Fig. 38.1
Hepatic micrometastases detected by using an indocyanine green fluorescent system are demonstrated. Although a hepatic tumor was not readily observable via macroscopic inspection, a fluorescent lesion was delineated using near-infrared imaging, and metastatic adenocarcinoma was confirmed via histological examination of the collected specimen
The gallbladder and extrahepatic bile ducts which contain biliary juice with physiologically secreted ICG showed fluorescence. Additionally, simple biliary cysts could also be positive for NIR examination. When those benign foci were excluded, the false-positive fluorescence rate was 7.8 % (8/102 patients) in our experience. Both the false-positive samples and those with histologically confirmed micrometastases via frozen section examination were submitted for further histological evaluation.
38.4 Histopathological Features of Hepatic Micrometastases
Our histopathological examination revealed that the hepatic micrometastases from pancreatic cancer detected by using fluorescence imaging were mainly located at the portal triad (Fig. 38.2). Most of them seemed to be derived from the tumor thrombi of the portal vein in the intrahepatic portal triads, and their extravenous invasion caused desmoplastic reaction around the foci. Such a reaction then resulted in obstruction and stasis of local biliary flow and bile stasis at the peripheral liver (Fig. 38.3). Thereafter, focal dilation of the biliary ducts was frequently observed in the specimens with hepatic micrometastases.
Fig. 38.2
Histopathological findings of hepatic micrometastases from pancreatic cancer are shown. Metastatic adenocarcinoma originating from the portal thrombi invaded toward the parenchyma of the portal triad. Desmoplastic reaction due to tumor invasion caused local biliary obstruction and resulted in dilation of the peripheral bile ducts (arrows)
Fig. 38.3
Schematic diagrams of hepatic micrometastases and their fluorescence mechanism are shown. Micrometastases do not fluoresce, but indocyanine green-contained stagnant bile caused by cancer development at the portal triad does under near-infrared examination
We observed eight cases of false-positive fluorescence in which benign foci were not distinguishable from micrometastases during intraoperative gross examination. Histological examination of the permanent specimens from those cases revealed different biliary congestive conditions including biliary hamartoma, focal steatohepatitis, and cholangiectasis of unknown origin [17]. Thus, some types of bile stasis were found in all cases with abnormal hepatic fluorescence regardless of the histological confirmation of micrometastases. We therefore hypothesize that the ICG-containing stagnant bile is the reason for fluorescence, and hepatic micrometastases themselves do not fluoresce [10, 17]. As a result, the size and location of the fluorescence are not in accord with those of the actual micrometastases (Fig. 38.4). Moreover, diffuse fluorescence was observed in the entire liver of patients with obstructive jaundice, owing to biliary stasis, which supports our hypothesis. In contrast, metastatic foci showed negative fluorescence in those patients (Fig. 38.5). This finding of false-positive results might be associated with inadequate sample collection.
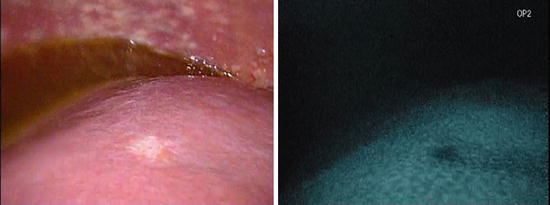
Fig. 38.4
The site and area of fluorescence observed on the liver surface were not in accord with those of the actual hepatic micrometastases
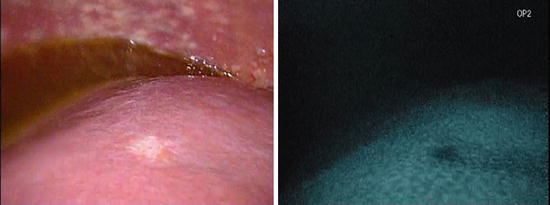
Fig. 38.5
Macroscopic features of hepatic micrometastases from pancreatic cancer detected in a patient with obstructive jaundice are shown. The liver fluoresced diffusely on indocyanine green near-infrared examination, but the metastatic focus observable via gross inspection did not
38.5 Clinical Impact of Hepatic Micrometastases
The most important issue regarding hepatic micrometastases from pancreatic cancer is whether they have the same clinical significance as the overt distant metastases. To date, we have treated the two conditions similarly [10]. In cases of histologically confirmed hepatic micrometastases, even if the disease is considered as loco-regionally resectable stage, systemic chemotherapy is administrated after exploratory surgery or palliative bypass operation. On the other hand, patients without hepatic micrometastases (including those with false-positive findings) undergo radical or palliative surgery according to other staging factors. All patients are periodically followed up with MDCT regardless of curative or palliative surgery.
Hepatic overt metastases were more frequently observed in patients with micrometastases (14/18, 77.8 %) within 6 months after the surgery than in those without (7/84, 8.3 %) (Fig. 38.6). The short-term hepatic relapse often developed in multiple lesions and widespread hepatic area. Therefore, the micrometastases detected during surgery seem to have similar clinical impact to that of overt hepatic metastases. Resection of hepatic micrometastases has little clinical validity even when the number of lesions is limited. In addition, systemic chemotherapy is often unable to control the liver disease; therefore, some liver-targeted therapies (i.e., perfusion chemotherapy, radiation) may be needed for patients with hepatic micrometastases [18, 19]. On the contrary, as the probability of hepatic relapse in patients without hepatic micrometastases is significantly lower, loco-regionally curative therapies may play an important role in those patients.