Surgical neck management
Definition
Radical neck dissection
En bloc removal of neck levels I–V, sternocleidomastoid, internal jugular vein, spinal accessory nerve (CN XI)
Modified radical neck dissection
Removal of neck levels I–V but sparing of at least one uninvolved non-lymphatic structure (sternocleidomastoid, internal jugular vein, and/or accessory nerve)
Selective neck dissection
Removal of neck levels I–V, with preservation of at least one nodal level
Types
Supraomohyoid
Typically performed in oral cavity carcinomas, levels I–III, or in occasional skip metastases, to level IV (referred to as extended supraomohyoid neck dissection)
Lateral
Typically performed in oropharyngeal, hypopharyngeal, and laryngeal carcinomas: levels II–IV
Anterior compartment
Thyroid carcinomas at highest risk: level VI
Well-lateralized N + tumors after unilateral neck dissection strongly warrant bilateral postoperative radiation therapy, due to altered lymphatic drainage.
Factors strongly recommended for postoperative chemoradiation, per EORTC 22931 and RTOG 9501, are extracapsular extension and positive margins.
2 Diagnostic Workup Relevant for Target Volume Delineation
Clinical examination, CT with IV contrast, and PET scan are the best modalities for the majority of cases. PET scan is helpful for small FDG-avid nodes that fall under size criteria on CT scan. Note the PET fusion may be misleading due to patient movement and should be evaluated closely for any inconsistencies without CT correlate. Ultrasound can be helpful when combined with fine-needle aspiration for staging the neck when other radiographic modalities are nondiagnostic.
MRI with contrast may be helpful in those who cannot receive CT with IV contrast and in cases where nodal adenopathy is obscured or is not easily delineated with contrast CT.
3 Simulation and Daily Localization
CT simulation with 3 mm slice thickness and IV contrast is preferred to ease delineation of vascular structures from lymph nodes. Supine patient positioning with rigid head cradle with the neck extended to reduce oral cavity exit dose is recommended. A custom thermoplastic mask to immobilize the nose, chin, and forehead is utilized. Shoulder pulls or other reproducible devices are used to reduce beam interference and allow adequate neck exposure. The CT simulation scan should encompass adequate superior extent of coverage of the primary disease and inferiorly to the level of the carina.
Image fusion depending upon the primary disease may include MRI and/or PET to aid in delineating involved gross disease in the neck. Attention should be paid to image fusion between primary disease and fusion to nodal disease, as patients will not have PET images in the CT simulation position (neck extended, shoulders pulled down).
Mediastinal windows should be used for contouring the neck nodal contents.
IGRT is recommended to aid in decreasing the PTV margins, depending upon patient positioning reproducibility and treatment machine considerations.
Uninvolved glottic larynx may be spared to limit RT-related speech disorders. Two possible techniques to treat the entire neck include an extended field IMRT or split field using an upper IMRT field matched to a lower anterior neck field (Fig. 1). Advantages of a split field include significantly reduced mean dose to the uninvolved larynx and inferior pharyngeal constrictors (Caudell et al. 2010). This technique is not recommended in laryngeal, hypopharyngeal, or unknown primary head and neck cases or when gross primary or nodal disease is present at the matchline or inferior to the larynx. In these cases, extended field IMRT will provide excellent coverage, whereas a split field may contribute to matchline failures or underdosage (Lee et al. 2007).
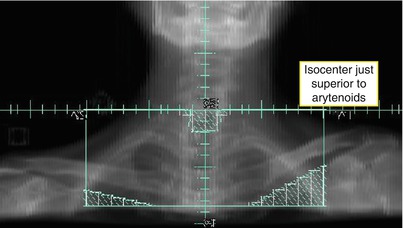
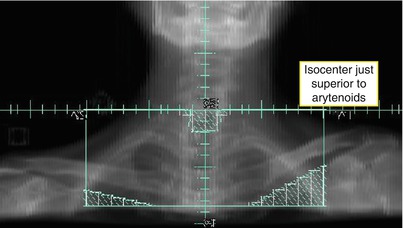
Fig. 1
Beam’s eye view of low anterior neck field
4 Target Volume Delineation and Treatment Planning
Fractionation schemes may vary between dose-painting IMRT and conventional IMRT (Table 2.) Suggested target volumes for nodal GTV and CTVs are detailed in Tables 3, 4, and 5.
Table 2
Selected IMRT dose fractionation schemes for the neck
Concomitant dose-painting IMRT | Postoperative dose-painting IMRT | Definitive dose-painting IMRT | |
|---|---|---|---|
Total dose/dose per fraction (Gy) | |||
GTV | 69.96/2.12, 66/2.0a | 70/2.0c | 69.96/2.12 |
70/2.0b | |||
CTVhigh risk | 59.4/1.8 | 66-60/2.2-2.0 | 59.4/1.8 |
59.5/1.7b | |||
CTVlow risk | 54/1.64 | 54/1.8 not surgically manipulated | 56/1.7 |
56/1.70b | |||
Optional CTV | |||
CTVlow neck | 50.4/1.8 | ||
Table 3
Suggested target volumes for involved nodal disease
Target volumes | Definition and description |
|---|---|
Concomitant or definitive dose-painting IMRT | |
GTV70 | Neck nodes: clinically involved, nodes ≥ 1 cm, central necrosis, FDG-avid on PET, or biopsy proven. Include any suspicious or questionable nodes |
GTV66 | Small, involved nodal disease can be treated to 66 Gy |
CTV70 or 66 | No margin from GTV. Consider GTV70 or 66 + 5–10 mm margin if unclear or imaging quality is reduced |
PTV70 or 66 | CTV70 + 3–5 mm, variable |
Postoperative IMRT | |
CTVpostop66 | Extracapsular involvement. 70 Gy may be needed for residual gross disease |
PTVpostop66 | CTVpostop66 + 3–5 mm, variable |
Table 4
Suggested target volumes for high-risk nodes
Target volumes | Definition and description |
|---|---|
Concomitant or definitive dose-painting IMRT | |
CTV59.4 | Typically, one level above and below grossly involved nodal disease. May involve entire involved muscle or at least one level above and below the muscle if ECE is present
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|