Introduction
Contrast agents used in magnetic resonance imaging (MRI) can be either endogenous or exogenous. The most common type of endogenous contrast-enhanced MRI is arterial spin labeling (ASL) techniques, which use a dynamic labeling of internal water to measure brain perfusion. ASL is noninvasive, and the sequences needed to acquire this type of imaging are included on most major vendors’ platforms. However, ASL still suffers from poor signal-to-noise ratios (SNRs) and limited spatial coverage. Exogenous contrast agents for MRI, first introduced in the early 1980s, can substantially increase image contrast to facilitate diagnosis of lesions in both brain and body imaging. Beyond simply increasing the conspicuity of lesions, exogenous contrast agents are also commonly used to measure tissue properties such as blood perfusion and permeability. Approximately 30 million MRI examinations are performed in the United States annually, and exogenous contrast agents are used to improve image quality in about 30% of cases. Exogenous contrast agents for MRI are administered either by venous injection or orally and usually include gadolinium (Gd)-, iron-, or manganese-based compounds, with Gd-based contrast agents being the most common. The applications of iron- and manganese-based agents are still in early-stage development. In this chapter, we focus on Gd-based exogenous contrast agents and their applications.
Gadolinium (Gd, atomic number 64) is a paramagnetic heavy metal. Although the Gd(III) ion is quite toxic to humans, chelated-Gd(III) compounds are much less toxic and are referred to as Gd-based contrast agents (GBCA). GBCAs are manufactured by a chelating process in which large organic molecules encapsulate the gadolinium. This procedure reduces the chances of toxicity due to free Gd ions because these stable chelated compounds are predominantly eliminated via the kidneys before the compounds degrade and release free Gd ions. The U.S. Food and Drug Administration (FDA) first approved a GBCA for use in MRI in 1988. Since then, eight additional GBCAs have been approved for use in clinical studies. FDA-approved GBCAs are as follows: Ablavar (gadofosveset trisodium), Dotarem (gadoterate meglumine, Gd-DTOA), Eovist (gadoxetate disodium, Gd-EOB-DTPA), Gadavist (gadobutrol, Gd-DO3A-Butriol), Magnevist (gadopentetate dimeglumine, Gd-DTPA), Multihance (gadobenate dimeglumine, Gd-BOPTA), Omniscan (gadodiamide, Gd-DTPA-BMA), Optimark (gadoversetamide, Gd-DTPA-BMEA), and Prohance (gadoteridol, Gd-DO3A-HP). GBCAs can be divided into two groups: ionic and nonionic agents. Ionic contrast agents typically, but not always, have higher osmolality and more side effects. Nonionic contrast agents have lower osmolality and tend to have fewer side effects. The properties of GBCAs are summarized in Table 5-1 .
| Drug Name | Active Ingredients | Nonionic/Ionic | Recommended Dose (mL/kg) | Indication | Children/Adults | Elimination Half-Life (hours) | Elimination Percentage (%) | Year Approved |
|---|---|---|---|---|---|---|---|---|
| Ablavar | Gadofosveset trisodium | Ionic | 0.12 | MRA | A | 0.48/16.3 a | 78.7 c | 2008 |
| Dotarem | Gadoterate meglumine (Gd-DTOA) | Ionic | 0.2 | CNS | C/A | 1.4 in females, 2.0 in males b | 72.9 in females, 85.4 in males d | 2013 |
| Eovist | Gadoxetate disodium (Gd-EOB-DTPA) | Ionic | 0.1 | Liver | A | 0.9 b | None | 2008 |
| Gadavist | Gadobutrol (Gd-DO3A-butriol) | Nonionic | 0.1 | CNS | C/A | 1.81 b | >90 e | 2011 |
| Magnevist | Gadopentetate dimeglumine (Gd-DTPA) | Ionic | 0.2 | CNS/ body | C/A | 0.2/1.6 a | 91 e | 1988 |
| MultiHance | Gadobenate dimeglumine (Gd-BOPTA) | Ionic | 0.2 | CNS/ MRA | C/A | 2.02 b | >80 e | 2004 |
| Omniscan | Gadodiamide (Gd-DTPA-BMA) | Nonionic | 0.2 | CNS/ body | C/A | 0.062/1.30 a | 95 e | 1993 |
| Optimark | Gadoversetamide (Gd-DTPA-BMEA) | Nonionic | 0.2 | CNS/ Liver | C/A | 0.23/1.73 a | 95 e | 1999 |
| Prohance | Gadoteridol (Gd-DO3A-HP) | Nonionic | 0.2 | CNS | C/A | 0.2/1.57 a | 94 e | 1992 |
a Using the two-compartment model;
b using the one-compartment model;
c elimination percentage within 72 hours;
d elimination percentage within 48 hours;
Although GBCAs are considered to be relatively safe in clinical studies, they are not completely without risks. Recently, associations between nephrogenic systemic fibrosis (NSF) and GBCAs have been reported in a small subset of patients. NSF may result in fatal or debilitating fibrosis. Patients with acute, chronic, and severe kidney disease (glomerular filtration rate [GFR] < 30 mL/min/1.73 m 2 ) have very poor elimination of GBCAs and could have an increased risk of developing NSF due to GBCAs. Because GBCAs increase the risk of NSF, patients with poor elimination should not be administered such contrast agents. Patients in MRI examination with GBCAs should be properly screened and be closely observed during the procedure. Upon any reaction to the drugs, the appropriate therapy must be used, and any case of NSF should be reported to the FDA (1-800-FDA-1088 or www.fda.gov/medwatch ).
Because GBCAs are paramagnetic, they generate a magnetic moment when placed within a static magnetic field, influencing water protons within their local magnetic field and shortening T1, T2, and T2* relaxation times to enhance image contrast. T1 is the spin-lattice or longitudinal relaxation time, which measures how fast the proton magnetization recovers to its equilibrium position. Shortening T1 increases the recovery speed and further increases MR signal in the tissue. T2 is the spin-spin relaxation time, which represents how fast MR transverse magnetization disappears. T2 shortening increases the rate at which the transverse magnetization disappears and further decreases MR signal in the tissue. T2* is the transverse relaxation time including T2 and magnetic field inhomogeneity effects. Although T2* has an effect on MR signal that is similar to that of T2, T2*’s effect is usually much smaller than that of T2. In MR imaging, spin echo sequences generate T2-weighted images and gradient echo sequences usually generate T2*-weighted images.
GBCAs do not cross an intact blood-brain barrier (BBB) and therefore do not accumulate in normal brain. However, disruption of the BBB allows accumulation of GBCAs in lesions such as neoplasms. Within the body, there is no barrier to hinder extravasation of the smaller GBCAs into the surrounding tissue. The rate and degree to which this extravasation occurs are highly elevated in many neoplasms and can be used to accentuate the conspicuity of the lesions. In this chapter, we will describe the measurement of perfusion and permeability in tissues performed by using dynamic contrast-enhanced MRI (DCE-MRI) and dynamic susceptibility contrast MRI (DSC-MRI).
DCE-MRI and DSC-MRI
Dynamic MRI with GBCA can be used to measure two basic physiologic properties: perfusion and capillary permeability. Perfusion is a faster process and requires a faster acquisition with high temporal resolution to capture the first pass of the bolus of contrast agent while it is still intravascular. DSC-MRI is mostly used to measure perfusion with high temporal and low spatial resolution. Permeability is usually a relatively slower process and requires a longer acquisition time to characterize the slow transfer of GBCA from capillaries to the interstitial space. DCE-MRI is generally used to measure permeability using higher spatial resolution and a longer acquisition time.
DSC-MRI acquires a series of T2*-weighted or T2-weighted dynamic MR images before, during, and immediately after a bolus injection of a GBCA. DSC-MRI is widely used for perfusion measurements in brain imaging, which generates a larger signal change with the same concentration of GBCA than does DCE-MRI; this is because of the higher T2* relaxivity of GBCA. DSC-MRI can be routinely acquired as a relatively low spatial resolution volume data set with a temporal resolution of approximately 1 second and an acquisition time of approximately 60 seconds, making DSC-MRI ideal for the study of first-pass kinetics of the GBCA bolus. However, it is difficult for DSC-MRI to measure permeability because the decrease of signal due to T2* effects counteracts the increase in signal caused by T1 effects during the leakage and thus confounds the signal change.
DCE-MRI acquires a series of T1-weighted dynamic MR images before, during, and after a bolus injection of a GBCA. T2* effects can be minimized by using a short echo time. The T1 relaxation rate has a linear relationship with drug concentration, and the T1 relaxivity is largely independent of tissue type. When first introduced, DCE-MRI had a relatively low temporal resolution (>1 minute per image) because of acquisition sequence design, hardware limitations, and the requirement for higher spatial resolution. However, because of improvements in the acquisition sequences and hardware improvements, DCE-MRI can now be acquired as a volume data set with a temporal resolution of approximately 3 seconds. DCE-MRI can be used to measure perfusion and permeability simultaneously but has to have both a high temporal resolution and a sufficiently long acquisition time of approximately 8 to 10 minutes. DCE-MRI measures of perfusion have a lower contrast-to-noise ratio (CNR) than DSC-MRI does because of its lower T1 relaxivity in comparison with the high T2* relaxivity in DSC-MRI. This drawback can be largely mitigated when imaging highly vascularized cerebral tumors, where high drug concentrations can be reached.
DCE-MRI
A complete DCE-MRI study usually includes baseline T1 mapping, dynamic data acquisition, arterial input function measurement, and dynamic data analysis. In the following sections, we will discuss each part of the whole process. DCE-MRI images can be analyzed by using a heuristic method or a suitable tracer-kinetic model to get the proper physiologic metrics related to perfusion and permeability. For convenience, all physiologic parameters in this chapter are summarized in Table 5-2 for later reference.
| Category | Parameters | Normal Range | Unit | Interpretation |
|---|---|---|---|---|
| Perfusion | F p | 20-400 | mL/min/mL | Plasma flow |
| v p | 1-30 | % | Plasma volume <5% for brain | |
| Mixed | K trans | E × F p | 1/min | Volume transfer constant |
| k ep | K trans /v e | 1/min | Interstitium-to-plasma rate constant | |
| Permeability | PS | 0.01-0.1 | mL/min/100 mL | Permeability–surface area product for normal muscle |
| v e | 20-30 | % | Interstitial volume fraction (extracellular extravascular space [EES] fraction) | |
| E | ∝PS < 10-20 | % | Extraction fraction | |
| τ | <5 | Second | Mean intracellular water molecule lifetime |
Baseline T10 Measurement
The baseline longitudinal relaxation time T10, before drug injection, is required for pharmacokinetic modeling analysis. Several methods can be used to measure T1. The variable flip angle (VFA) method is one of most widely used methods, calculating a T1 map by using multiple spoiled gradient echo acquisitions with different flip angles. The VFA method allows rapid high-resolution three-dimensional (3D) acquisitions because of the modern implementation with very short repetition time. Radio frequency (RF) field (B1) inhomogeneity leads to variable actual flip angles in different locations even when the same nominal flip angle is prescribed. To ensure more accurate T1 mapping, B1 mapping has to be assessed for correction of errors caused by B1 inhomogeneity. B1 inhomogeneity correction increases the complexity of the data processing and requires additional acquisition time, which diminishes the advantage of the time-efficient VFA method. A potential alternative method for T1 mapping, T1 inversion recovery, uses a single-shot fast-spin echo sequence with multiple inversion of times (TI). These sequences are less sensitive to B1 inhomogeneity and require similar acquisition times. An example of T1 protocols for the VFA method and the inversion recovery method are given in Table 5-3 for readers’ reference.
| Parameters | Variable Flip Angle | Inversion Recovery | ||||
|---|---|---|---|---|---|---|
| B 0 | 1.5 T | 1.5 T | ||||
| Sequence | 3D spoiled gradient echo | 3D single-shot fast spin echo | ||||
| Vendors | GE | Phillips | Siemens | GE | Phillips | Siemens |
| Sequence name | SPGR | T1-FFE | FLASH | Single-shot FSE | Single-shot TSE | HASTE |
| Time of echo (TE) | 1.0 ms | 78 ms | ||||
| Time of repetition (TR) | 5.0 ms | 4000 ms | ||||
| Flip angles | 2°, 5°, 10°, 15°, 20°, 25°, 30° | 90°-180° | ||||
| Time of inversion (TI) | None | 100, 300, 900, 1500, 2200, 3300 ms | ||||
| Slice number | 16 | 16 | ||||
| Slice thickness | 5 mm | 5 mm | ||||
| Acquisition matrix | 256 × 160 × 16 | 256 × 128 × 16 | ||||
| Average number | 4 | 1 | ||||
| Partial Fourier | None | 6/8 in slice; 5/8 in phase | ||||
| Time/measures | 0.85 minutes | 0.83 minutes | ||||
| Total time | 5.97 minutes | 5 minutes | ||||
DCE-MRI Data Acquisition
DCE-MRI data should be acquired by using a 3D T1-weighted spoiled gradient echo sequence, which is widely available on 1.5 and 3 T scanners from major vendors. For better B1 homogeneity, a body coil should be used as the transmit coil; the receiver coil can be a body or phased array coil, depending on the anatomy being studied. The acquisition volume should cover the whole lesion (or the major lesions) and a feeding vessel with in-plane flow for measuring arterial input function (AIF) if feasible. The ideal echo time (TE) should be less than 1.5 milliseconds to improve SNR and to diminish the T2* effects on signal change. The repetition time (TR) should be approximately 3 to 5 milliseconds to achieve higher temporal resolution and optimal T1 quantification. The temporal resolution should be less than 10 seconds for quantifying perfusion. A small flip angle could cause saturation effects when used with higher tracer concentrations. Therefore 25- to 30-degree flip angles are recommended to minimize saturation effects and balance specific absorption rate (SAR), which measures the amount of energy deposited into the human body by radiofrequency pulses. Faster acquisition techniques, including partial Fourier and parallel imaging, can be used with additional attention to ensure consistency on all scanners. The total acquisition time should be no less than 5 minutes; the optimal is about 8 to 10 minutes to ensure the accuracy of estimating kinetic parameters related to the relatively slow process of permeability. An example of a DCE-MRI protocol is shown in Table 5-4 and can be modified for specific applications. Additional details and sample protocols can be found in a workshop report by the Imaging Committee of the Experimental Cancer Medicine Centres (ECMC) and in the Quantitative Imaging Biomarkers Alliance (QIBA) protocols and profiles.
| Parameters | DCE-MRI | |||
|---|---|---|---|---|
| B 0 | 1.5 T | |||
| Sequence | 3D spoiled gradient echo | |||
| Vendors | GE | Phillips | Siemens | |
| Sequence name | SPGR | T1-FFE | FLASH | |
| Time of echo (TE) | 1.2 ms | |||
| Time of repetition (TR) | 3.5 ms | |||
| Flip angles | 30° | |||
| Parallel imaging | GRAPPA R=2, Nref=24 | |||
| Slice number | 16 | |||
| Slice thickness | 5 mm | |||
| Acquisition matrix | 256 × 192 × 16 | |||
| Bandwidth | 360 Hz/pixel | |||
| Partial Fourier | 6/8 in slice and phase | |||
| Time/measures | 7 seconds | |||
| Measurement number | 50 (minimum) | 80 (optimal) | ||
| Total time | 5:50 min | 9:20 min | ||
Contrast injection should start after at least five measurements have been acquired to allow for a robust nonenhanced baseline reference. The preferred method for contrast agent delivery is a bolus-like injection consisting of a fast constant rate injection of generally 2 to 4 mL/s to ensure that the most meaningful perfusion information is obtained in the early enhancement phase. Because of the relatively small volumes of GBCA being administered, the injection should be immediately followed by a saline flush of 20 to 40 mL administered at the same rate as the bolus to ensure that all contrast agent is cleared from the line. Although a manual bolus injection can be used, a power injector synchronized with the MRI scanner should be used for the most consistent results.
MRI Signal vs. Tracer Concentration
MRI signal is measured in arbitrary units and varies substantially with many factors, including the scanners, coils, field inhomogeneity, and imaging location. Therefore MRI signal is not a suitable measure with which to directly quantify physiologic parameters in large clinical studies. However, MRI signal can be converted to tracer concentration for further modeling analyses. The first step in this conversion is to convert the gradient echo signal into T1 relaxation rate (R 1 = 1/T1). The second step is to calculate the tracer concentration by using an assumed linear relationship: R 1 = R 10 + r 1 ⋅ C, where the baseline R 10 = 1/T10 is measured in a precontrast scan as described previously, r 1 is the T1 relaxivity of the specific GBCA administered, and C is the GBCA concentration. It has been demonstrated that the difference in T1 relaxation rates (ΔR 1 = R 1 − R 10 ) is approximately linearly proportional to the GBCA concentration. Most in vivo studies use an r 1 of approximately 4.0 kg/s/mmol, which is a value originally measured in cartilage. However, r 1 has also been reported to vary in different anatomic locations in animal models for different agents. For example, r 1 for Gd-EOB-DTPA changes from 2.0 in kidney to 10.7 in liver, and r 1 for Gd-DTPA changes from 1.2 in kidney to 4.8 in liver. Additional care should be taken when using a constant r 1 value in studies that may involve various types of tissue.
Heuristic Analysis
Heuristic analyses attempt to extract the important features or attributes of the contrast-enhancing signal curve without any assumptions or inferences about the underlying physiology of the tissue. The main heuristic parameters include initial slope, peak enhancement, time to peak, terminal slope, and initial area under the Gd concentration-time curve (IAUGC) as shown in Figure 5-1 . The IAUGC refers to the time period defined by the first 30, 60, 90, 120, or 180 seconds after bolus arrival, with the IAUGC_60 being the most commonly used in DCE-MRI studies. These parameters are attractive clinically because they provide a simple and straightforward measure of the contrast-enhancing signal curve without requiring further measurements, such as an AIF, but have less physiologic significance and could vary greatly with different protocols, contrast agent injections, and scanners. The IAUGC parameter has a higher reproducibility because it is calculated from the tracer concentration curve by acquiring the additional baseline T10. Therefore measurements of IAUGC have become one of the primary end points in many DCE-MRI studies.

Pattern analysis methods have been proposed to classify DCE-MRI signal curves into several groups on the basis of their curve shapes to differentiate features of benign and malignant tumors. These methods quantify areas with different curve patterns from DCE-MRI data. Pattern analysis method can also be combined with additional quantification methods to automatically generate several quantitative parameters, which are less sensitive to acquisition protocols but still do not require additional measures of an AIF and baseline T10 measurement. One parameter in this hybrid method is highly correlated with the kinetic parameter K ep in the modeling analyses described later and could provide some physiologic significance. The application of this method in DCE-MRI studies is straightforward and can be applied to existing DCE-MRI studies that may not have contained the additional data needed for modeling analyses.
Arterial Input Function
For more elaborate kinetic models, an AIF is necessary. An AIF is one of the dominant sources of variability in evaluating kinetic parameters. Three types of AIFs can be used: an assumed AIF, a measured AIF, and a reference AIF. An assumed AIF can be any kind of predefined function. In the early 1990s, assumed simple AIFs, such as a biexponential function, were used in model analysis. The advantage of using an assumed AIF in the analysis is the simplicity of implementation, but the disadvantage is that it could lead to large systematic errors. An assumed AIF cannot reflect any change in shape of the bolus for different organs or different injections. A measured AIF can be extracted from the vessel in the dynamic data or measured separately in a previous examination. A visual comparison between an assumed biexponential AIF and a measured AIF from a large artery is shown in Figure 5-2 . A reference AIF can be explicitly evaluated or be implicitly assessed by using information from a reference tissue such as muscle.

Because an AIF is crucial for the accuracy of estimating kinetic parameters, researchers began to measure individual AIFs within each subject. To measure it accurately, high temporal resolution (2-3 seconds) is required. A low concentration of contrast agent must be administered to avoid signal saturation in the blood vessel. Both the shape and amplitude of the AIF can still change dramatically depending on which artery is used and where the region of interest is located within the artery to extract the AIF. Therefore vessel orientation, inflow effects, and tumor position must be considered to measure an accurate AIF. However, even with great care, the amplitude of the AIF may still vary substantially (≈50% change) when measured in the same location from a single subject over five visits because of partial volume corruption and timing effects. In certain tumors (e.g., breast tumors, osteosarcoma), no large arteries in which to extract an AIF may be visible within the imaging sections acquired in many subjects. An averaged AIF extracted from a smaller subset of subjects with large arteries within the imaging plane can serve as a surrogate AIF for the whole cohort of subjects. Another option is to use a population-averaged AIF from a cohort of subjects imaged multiple times, which can have an experimentally derived functional form to model the AIF. These AIFs are similar to the assumed AIF, but their amplitudes and shapes are closer to those of measured AIFs and can be used with proper adjustment. This approach of using a population-averaged AIF may substantially improve measurement repeatability.
The reference AIF approach is derived explicitly or implicitly from one or more reference regions of normal tissue such as muscle. These methods assume normal tissue pharmacokinetic properties to allow reverse calculation of the AIF or direct calculation of kinetic parameters in tumors. However, there are two concerns with these methods. First, muscle usually has a very limited contrast enhancement compared to that of tumor and especially artery. Robustness and accuracy become serious problems when trying to estimate large changes in tumors from small signal changes in muscle. Second, pharmacokinetic properties in muscle may be altered by therapy or atrophy during treatment. These variations from the assumed values may cause substantial errors in the derived tumor properties. Although researchers have expended much time and effort to improve its accuracy and reliability, AIF estimation still remains a challenging and dominant factor influencing DCE-MRI analysis.
Modeling Analysis
Within an MR image, each voxel usually includes different tissue compartments such as a vascular space, a cellular space, and an interstitial space (extravascular extracellular space [EES]). The kinetic models describing the dynamic contrast-enhancing process can be divided into three categories: one-, two-, and three-compartment pharmacokinetic models, as shown in Figure 5-3 . In the one-compartment model shown in Figure 5-3A , a single compartment is assumed, where the dominant effect is the relationship between the signal and drug concentration within the vascular space while contributions from the other two tissue compartments can be neglected owing to relatively small size and/or extremely rapid water exchange between compartments. In the two-compartment model shown in Figure 5-3B , effects from both vascular space and EES are considered for fitting the data more accurately. This model assumes that contrast does not cross the cellular membrane and that the water exchange across the membrane is slow enough that the cellular space can be ignored. The three-compartment model shown in Figure 5-3C includes all three tissue spaces and becomes much more complicated. Although the GBCA still does not cross the cellular membrane, the water exchange across the cellular membrane is fast enough that the water within the cell also experiences the shortened T1 effects of the contrast.

The number of fitted parameters usually increases as the number of compartments increases, which should provide a better fit to the data. However, overfitting, which occurs when a model is excessively complex with too many parameters, could become an issue. The effects from random error or noise are emphasized instead of the underlying physiologic relationships in case of overfitting. If this occurs, then the model generally has poor predictive performance in clinical trials because it can exaggerate minor fluctuations in the data. Therefore the optimal model is the simplest model that fits the data with the least number of parameters.
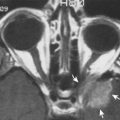
DCE-MRI analysis was first applied to the averaged concentration curve for a whole tumor because it is easy to perform and the averaged curve has higher SNR than that of a single voxel. Researchers found that signal curves could be dramatically different in different tumor regions, as shown in Figure 5-4 . Data have to be analyzed pixel-by-pixel to generate parametric maps for capturing physiologic variation inside heterogeneous tumors. DCE-MRI data can vary dramatically for different types of tumors, with a model performing well for one kind of tumor and failing in another. This characteristic resulted in many different kinetic models being proposed in the past, but under certain conditions and assumptions, these kinetic models could all be derived from one another. Three of the most popular kinetic models will be described in detail below: Tofts (one-compartment), extended Tofts (two-compartment), and shutter-speed models (three-compartment). For further reading to understand the details and complicated relationships among different kinds of kinetic models, we recommend the excellent review on DCE-MRI modeling by Sourbron et al.

One-Compartment Model
A one-compartment model describes a voxel or a region of interest as a single compartment to simplify the impulse response function to a monoexponential decay. The single compartment could refer to vascular space, EES, or the combination of both. Therefore there are four regimes: (1) fast exchange regime, (2) weakly vascularized regime, (3) highly vascularized regime, and (4) no exchange regime. The fast exchange regime assumes the GBCA exchange between vascular space and EES is very fast, such that these two spaces can be treated as a single compartment. The weakly vascularized regime applies to tissues such as connective tissues or partially necrotic tumor tissues, which have a less abundant supply of capillaries. The highly vascularized regime applies to tissues such as large vessels or tumor edge, which have a dominant supply of capillaries. The no exchange regime refers to the brain, in which there is no drug exchange between the vascular space and the EES because of the BBB.
In the early 1990s, Tofts proposed a simple one-compartment model, which is also referred to as the Tofts/Kety model and belongs to the weakly vascularized regime. The Tofts model can be written as:
C t ( t ) = C p ( t ) ⊗ I ( t ) = C p ( t ) ⊗ K trans ⋅ e − K trans v e ⋅ t
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree