Fig. 14.1
Anatomy of the deep and superficial vein systems of the leg: 1 external iliac vein, 2 internal iliac vein, 3 inguinal ligament, 4 common femoral vein, 5 femoral vein (formerly superficial), 6 deep femoral vein, 7 great saphenous vein, 8 small saphenous vein, 9 popliteal vein, 10 perforating veins, 11 superficial communicating vein, 12 anterior tibial vein, 13 posterior tibial vein, 14 peroneal vein (From Strauss (1995))
Copyright: Springer
It must be emphasised that the term “superficial femoral vein” has been replaced by “femoral vein” (Caggiati et al. 2002). The term “communicating veins” is reserved for linking veins within the same system.
The deep veins of the leg accompany the arteries of the same name and are generally paired in the calf. However, their junctions are not paired and their locations are variable. In the context of diagnosing a deep vein thrombosis, the posterior tibial and peroneal veins are the most frequently affected.
The posterior tibial veins arise in the deep calf compartment and join the peroneal veins. They are joined also by perforating veins from the posterior arch veins and the great saphenous vein (Chaps. 2 and 9). Using ultrasound they are best visualised from the medial side. In the lower third of the calf, their course is relatively superficial where they are easily noticeable. This is apparent especially in the standing patient because of their paired position in relation to a central artery (Fig. 14.2a).
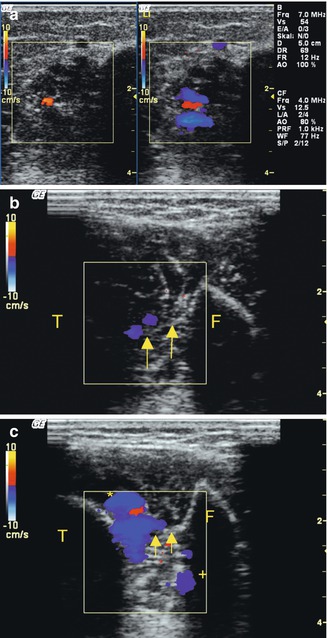
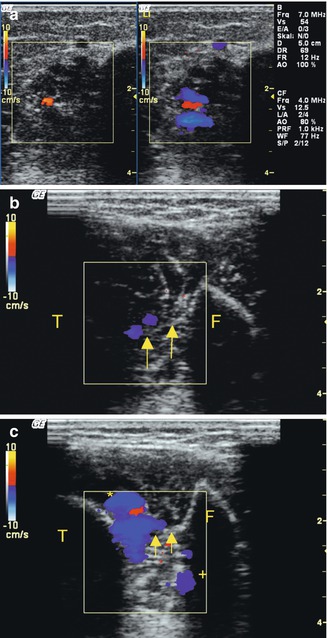
Fig. 14.2
(a) Transverse view through the distal and middle thirds of the calf in a standing patient. The posterior tibial artery is shown with its accompanying veins. Left, at rest. The tibial artery (red) is seen between two veins (black). The great saphenous vein is seen at the top of the colour duplex window. Right, during muscular systole. The posterior tibial veins demonstrate antegrade flow (blue). (b) Transverse view through the front of the calf in a standing patient. The probe has been placed lateral to the edge of the tibia. The paired anterior tibial veins are shown during muscular systole (blue) between the tibia (T) and fibula (F) but anterior to the interosseous membrane (yellow arrows). (c) Transverse view lateral to the edge of the tibia during muscular systole. The anterior tibial veins are shown with the anterior tibial artery in the centre . In addition, the peroneal veins (+) can be seen on the posterior side of the interosseous membrane (yellow arrows)
Copyright: [Author]
The anterior tibial veins are usually small so they cannot be always identified with certainty. They run anterior to the interosseous membrane and are best shown by positioning the probe transversely and lateral to the edge of the tibia (Fig. 14.2b, c). In the upper third of the calf, they pierce the interosseous membrane and run posterior where they join the posterior tibial and peroneal veins at a variable level to form the popliteal vein.
The peroneal veins run upwards on the anterior side of the interosseous membrane just medial to the fibula. In their course in the upper part of the calf, they receive blood from the muscle veins. They are best identified higher up in the calf where they form large calibre calf veins. On ultrasound they are best seen from a posterior viewpoint.
The gastrocnemius and soleus veins are the most clinically significant muscle veins in the calf. They have a large lumen in the standing patient, and they are often the point of origin of a deep vein thrombosis. The gastrocnemius veins join the popliteal vein either in isolation or together with the small saphenous vein at an acute angle (Sect. 2.5 and Figs. 8.14, 8.15, 8.16, and 8.17).
Knowledge of the variations in this region is important for diagnosing thrombosis. In one study (Kubik 1985 in Appendix 2), a single popliteal trunk vein was found in the popliteal fossa in only 55 % of legs. In 40 % there were two trunk veins which joined the femoral vein, generally together to form a single femoral vein. However, in around 2 % of cases, duplicate trunk veins join duplicate femoral veins. In 5 %, three or more trunk veins are present in the popliteal fossa. In addition, the small saphenous vein and its cranial extension (vein of Giacomini) may run through the popliteal fossa (Chap. 8).
In the thigh, the upward extension of the popliteal vein from the adductor hiatus to its junction with the deep femoral vein is known as the femoral vein (Caggiati et al. 2002). The term superficial femoral vein should no longer be used in order to avoid potentially dangerous confusion with superficial veins in clinical treatment decisions. For example, superficial vein thrombosis (phlebitis) may be a thrombosis of the great saphenous vein, but it usually does not involve the “superficial” femoral vein, or a diagnosis of superficial femoral vein thrombosis may indicate to some less experienced practitioners a thrombus in a superficial vein rather than the very significant deep venous thrombosis that actually is present. The femoral vein courses upwards, winding medially around the femur to reach an anterior position in the groin. Around 2–7 cm below the skin crease of the groin, it is joined by the deep femoral vein. At this point it becomes the common femoral vein (Fig. 7.20). A deep vein thrombosis can be missed easily if only one of the limbs of a duplicate femoral vein is involved (Fig. 14.3).
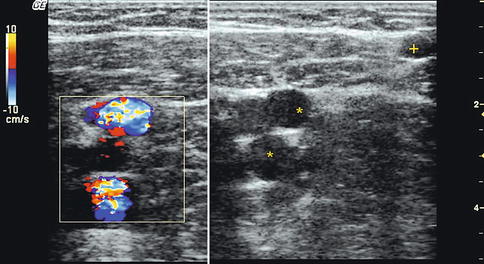
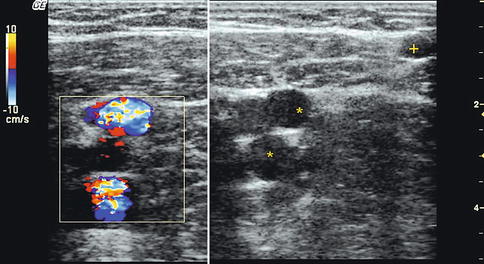
Fig. 14.3
Transverse view through the thigh demonstrating duplication of the common femoral vein during muscular systole (left) and in B scan (right). Approximately 5 cm further down the great saphenous vein (+) is also visible in the image (on the online material there are further examples of duplicate femoral and popliteal veins with thrombi in one of the two lumens)
Copyright: [Author]
The deep femoral vein can generally only be seen on ultrasound near its junction with the femoral vein from the posterolateral aspect (Fig. 7.20).
The common femoral vein is only a few centimetres long. It is joined by the great saphenous vein and some other tributaries which enter it directly in the region of the saphenofemoral junction. The term saphenofemoral junction is preferred to synonyms like “crosse” or “confluence of superficial inguinal veins”. The common femoral vein then runs cranially under the inguinal ligament where it becomes the external iliac vein.
14.2 Deep Leg Vein and Muscle Vein Thrombosis
14.2.1 Definition of Deep Vein Thrombosis
In clinical practice deep vein thrombosis is a thrombus formation in the deep veins of the leg.
In most cases the proximal extent of a thrombosis is easily visualised and well delimited. Thus, a calf vein thrombosis is termed when the proximal end of the thrombus is below the popliteal vein. In calf and popliteal vein thrombosis, the proximal end of the thrombus ends in the popliteal vein. If the femoral vein is thrombosed up to the inguinal ligament, this is described as a calf, popliteal and femoral vein thrombosis. A further stage may involve a thrombosis of the iliac vein. Here the proximal end of the thrombus remains in the iliac vein, below the junction with the inferior vena cava (Table 14.1).
Table 14.1
Stages of deep vein thrombosis
Description | Location | Proximal limit |
|---|---|---|
One level | Limited to the calf veins | Below the popliteal vein |
Two levels | Calf and popliteal veins | Popliteal vein |
Three levels | Calf, popliteal and thigh veins | Femoral vein or common femoral vein |
Four levels | Calf, popliteal, thigh and pelvic veins | Iliac vein |
Deep vein thrombosis may ascend in an ordered fashion from the calf upwards involving the upper segments in sequence. Less frequently they may develop in a localised segment within the thigh, and rarely, they may descend from the iliac vein (Sect. 14.2.4). Thrombosis is a dynamic process with concurrent propagation, detachment, resolution and recanalisation occurring in varying degrees.
14.2.2 Diagnostic Techniques
The historical technique for diagnosing a deep vein thrombosis used to be with CW Doppler ultrasound. Its diagnostic value is limited because of incomplete imaging and a diagnosis based on exclusion. For example, if there is duplication a wrong diagnosis may result. Thrombosis of one limb may not be recognised because of incomplete imaging, and the patent remaining limb may give the false reassurance of a negative diagnosis. Furthermore, the diagnostic criteria using CW Doppler ultrasound are very dependent on the experience and technique of the examiner. This leads to a high risk of misinterpretation. Whilst the safety of a diagnosis in the proximal veins is quite good, with a maximum sensitivity of 80–85 % and a specificity of 85 %, the sensitivity and specificity in the calf are unacceptably low.
Now that B scan and duplex ultrasound are generally available, these techniques should be used exclusively for diagnosing thrombosis. They have greater diagnostic precision. For decades ascending phlebography was the gold standard test in the diagnosis of a deep vein thrombosis. However, venous compression ultrasound, and its systematic use in the technique of complete compression ultrasound (CCUS), has now pushed phlebography into the background (Schellong et al. 2009). Other points in favour of compression ultrasound are its non-invasive nature and the practical advantage of a rapid on-the-spot diagnosis. This is because of the portability of the ultrasound machine in everyday clinical use. Furthermore, the simultaneous use of B scan ultrasound may help in the differential diagnosis. These include recognition of a ruptured Baker’s cyst, torn or bruised muscle fibres, an aneurysm, compartment syndrome or a tumour. Tissue ultrasound also makes it possible to determine the location and extent of oedema. The above factors have led to a considerable increase in examination frequency as compared to phlebography. High-quality compression ultrasound is now readily available in most hospitals.
The few remaining indications for conventional phlebography




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree