Critical Care Echocardiography
INTRODUCTION
Critical care ultrasound (CCUS) comprises ultrasound evaluation of the heart, lungs, pleural space, abdomen, vascular access, and evaluation of venous thrombosis. CCUS has been used by emergency medicine and critical care physicians for at least 15 years (1,2). Recently, several societies have published position papers, training guidelines, competency statements, and educational curricula on CCUS (3–7). It is important to recognize that CCUS is not meant to replace traditional diagnostic ultrasound (US). CCUS is designed to be used as a series of simplified, focused examinations that can quickly rule in or rule out a diagnosis, or support the need for additional testing, imaging, or procedures. The advantages to CCUS are that it is noninvasive, performed and interpreted by the physician caring for the patient at the bedside, can be easily repeated, and is rapidly available 24 hours a day. This chapter will review the use of focused transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) in critically ill patients, and during advanced cardiac life support (ACLS). The chapter will also briefly review the use of focused echocardiography in the diagnosis of common complications seen in the intensive care unit (ICU).
FOCUSED, GOAL-DIRECTED ECHOCARDIOGRAPHY
Multiple protocols for echocardiography in critically ill patients have been described and all have common concepts including:
1. They are all rapidly applied, focused examinations.
2. They can all be learned with relatively brief training.
3. They all use some combination of four to six limited views (subcostal, apical, parasternal, and pleural).
4. They are all performed real time, by the treating physicians at the patient’s bedside.
5. The examination can and should be repeated over time to evaluate the effects of therapeutic interventions.
6. The examinations are not meant to replace traditional diagnostic examinations.
FOCUSED GOAL-DIRECTED TRANSTHORACIC ECHOCARDIOGRAPHY
This section will describe the standard views for a focused, goal-directed echo (GDE) and transthoracic echocardiography (TTE). Views can be grouped according to probe position, namely parasternal, apical, and subcostal views. This can be further divided into axis (long and short) and chambers views (two and four) (Fig. 18.1).
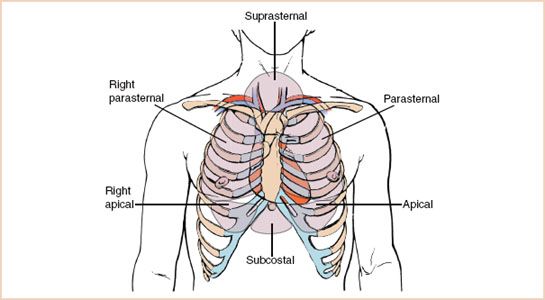
FIGURE 18.1 This diagram demonstrates the various transducer locations used in echocardiography. (From Henry WL, DeMaria A, Gramaik R, et al. Report of the American Society of Echocardiography Committee on Nomenclature and Standards in Two-dimensional Echocardiography. Circulation. 1980;62:212–217, with permission.)
Parasternal Long Axis
The parasternal window is found immediately adjacent to the sternum, in the third or fourth intercostal space. Images obtained in this window are greatly improved by left lateral decubitus positioning, which brings the heart closer to the chest wall. The parasternal long axis (Fig. 18.2) provides images of the aortic and mitral valves, the left atrium and ventricle, and a small portion of the right ventricular outflow tract. The septum and posterior walls of the left ventricle are seen in this view (Video 18.1).
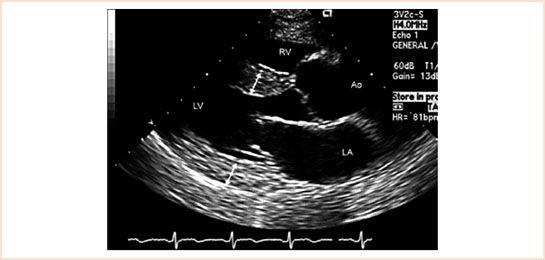
FIGURE 18.2 Transthoracic two-dimensional echocardiogram recorded in a parasternal long-axis view revealing the right ventricle, left ventricle, left atrium, and proximal aorta as well as septal and posterior wall thickness (double-headed arrows).
Parasternal Short Axis
By rotating the probe 90 degrees, the parasternal short axis is seen. Views at the midventricular level at the level of the papillary muscles allow for evaluation of left and right ventricular chamber size and wall motion abnormalities (Fig. 18.3, Video 18.2).

FIGURE 18.3 A parasternal short-axis view at the level of the mitral valve is shown.
Apical Four-chamber
This window is found at the ventricular apex, or point of maximal impulse (PMI), near the anterior axillary line. Images are greatly improved with lateral decubitus positioning, making this view more difficult to accomplish in ICU patients. The apical four-chamber view (Fig. 18.4) provides a global picture of all four chambers. Chamber size and ventricular interdependence can be evaluated (Video 18.3).
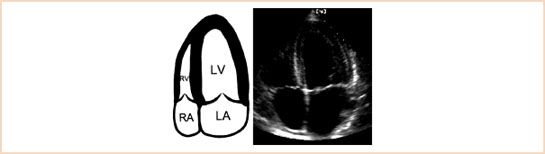
FIGURE 18.4 The apical four-chamber view is shown. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Apical Two-chamber
Accomplished by rotating the transducer 90 degrees, the apical two-chamber allows visualization of the left ventricular anterior and inferior walls (Fig. 18.5).
FIGURE 18.5 Apical two-chamber view. In the apical two-chamber view, small portions of the posterior mitral leaflet are seen laterally and medially with the anterior leaflet filling most of the annulus area. Part of a papillary muscle has been shown for orientation, but the papillary muscles are located symmetrically posterior to the image plane. The tomographic plane has been rotated with the apex of the sector at the top.
Subcostal Four-chamber
The subcostal window is found just inferior to the xiphoid process. This image is difficult to obtain in patients with midline abdominal incisions or mediastinal chest tubes. All chambers of the heart can be visualized with this view (Fig. 18.6, Video 18.4). The inferior vena cava (IVC) can also be examined by rightward angulation of the probe allowing the ultrasound beam to transmit through the liver (Fig. 18.7, Video 18.5).
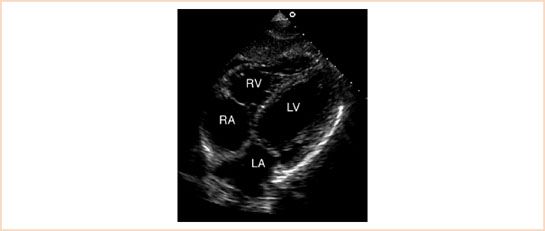
FIGURE 18.6 A subcostal four-chamber view is demonstrated. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
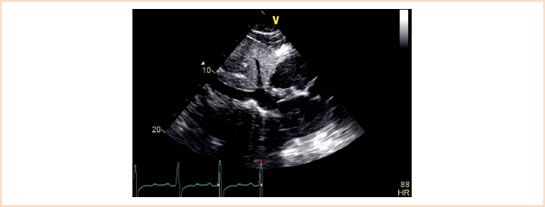
FIGURE 18.7 The inferior vena cava near the hepatic vein. Note the liver provides the acoustic window.
Pleural Ultrasound
Although not included in conventional TTE protocols, evaluation of the pleural spaces should be included when assessing causes of hypotension and hypoxia. Many lung pathologies are definitively diagnosed with radiographic studies, but ultrasound provides real time evaluation, especially in circumstances where x-ray or CT scan is not available. In unstable patients, “the usefulness of thoracic ultrasonography rests with its immediate application” (8). Evaluation of the pleural and lung parenchyma can be done by placing the transducer between the ribs, and serially scanning the lungs in multiple longitudinal planes. If findings are abnormal, comparison with normal lung tissue is imperative. Images are actually of the interface between chest wall and lung, as the air-filled lung provides poor images. A normal examination consists of the movement of the pleura caused by normal ventilation, called the sliding, or gliding sign (9,10). Absence of this sign is indicative of a pneumothorax (Figs. 18.8 and Figs. 18.9).
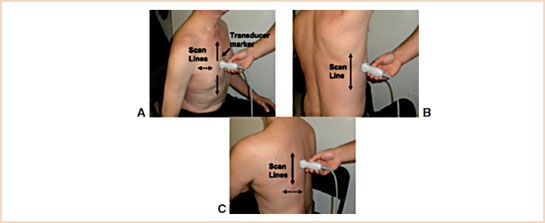
FIGURE 18.8 Ultrasonograph scan lines. A: Anterior scan line. The ultrasound probe is held firmly perpendicular to chest wall. The ultrasonographer moves the ultrasound probe cephalad and caudad in one longitudinal line and then moves either lateral or medial and repeats a longitudinal scan. Transducer marker points cephalad. B: Midaxillary scan line. C: Posterior scan line. (The patient provided written consent for the use of this photograph.) (From Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary specialist. Chest. 2011;140:1332–1341.)
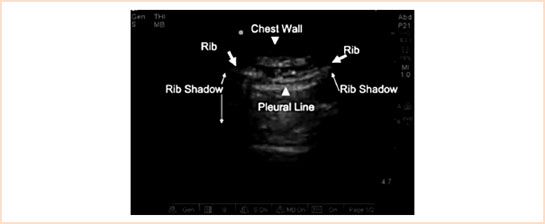
FIGURE 18.9 Normal pleural line. Longitudinal anterior chest ultrasonograph displaying typical anatomic landmarks in normal lung (8).
ECHOCARDIOGRAPHY AND ADVANCE CARDIAC LIFE SUPPORT
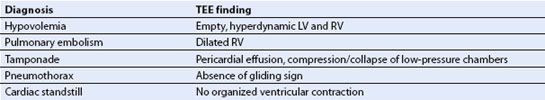
Use of TTE during cardiopulmonary resuscitation (CPR) has become increasingly widespread, as familiarity and skills increase. It is most useful in pulseless electrical activity (PEA) and very low flow states, which carry a high mortality rate, but may be associated with identifiable and potentially treatable causes. The use of TTE during ACLS can identify several of these potentially correctable causes (11) (Table 18.1).
TABLE 18.1 Causes of Cardiac Arrest with TEE Findings
TTE is also beneficial in differentiating low flow states versus true PEA, as well as the return of spontaneous circulation. Many authors have found that clinicians are inconsistent in their ability to detect a pulse during CPR (12–15). Other monitors, such as pulse oximetry or noninvasive blood pressure measurement, are often unreliable in severe hypotension. TTE provides direct visualization of cardiac wall motion, allowing assessment of organized cardiac contraction and return of circulation. The focused echocardiographic evaluation in resuscitation (FEER) examination (16) and cardiac arrest ultrasound examination (CAUSE) (17) are two protocols specifically created for cardiac arrest and resuscitation.
The diagnostic abilities of echocardiography are proven, but the ability to appropriately utilize the technology is still questionable. Concerns regarding interruption of chest compressions and training of responders utilizing echo has been addressed in several studies, with promising results (16). The 10-second pulse check has been utilized in several of the aforementioned studies as a period to perform a scan without interruption of CPR, with evidence of rapid image acquisition and interpretation (16–18). The utility of echocardiography in cardiac arrest will continue to evolve.
FOCUSED GOAL-DIRECTED TEE
There are many critically ill patients where performing a goal-directed TTE is not possible due to dressings, drains, chest tubes, patient characteristics, or positioning difficulties. Provided there are no contraindications to placement of the TEE probe, it is reasonable to perform a focused goal-directed TEE examination using standard views that are similar to those described for goal-directed TTE, in these patients. Immediate clinical decision-making can be greatly aided by goal-directed TEE, followed by a comprehensive TEE examination once hemodynamic stability is restored.
GOAL-DIRECTED TEE VIEWS
Similar to goal-directed TTE, goal-directed TEE would use the following views:
• ME four- and five-chamber views
• ME bicaval
• ME RV inflow–outflow
• TG midpap SAX
• TG midpap LAX
• ME evaluation of pleural spaces
ME FOUR- AND FIVE-CHAMBER VIEWS
This ME four- and five-chamber views (Figure Chapter 2) provide a quick overview of atrial size and function, right ventricle and left ventricle size and function, tricuspid and mitral valve function, and the presence or absence of pericardial fluid. The five-chamber view adds additional information about the aortic valve.
ME RV INFLOW–OUTFLOW VIEW
In the ME RV inflow–outflow, the RVOT and the pulmonic valves are seen (Figure Chapter 2) allowing for evaluation of RV size and function and pulmonic valve function.
ME BICAVAL VIEW
The bicaval view shows the intra-atrial septum, right atrium (RA), SVC, and IVC allowing for size determination of these structures plus placement of intracardiac lines (Figure Chapter 2).
TG MIDPAP SAX VIEW
The TG midpap SAX view (Figure Chapter 2) provides information on right and left ventricle size and function, and regional wall motion in the major distribution of the left, right, and circumflex coronary arteries.
TG LAX
The TG LAX view allows evaluation of LV size, function, and wall motion, as well as assessment of the mitral valve, and left atrium (Figure Chapter 2).
BILATERAL PLEURAL SPACE VIEWS
In the midesophageal position, rotation of the probe to the patient’s right can evaluate the right pleural space; rotation to the patient’s left can evaluate the left pleural space and descending thoracic aorta.
The use of these views should allow the rapid assessment of hypotension, global right and left dysfunction, myocardial ischemia, volume status, severe valvular disease, pleural and pericardial effusion, and pericardial tamponade.
Recently, a small miniaturized TEE probe (Fig. 18.10) has been approved by the FDA and can be left in place for 72 hours (ImaCor, Inc. Garden City, New Jersey). This technology may prove to be a useful device to aid in the ongoing assessment and treatment of hemodynamically unstable patients.

FIGURE 18.10 Miniaturized transesophageal echocardiography (TEE) probe has been approved by the FDA and can be left in place for 72 hours.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree