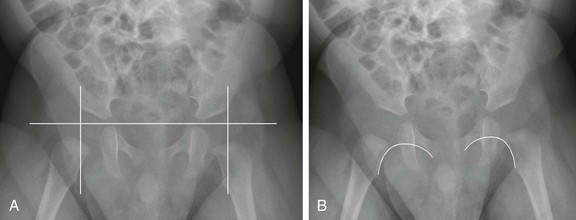
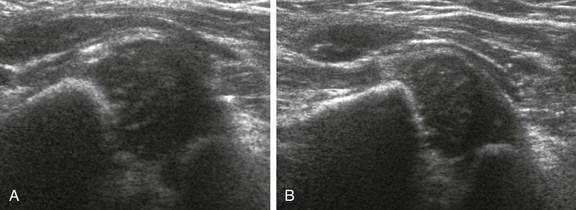
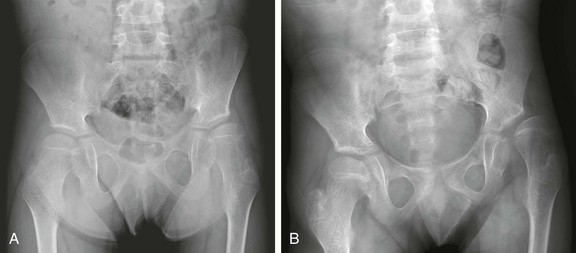
Chapter 136 Developmental dysplasia of the hip (DDH), formerly referred to as congenital dislocation of the hip, was first described thousands of years ago. Hippocrates is credited with ascribing intrauterine pressure as a possible etiology for this entity.1 This chapter covers the etiology, multimodality diagnostic imaging, and its implications in the treatment of DDH. Etiology: DDH is a spectrum that may vary from a normal congruent hip with normal appearing acetabula with ligamentous laxity, to a structurally abnormal hip with joint incongruity related to primary acetabular dysplasia. Usually, DDH is a result of a combination of both structural and ligamentous laxity leading to an abnormal incongruent hip. Ultimately, the precise underlying etiology of DDH is not known. Purported in utero developmental factors and fetal crowding may result in DDH. During week 7 of gestation, hip joint cleavage occurs.2 The lower extremity rotates medially during week 12 of gestation and hip muscles develop during week 18. However, it has been suggested that only 2% of cases result from intrauterine factors at this early phase of development and that the remaining 98% of cases are caused by changes to a normal hip during the last 4 weeks of pregnancy or in the immediate postnatal period.2 Postnatal factors are also hypothesized to have a role in DDH, including tight swaddling or the use of cradle boards that force the legs into extension and adduction. Epidemiology: Being the first born, breech birth, oligohydramnios, being large for gestational age, skull-molding deformities, female gender, and positive family history have all been associated with DDH. DDH is more common on the left.2 The theory of many of these factors relating to the cause of DDH reflects constricted in utero space. The uterus of a primiparous woman has less give. The hips are subjected to increased pressure and hyperflexion in breech presentations. With frank breech presentations, the risk is even greater. Decreased amniotic fluid or a large gestation also results in increased constriction. The most common fetal presentation is cephalic, with the fetal spine aligned to the mother’s left. This causes the left hip to be wedged against the maternal spine, which limits abduction and leads to a higher incidence of DDH on the left. Females are thought to be more affected because they are more sensitive to the circulating maternal hormone relaxin, resulting in ligamentous laxity.2 DDH is associated with myelodysplasia, arthrogryposis, multiple syndromes (such as Mobius and Poland syndromes), and chromosomal abnormalities. DDH is associated with talipes equinovarus or clubfoot, torticollis (fibromatosis colli, with a reported incidence of 5.5%), and congenital knee dislocation.3,4 The prevalence of DDH is reported up to 28.5 per 1000, depending on the population studied.5 Variation in rates may result from expertise of the examiners and inclusion of children with isolated ligamentous laxity. The incidence of DDH increases with family history: 6% chance with an affected sibling, 12% chance with one affected parent, 36% chance with both parents affected.2 During the first 2 weeks of life, physiologic instability exists, but it dissipates with increasing muscle tone and resolving ligamentous laxity as maternal hormones decrease. Natural History: If undiagnosed or left untreated, DDH may result in permanent acetabular dysplasia in children of walking age, typically having a shallow acetabular roof (sourcil) with anterior undercoverage related to increased acetabular version. Similarly, the femoral head may become secondarily dysplastic and lose its normal sphericity related to eccentric loads because of an incongruent hip, with resultant spherical growth plate disturbance and modeling changes.6 The femoral head must be seated within the acetabulum for normal development to occur. If the femoral head is dislocated, the transverse acetabular ligament and inferior capsular fibers become interpositioned, inhibiting hip congruity. Pulvinar (fibrofatty tissue) may also interpose between the femoral head and acetabulum, interfering with hip congruity. Hypertrophy of the fibrocartilaginous labrum often compensates for a shallow bony acetabular roof, and this has historically been referred to as a limbus.2 Long-term sequelae include incomplete coverage of the femoral head, excessive femoral anteversion, coxa valga, and coxa magna with muscle tightness (with the greatest impact on the adductors)7 (Fig. 136-1). As a result of these morphologic features, individuals with untreated DDH may develop premature degenerative changes of the hip joint and a permanent limp. Excessive femoral anteversion will lead to in-toeing. Hip degenerative changes are caused by loss of cartilage and labral tears secondary to abnormal eccentric joint contact pressure from chronic incongruent acetabular and femoral head articulation; rupture of the ligamentum teres has also been described.8 Degenerative changes caused by hip subluxation typically appear before women reach the age of 40 years and before men reach the age of 55 years; however, symptoms may become apparent during adolescence.2 With completely dislocated hips, many patients may function very well even into late adolescence with a neoacetabulum that forms along the iliac wing.2 Figure 136-1 Frontal radiographs of the pelvis demonstrating late presentation, and progression of developmental dysplasia of the hip of the left hip. Physical Examination: The physical examination to diagnose DDH consists of maneuvers described by Ortolani, a pediatrician, and by Barlow, an orthopedic surgeon. Ortolani described the hip click in 1937, although hip instability had been reported in 1879 and the clinical test described by Le Damany and Saiget in 1910.5 Barlow described his technique to demonstrate laxity of the dysplastic hip in 1961. In the Ortolani maneuver, forward pressure is applied to each femoral head with the infant in the supine position and the hips flexed to abduct the hip and to reduce a subluxated or dislocated femoral head. If subluxation or dislocation exists, an audible “clunk” is heard as the femoral head is reduced into the acetabulum. In the Barlow maneuver, backward pressure is applied to each femoral head with the in the infant supine position and the hips flexed to subluxate the hip.9–11 Both these maneuvers may fail to diagnose bilateral irreducible hip dislocations. Radiography: The infant’s lower extremities should be positioned in neutral extension with longitudinal symmetry. For symmetric imaging, the central ray should be directed above the pubic symphysis in the midline. In the presence of abnormality such as dislocation of the femoral head, a frog-leg view may be useful to evaluate reduction of the femoral head and may provide an opportunity for a second look at acetabular morphology. Positioning the thigh in abduction and internal rotation with a 45-degree angle (the von Rosen view) provides similar information as a frog-leg lateral view.12 Several lines may be drawn to assist in the assessment of hips, but attention should be made to the overall configuration rather than to the measured angles, which could have varying rates of interobserver and intraobservor variability. The Hilgenreiner line passes horizontally through the superior aspect of the triradiate cartilages. The Perkin line is the vertical line extending from the lateral margin of the acetabulum. The expected location of the femoral head is in the medial, inferior quadrant of the intersection of the Hilgenreiner and Perkin lines (Fig. 136-2, A). The Shenton line curves along the lesser trochanter, femoral neck, and inferior margin of the pubis or obturator foramen and should be smooth (Fig. 136-2, B) The acetabular index is the angle between the acetabulum (from the superolateral margin of the acetabulum and the superolateral margin of the triradiate cartilage) and the Hilgenreiner line. The acetabular index changes with age: 28 degrees in newborns, 23.5 degrees at age 6 months, 22 degrees at age 1 year, and 20 degrees at age 2 years. The maximal normal measurement for the acetabular index is 30 degrees up to age 4 months and 25 degrees up to age 2 years. The orientation of the pelvis on the radiograph impacts this measurement.13,14 In the preschool children and older children, the center edge angle may be calculated, and this measures the relative acetabular coverage of the femoral head. To determine the center edge angle, one line is drawn between the center of both femoral heads. Next, a vertical line is drawn 90 degrees at the center of the femoral head, and this serves as one reference line. Next, a line from the femoral head is drawn to the lateral acetabulum, and this serves as the second reference line. Now the center edge angle can be determined. This measurement is used in children over age 5 years. DDH should be suspected when the center edge angle is less than 19 degrees in children aged 6 to 13 years and less than 25 degrees in those over age 13 years.13,15 Radiographs are utilized to screen for DDH after age 4 to 6 months, when ultrasonography becomes more challenging and less reliable because of ossification of the femoral heads. Radiographic findings of DDH include an upward slanting sourcil, small capital femoral epiphysis, and superolateral subluxation of the femoral head (Figs. 136-3 and 136-4). Anteroposterior views are sufficient for screening. When abnormal, a frog-leg lateral view or a von Rosen view may be obtained to assess whether the femoral head reduces with hip abduction. When chronic, untreated DDH exists, the ipsilateral capital femoral epiphysis may become disproportionately smaller (Fig. 136-5). Without concentric apposition of two bones of a joint, as may occur with untreated DDH, epiphyseal ossification will be delayed. Figure 136-3 An anteroposterior radiograph in an 8-month-old girl demonstrates bilateral developmental dysplasia of the hip, with the left hip worse than the right hip. Ultrasonography: An orthopedic surgeon, Graf, described the use of ultrasonography in the assessment of the anatomy of the infant hip in 1980.16 Four years later, a group of radiologists including Harcke, described the dynamic technique to assessing infant hips.17 Ultrasonography has the advantages of absence of ionizing radiation, widespread availability, and the feasibility of a dynamic examination. The examination is typically performed with a linear array transducer using the highest frequency that provides adequate penetration (often 12 megahertz [MHz]). The transducer is placed over the lateral aspect of the hip in either the coronal plane, with the hip in neutral or flexed positions, or in the transverse or axial plane, with the hip in adduction or abduction (e-Fig. 136-6
Developmental Dysplasia of the Hip
A, At presentation, in this 11-year-old boy, the left hip is dysplastic, with an upsloping sourcil and mild undercoverage of the femoral head. The femoral head is already noted to be aspherically shaped. B, Three years later, progressive lateral uncovering of the femoral head and progressive secondary dysplastic changes of the femoral head are seen, and the greater trochanter overlies the femoral neck despite proper positioning, indicative of excessive femoral anteversion.

Note the upward slanting sourcil bilaterally. The right femoral head is concentrically located within its dysplastic acetabula. The left femoral head is superolaterally dislocated.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree