised by an experienced clinician and is documented to have been supervised. The absence of a fracture radiologically does not exclude a serious ligamentous injury of the spine nor indeed serious cord damage. An enlarged prevertebral soft tissue shadow can be the only radiological manifestation of a serious spinal injury. The cervicodorsal junction and upper thoracic vertebrae are usually difficult to visualize despite pulling on the arms of the patient while taking a lateral radiograph. The quality of the exposure is likely to improve if an attendant gently pushes the shoulders downward while two other attendants hold a gentle pull on the arms from both the elbow and the wrist. Swimmer’s views are helpful in patients with short thick necks.
Spinal cord injuries without radiologic abnormality (SCIWORA) have been reported in the literature for many decades and may have contributed to a delay in diagnosis in some patients. Although SCIWORA is generally expected in some children, it can also occur in elderly patients with central cord syndrome due to hyperextension injuries of the cervical spine. In the author’s opinion the term SCIWORA needs to be reviewed in the light of the advanced radiological investigations (CT and MRI).
Once a traumatic injury to the spinal axis has been suspected and/or confirmed, in my opinion it is imperative that the whole of the spinal column is radiologically investigated. There is a significant incidence of double injury of the spinal column that ranges between 9.5% and 17%.13,14
Although the CT scan is the investigation of choice for assessing spinal fractures, an MRI scan is usually essential to assess ligamentous injuries, stability, and cord damage. MRI scans are also very valuable in detecting single or multiple vertebral contusions adjacent or noncontiguous to the fracture. The prognostic value of the MRI scan (in terms of neurological recovery) in the acute stage is discussed elsewhere. A baseline MRI scan is, however, essential to compare with subsequent MRI scans in case of neurological deterioration. This deterioration does not only occur in the acute stage, it can also occur anytime throughout the patient’s life. The incidence of MRI-evident posttraumatic syringomyelia is up to 30 % in these patients.24 Fortunately, the clinically manifested effects occur in a much smaller percentage. El Masry and Biyani discussed the pathophysiology and documented the incidence of posttraumatic syringomyelia at various levels and for various densities of lesions.25,26
A baseline chest radiograph is highly advisable especially in tetraplegic/paretic patients and patients with thoracic injuries. Most patients with cervical cord injuries will have impaired respiratory functions. Those patients with thoracic spinal injuries are likely to have associated rib fractures, and/or sternal fractures both of which may add to the biomechanical instability of the thoracic spinal fracture. A lateral radiograph of the sternum is therefore also advisable in all patients with thoracic spinal injuries.
The interpretation of the film taken in the supine position requires radiological expertise. A hemothorax may not result in blunting of the costophrenic angle, but the collection is likely to be seen over the apex of the lungs.
Most patients with thoracic fractures will develop an increase in the paravertebral shadow and an appearance of widening of the mediastinum. Further radiological investigations may be required to exclude mediastinal damage.
Caution needs to be exercised during any procedure undertaken on patients with suspected cord damage, especially those with higher thoracic or cervical cord injury. Because during the stage of spinal shock the sympathetic nervous system is areflexic, patients are usually poikilothermic. In a cold environment they can readily become hypothermic. Hypothermia in patients with cord injury above the level of T5 can result in bradycardia and cardiac arrest. Radiology departments in trauma centers are advised to keep some atropine ready to administer if the pulse of the patient drops below 45/min. In a hot environment the patient can easily become pyrexial.
The Subacute Stage and Long Term
A repeat radiograph of the chest should be considered on the second, third, or fourth post-injury day in patients with thoracic spinal injuries. In the author’s experience about 40-50% of these patients are likely to have an increase in the size of the hemothorax 2448 hours following the injury.
Patients with spinal cord injuries, at all levels, are at risk of developing a delayed ileus and care should be taken not to commence hydration and oral feeding before normal bowel sounds are heard at least 24 hours following injury.
Patients with thoracolumbar and lumbar injuries are likely to develop a retroperitoneal hematoma and a paralytic ileus for a period of time even when the spinal cord has not been damaged. An associated intraabdominal injury is not easy to exclude clinically. Often the radiologist has to come to the rescue. An abdominal ultrasound scan and/or a CT scan are likely to be required if the bowel sounds do not return by the fourth or fifth day post injury. A perforation in the lesser sac can remain undiagnosed for a number of days and requires a high degree of suspicion for exclusion.
In the absence of normal sensation, the combination of vomiting and a distended abdomen with or without pyrexia offer a great diagnostic challenge to the clinician treating spinal cord injury patients. This can happen on a number of occasions during the patient’s life. Although constipation is likely to be the commonest cause, this diagnosis can only be made by exclusion.
Assessment of the Cardiovascular System
The combination of: bradycardia (pulse of 45-60/min), hypotension (systolic blood pressure of 80-90), warm peripheries, visible veins, and good peripheral pulse volume in a patient presenting to hospital following trauma is indicative of a spinal cord injury until otherwise proven. Unlike patients with hemorrhagic shock who exhibit tachycardia in association with hypotension, cold peripheries, and poor volume pulse, and who require bigger intravascular volume replacements, great care should be taken with intravenous fluid administration to patients with bradycardia and hypotension due to SCI. The impaired sympathetic system of the patient, which is responsible for the hypotension and partly responsible for the bradycardia, is usually unable to cope with any excess amount of fluid. The patient can easily develop pulmonary edema and respiratory failure.
Bradycardia can be aggravated by hypoxia, hypothermia, and tracheal suction all of which can cause cardiac standstill. The highest risk is during the stage of spinal areflexia “spinal shock” when the vagus nerve activity is unopposed by the sympathetic nervous system activity. The patient without a previous history of cardiac disease responds readily to cardiac massage and atropine 0.3 mg intravenously provided the cause of the cardiac standstill is effectively treated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree