(1)
Department of X-Ray and MRI, RailWay Clinical Hospital, Yaroslavl, Russia
Abstract
Diverticulum (di + verto) in Latin means a way to the side, a branch, and to divert and refers to outpouchings in walls of hollow organs such as intestines or esophagus. The same term is used in respect of the caudal part of the mesonephric duct (wolffian duct) in embryos, which us an aniage of ureter and kidney pelvis.
1.1 Terms, Classification, and Statistics
Diverticulum (di + verto) in Latin means a way to the side, a branch, and to divert and refers to outpouchings in walls of hollow organs such as intestines or esophagus. The same term is used in respect of the caudal part of the mesonephric duct (Wolffian duct) of embryos, which were the beginning of the ureter and renal pelvis
Renal calyx diverticulum was first discovered during autopsy in 1841 [1]. RCD or medullocalyceal dystopia (after М. Rauer) represents a small calyx with a much more peripheral location than the rest. Diverticulum duct 2–4 mm long and 1 mm wide is sometimes connected with the minor renal calyx and sometimes with the major renal calyx or, which is a much rarer case, with the kidney pelvis.
Until 1978 terminology for isolated cystous formations in renal calyces and pelvis included a number of various controversial terms. The following terms were used as descriptions for this type of cysts: intrarenal cyst; peripelvic cyst; calyx cyst; calyx diverticulum; hydrocalyx; hydrocalycosis; pelvis diverticulum; pyelogenic cyst; pelvic cyst; pelvical, calyceal, pyelogenic, intramural cyst; localized obliterating pyelonephritis; calyx ectopia; etc. The most commonly used terms were calyceal cyst, hydrocalycosis, and pyelogenic cyst.
A. Ya. Pytel and A.G. Pugachyov (1977) specified that “…cystous formations are located near pelvicalyceal system of the kidney, are directly connected with it or have a continuous or intermittent connection. The cyst can be: (1) connected with the minor calyx thus forming its true diverticulum, due to which many call such a cyst calyceal diverticulum, (2) located more distal in respect of the location of a prelum or occlusion of the minor calyx neck resulting from cicatrical process” (see Figs. 1.1 and 1.2).
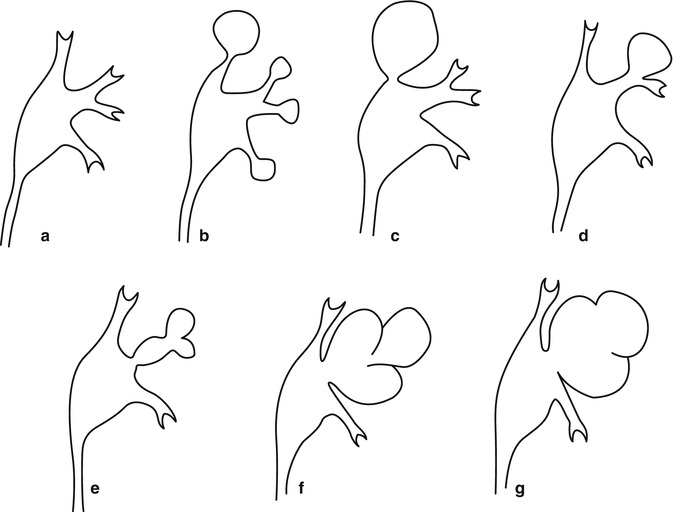
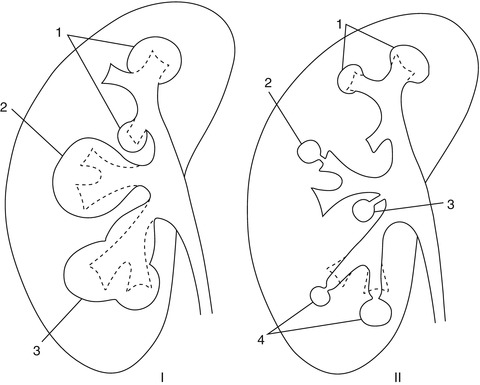
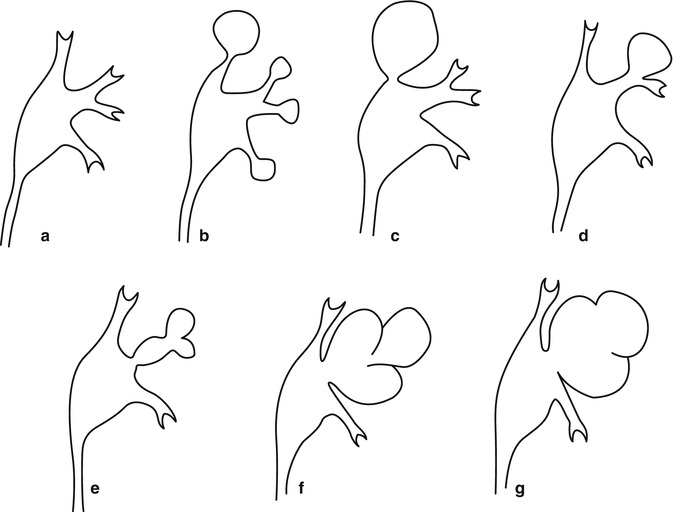
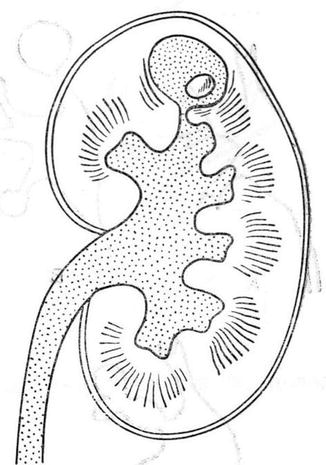
Fig. 1.1
Scheme of various arrangements of the calyceal cyst and hydronephrosis. (a) Norm; (b) hydrocalycosis of the forniceal and minor calyx; (c) hydrocalycosis of the major calyx; (d) hydrocalycosis of the minor calyx; (e–g) complex hydrocalycosis (After Pytel and Pugachyov [9])
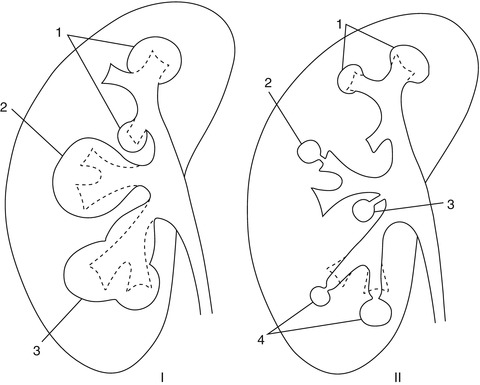
Fig. 1.2
Scheme of various types of hydrocalycosis and pyelogenic kidney cysts. (a) Various types of hydrocalycosis: 1 hydrocalyx of minor calyx; 2 hydrocalyx of major calyx; 3 diffuse hydrocalyx. (b) Various kinds of pyelogenic cysts: 1 forniceal hydrocalyx (Moore); 2 pyelogenic cyst connected by means of a duct with the minor calyx; 3 pyelogenic cyst connected by means of a duct with the kidney pelvis; 4 abnormality of the forniceal and calyceal area described by Dell’Adami and Borelli (After Pytel and Pytel (1966))
In 1978, calyx diverticulum was approved as the official term by the Second All-Union Conference of Urologists (Kiev), and it was classified as a congenital abnormality, (see Section Е for abnormalities of the pelvicalyceal system: (a) pelvis aplasia, (b) calyx diverticulum, (c) pelvis cyst [12–14]).
For the recent 20 years after the Second All-Union Conference of Urologists, as stated in the Urology Manual under the editorship of N.A. Lopatkin [15], a significant experience has been gained which required introduction of new doctrines into the existing classifications. However the proposed classification (1998), in our opinion, offers an unjustified reversion to the term calyceal and pelvic cysts which follows the term parapelvic cysts (move-after comma) instead of using the term calyx diverticulum. Such grouping has a wrong ground, since, as it is commonly known, parapelvic cysts come from lymph tubes of kidney hilum and are not connected with the pelvicalyceal system, while calyx diverticulum comes from the primary arteries. In addition, the term calyx diverticulum has been prevailing in foreign literature and many sources of domestic literature during recent years. An interesting fact is that unlike the terms ureteral diverticulum, bladder diverticulum, and urethral diverticulum, which are commonly accepted and almost have no synonyms, the terms calyx diverticulum and pelvis diverticulum have got more and more commonly used only for the recent 10–15 years.
In some sources calyx diverticulum is called Prater syndrome (www.chelmed.ru/library/p.htm).
Up to 1955, 101 patients with calyx diverticulum had been described in the world literature.
By 1963 B. Abeshouse and G. Abeshouse had collected data about 318 clinical and 11 autopsy calyx diverticulum cases [4, 5].
By 1985 the world data had enhanced to 400 observations in 370 patients, including 103 calyx diverticula in 96 patients in domestic literature reported by V.M. Perelman and V.M. Builov [22].
At the same time by 1977, A.Ya. Pytel and A.G. Pugachyov had found descriptions of more than 800 cases of calyx diverticulum in the world literature [9].
Calyx diverticulum detection rate is the same in men and women and is 2.1–4.4 of 1,000 excretory urographies [8, 9]. In accordance with data by Middleton and Pfister (1974), pyelocalyceal cysts (calyx diverticula) are detected in 0.2 % cases in excretory urograms (quoted after A. Ya. Pytel, A. G. Pugachyov 1977, p. 74). Calyx diverticulum is found in children in 3 % of cases and in adults in 2.1–4.4 % of cases out of 1,000 excretory urograms examined (Wulfsohn M.A. 1980). In accordance with the data by V.M. Perelman and V. M. Builov [22], who published the first and the largest report in the domestic literature (52 patients with 53 diverticula detected), calyx diverticulum was discovered in 0.05 % of cases out of 12,000 excretory urograms.
Bilateral localization of calyx diverticula is found in 3 % of cases. Most often calyx diverticulum is unilateral. Calyx diverticulum is found two times more often in the right kidney than in the left one. Solitary calyx diverticulum occurs in 92 % of cases. Calyx diverticulum is found in an upper calyx in 67 % of cases, in a lower calyx in 20 % of cases, and in a middle calyx in 13 % of cases. Calyx diverticulum contains straw-colored liquid with urinary salts. It can be combined with some other renal abnormalities [9].
At the end of the past century and the beginning of the current century, the frequency of reporting of diagnostics and treatment of calyx diverticulum has increased significantly, and this abnormality of kidney structure can no longer be considered rare.
1.2 Etiology and Pathogenesis
Two anatomical forms of calyx diverticulum are known. In the outermost kidney segments, most often in the upper ones, small diverticula are formed with the diameter of 0.1 cm to several centimeters which are connected with the minor calyces. In the middle segment of the kidney, larger diverticula are found which are connected with the kidney pelvis or the middle calyx. Diverticulum cavity is covered with a secretory transitional cell epithelium; its walls may also contain muscular elements. Calyx diverticula are connected with the pelvicalyceal system by means of a narrow and short duct. Calyx diverticula appear on the 5–6th week of embryonal development when primary kidney artery spread branches toward the kidneys. Thus the main role in their etiology is assigned to local abnormalities of the renal artery formation. Abnormality of the arterial blood supply to kidneys is usually combined with reduction of collecting tubes leading to calyces of the forth order, which lose their ability to morphogenesis and expand under the pressure of urine [3–5]. During embryogenesis of the pelvicalyceal system, branches of the ureteral sprout normally degenerate and gradually disappear within the period of minor calyx fragmentation. In case this does not happen and one or several branches of minor calyces of the third or fourth order are preserved and then calyx diverticulum develops [9]. Among other congenital abnormalities, along with hydronephrosis and absence or hypoplasia of the right kidney, the literature contains references also to calyx cysts or diverticula as often accompanying inborn alcohol syndrome (http://history.km.ru/vsiachina/alconavt.htm).
Some authors consider the possibility of acquired calyx diverticulum development. This happens when a small parenchyma abscess empties into the pelvicalyceal system, as a result of pyelotubular reflux and inflammatory stenosis of the minor calyx neck, as well as during hydrocalycoses caused by narrowing and even obliteration of the calyceal necks [6, 7]. According to A. Ya. Pytel and S.D. Goligorsky [3], a significant role in calyceal cyst and hydrocalycosis formation belongs to concomitant pedunculitis. When this condition is present, a tension of the abnormal vessel takes place which causes aggravation of loop occlusion of the calyceal neck; thus a calyceal cyst may appear due to constriction of the calyx neck with the abnormal intrarenal vessel, which is observed, for example, in case of Fraley syndrome [28, 29] (Fig. 1.3).
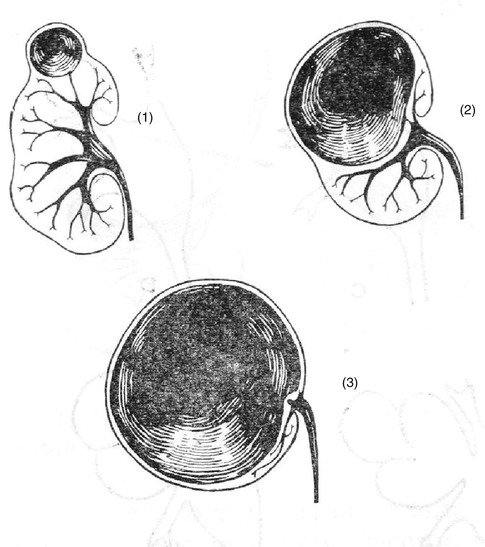
Fig. 1.3
Fraley syndrome, a vascular abnormality when arterial brunch is constricting the upper calyx neck which causes calyx cyst development (After Pytel and Pugachyov [9])
As well as A. Ya. Pytel and A. G. Pugachyov [9], we believe that the classification of this situation as calyx diverticulum is rather conventional, and it would be more logical and correct to address the development of obstruction in the area of the upper calyx neck as formation of local hydrocalycosis.
1.3 Clinical Diagnostics
In most cases clinical presentation is absent or defined by accompanying complications such as lithogenesis, inflammation, or spontaneous rupture [10–15].
Often an inflammatory process occurs in calyx diverticulum and an acute or chronic pyelonephritis, and in 38 % of cases stone formation takes place (Fig. 1.4).
The number of stones is usually not large (2–10) and they have a small size. There are described cases when up to 2,000 sand grains were found in the cyst (P. Rudstroem 1949—quoted after A. Ya. Pytel and A.G. Pugachyov 1977, p. 75).
When calyx diverticulum is infected or lithogenesis is in process inside it (Fig. 1.4), patients may suffer from dull pain in the lumbar region and sometimes from renal colic bouts. In accordance with the data by A. Ya. Pytel and A. G. Pugachyov [9], 15 % of patients have macrohematuria and 1/3 of patients have obstinate leukocyturia which is resistant to drug therapy. Cases of arterial hypertension are known among patients with calyx diverticulum which was complicated with pyelonephritis.
Upon examination of an overall radiogram of the urinary system, it can be seen that if radiopositive concrements are present in the calyx diverticulum cavity, they are usually located closer to the kidney cortex and may have faceted, polished outlines similar to structure of stones in the gall bladder (Fig. 1.22). If stones in the calyx cyst cavity are low in contrast or radionegative, USG and CAT can be helpful in their detection (Fig. 1.24).
Sometimes in the calyx diverticulum, cavity milk of calcium renal stone is found which is a mass of finest grains. Such a configuration is called calcium milk in the literature and is created by filling the calyx diverticulum cavity with a subtle colloidal fine suspension of calcium carbonate, calcium phosphate, calcium carbonate or oxalate, or calcium carbonate and triphosphate [38–41, 43]. Detection of this phenomenon, which produces no clinical presentations, is very important since it is often mistaken for a concrement in a calyx; thus remote lithotripsy and other respective therapies are used which are absolutely ineffective in this situation.
Some authors specify that calyx diverticulum can be caused by vesicoureteral reflux (Amar A.D. 1975) [27]. Among 32 children with calyx diverticulum, 23 were diagnosed with VUR. Calyx diverticula were different in sizes and were located in various kidney segments. In the opinion of Amar A.D. (1975), calyceal cysts development is to a great extent due to inflammatory process; 2/3 of young patients observed by him had signs of pyelonephritis. Thus when children are diagnosed with calyx diverticulum, they must also be examined to exclude VUR.
1.4 Ultrasound Diagnostics
As noted by A. N. Hitrova, V. V. Mitkov, and M. D. Mitkova, “Calyx or pelvis diverticula, pyelogenic cysts are almost never detected by ultrasonography” [44]. However, our experience proves that it is applicable only to small calyceal diverticula with the diameter less than 0.5 cm (Fig. 1.12) and does not refer to large calyceal diverticula (Figs. 1.13 and 1.16).
Ultrasound signs of calyx diverticulum, which were first described by us in 1993 [45–47], include:
1.
Echo-free rounded structure with smooth outline which is located to the distal side of the calyceal fornix or the pelvis outline and is connected with them by means of a narrow passage.
2.
The diameter of the structure is several mm to several cm.
3.
In the case of calcium milk phenomenon, a combination of echo-free and echo-producing structures is detected in the cavity of diverticulum with a horizontal level which is moving during multiple-view scanning.
In the recent years, the so-called twinking artifactwas described which had been observed at ultrasound dopplerography (USDG) of stones and calcium milk in the calyx diverticulum cavity which is detected in 91 % of patients. It represents hyperechoiс structures with reverberation effect in the kidney parenchyma or a chaotic sequence of colored signals in the view of the stone or calcium milk, as well as along the acoustic shadow in the modes of color and energy Doppler mapping. At multiple views, USG and CAT scanning these structures demonstrate “gravity dependence of location of dense structures in the liquid formation” [48] (Figs. 1.5 and 1.21). Such a phenomenon, in our opinion, is similar to the so-called rattlebag syndrome described in radiological pulmonology when upon the patient’s changing posture shifting of mycelium resulting from mycotic lesion of the sanitized lung cavities is discovered [44] (Fig. 1.5).
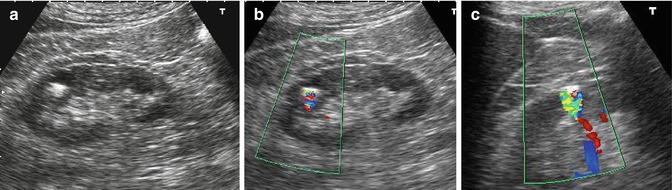
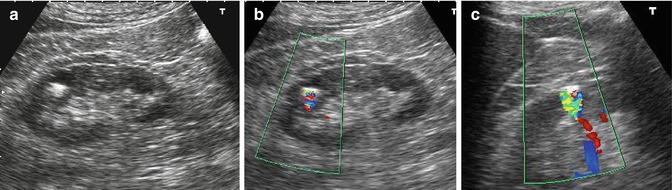
Fig. 1.5
Small diverticulum in an upper calyx of the right kidney with calcium milk symptom in sonograms and a color Doppler mapping image: (a, b) a small cavity with an echo-free and an echo-producing component separated with level line which shifts at turning in a sonogram of patient lying on the right side; (c) twinking artifact at color Doppler mapping (Observation by Gromov (2005), with author’s permission)
Pharmacosonography is a method which allows one to carry out differential diagnostics of liquid formations related to the pelvicalyceal system as well as of parapelvic cysts suggested by A. V. Amosov and G. M. Imnaishvilli in 1988 [50]. This method implies USG detection of expansion or absence of expansion of liquid formations against injection or intake of diuretics (Lasix (furosemide), bufenox). Thus expansion of a liquid formation proves its connection with the pelvicalyceal system (calyco-pyelectasis), while the absence of expansion may mean a parapelvic cyst or an intrarenal cyst [50, 51].
In the process of diagnostic differentiation of calyx diverticulum and isolated hydrocalycosis, a pharmacosonographic test reveals expansion of the ectatic calyx as opposed to the absence of expansion in a liquid formation resulting from calyx diverticulum, which cavity has a stable size during the test and becomes more intensive in delayed sonograms due to its retrograde opacification.
At the same time, it should be kept in mind that expansion of the liquid formation may be also absent due to pronounced expansion of the pelvicalyceal system when the reserve of the upper urinary tract has been spent (Fig. 1.6a–c).
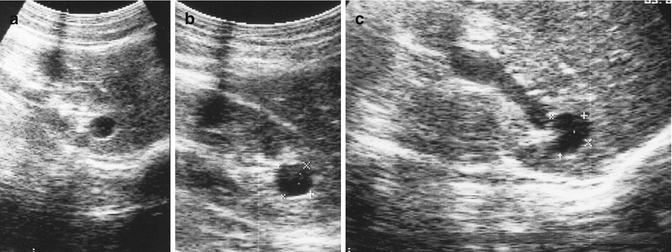
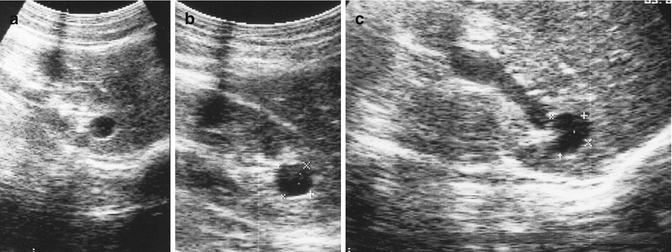
Fig. 1.6
(a–c) Pharmacosonography in case of diverticulum in an upper calyx of the right kidney (expansion of pelvis while expansion of calyx diverticulum is absent)
1.5 X-Ray Diagnostics
The main method for calyx diverticulum diagnostics is excretory urography (EU), which, especially when combined with cineradiography and making multiple-view compression spot films, allows to obtain data on the length and width of calyx diverticulum neck as well as on other anatomical details.
In case kidney function is satisfactory, we believe that for the purpose of performing EU and investigation of the urographic phase during CAT with contrast enhancement, it is necessary to try to use nonionic contrast media for the majority of patients, such as nonionic monomers—Ultravist, Omnipaque 300, or Visipaque and others in the dose of 1.0 ml per kilo of body weight with the highest possible speed of intravenous injection. We deem that nonionic contrast preparations such as Ultravist, Omnipaque 300, and others and the only isoosmolar to blood nonionic dimeric contrast preparation Visipaque are the only option to use in all patients of the risk group (anamnesis including nephratopy, allergic reactions, diabetic nephropathy, congestive heart failure, use of nephrotoxic medications such as nonsteroidal anti-inflammatory drugs) In our opinion, usage of relatively less expensive 76 % intravenous ionic solutions of Hypaque or urographine must be limited as much as possible due to a much lower tolerance and higher rate and intensity of side reactions and complications. At the same time it should be kept in mind that in spite of a great progress in development of contrast preparations, even the newest of them require the medical personnel to know their usage procedures as well as possible reactions and complications, preventive measures, and treatment. All these issues are highlighted in the Contrast Media Guidelines developed by the European Society of Urogenital Radiology (ESUR) (see Supplement).
In excretory urograms, usually a small rounded shadow can be seen to the lateral side of the fornix of the minor calyx which is connected with the calyx by a small narrow channel. In urograms made later, the degree of contrast of calyx diverticulum cavity is increasing with emptying which in turn results in decrease of contrast intensity of pelvicalyceal systems (Fig. 1.18).
The survey radiograph looks specific in case there are so-called milk of calcium renal stones in the calyx diverticulum cavity (Garrett and Holland 1973). When calcium milk phenomenon is present, as it was mentioned above, the calyx diverticulum cavity is filled with a subtle colloidal fine suspension of calcium carbonate, calcium phosphate, calcium carbonate or oxalate, or calcium carbonate, and triphosphate [40–44]. Then an intensive boundary is defined in the X-ray image which shifts to the horizontal level when the patient turns (Figs. 1.26, 1.27, 1.28, 1.29, 1.30, 1.31, and 1.32).
In case of calyx diverticulum, it is recommended to have USG and EU tests with images taken in 1 and 3 h. From our point of view, a delayed image taken in the 30–45th min is enough, which depends on the calyx diverticulum size, the most common size being from several millimeters to several centimeters [41].
As can be concluded, calyx diverticulum has the following radiographic features:
1.
A rounded cavity with smooth sharp outlines which is located to the distal side of the calyceal fornix or pelvis outline and is connected with them by a narrow passage which is often not visible in excretory urograms.
2.
Calyx diverticulum cavity is several millimeters to several centimeters in diameter:– Calyx diverticulum contrast intensity increases in urograms made later, as opposed to decrease in pelvicalyceal system contrast intensity in delayed images.
3.
Absence of motor activity of diverticulum walls as opposed to the walls of pelvicalyceal system which are detected by means of excretory cineradiographic calyceal-pelvic-ureteroscopy.
Spiral computed tomography and multislice computer tomography (SCT and MSCT) with image reconstruction in the urographic phase (SCTU) which appeared in the recent years allow to clarify calyx diverticulum anatomic details and define the density of concrements in accordance with the Hounsfield scale. This is especially important for choosing a method of treatment: remote lithotripsy (RL), endoscopic surgery with contact lithotripsy (CL), or conventional open surgery [21–29].
Thus application of USG and X-ray technique helps to obtain comprehensive information on the calyx diverticulum, its neck, presence of calcium milk, or a concrement in its cavity which is the principal factor in selection of a treatment method.
1.6 Magnetic Resonance Diagnostics (Magnetic Resonance Imaging and Urography)
The main method of upper urinary tract investigation along the whole of its length until the mid-1980s was X-ray technique with intravenous or retro- and antegrade introduction of iodinated contrast agent. The first reports on a possibility of making images of the upper urinary tract without introduction of iodinated contrast media at MRI, the so-called magnetic resonance urography method, using T2-weighted images in the frontal projection and the mode of suppression of signals from fat appeared in 1986 (Henning J. et al.). In our country, the first reference to clinical usage of MRU was made by Yu. N. Belenkov, O. I. Belichenko, V. E. Sinitsin, and M. Ch. Tavzadze [58, 59]. Invention of MRU technology is compared by many authors with invention of EU in respect of its significance for diagnostics of urological diseases. Apart from the possibility to visualize the upper urinary tract while avoiding introduction of contrast media and exposure of patients to radiation, MRU has become the first method which allowed to implement a 3D reconstruction of an image, rotation of an image in any plane with selection of the best projection, as well as the function of virtual endoscopy of the upper urinary tract [60].
MRU method principle is the following: When MRI is being carried out in the hydrographic mode, a highly intensive MR signal is registered which comes from stationary or quasi-stationary liquid located in natural or pathological structures against the background of a much less intensive signal from surrounding organs and tissues. This helps to obtain sharp images of urinary tract, especially in case it is expanded. In order to improve images, especially those of unexpanded urinary tract and smaller calyx diverticula, methods based on using loop diuretics were suggested (Lasix (furosemide)). They are introduced parenterally prior to MRU, which provide a quick diuretic effect and causes expansion of pelvicalyceal systems and ureters which improves their visualization. In addition to intravenous introduction of furosemide, also external compression of ureters was suggested. However for the best visualization of urinary tract, introduction of paramagnetic contrast materials is required, including cases of combination with diuretic load [59–63] (Figs. 1.7, 1.8, and 1.9).
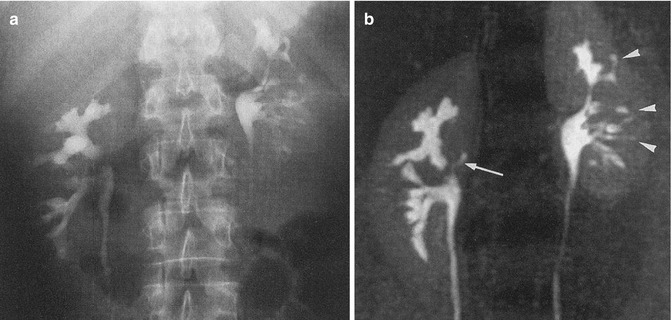
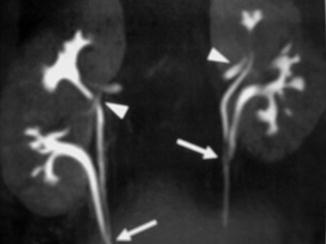
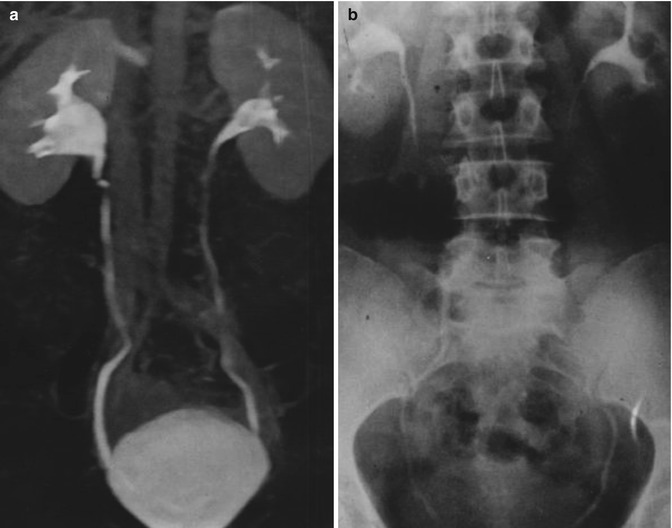
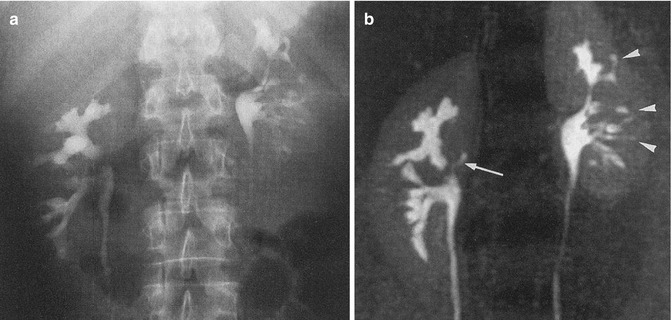
Fig. 1.7
(a) A small diverticulum in the right kidney pelvis cannot be seen in the excretory urogram; (b) the same diverticulum diverticula (arrow-in the right and arrow-head in the left kidneys) can be well distinguished in the magnetic resonance urogram (Nolte-Ernsting et al. [59])
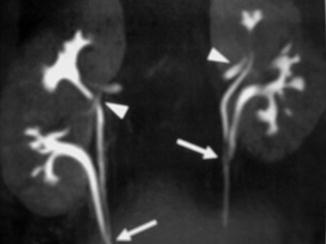
Fig. 1.8
Small diverticula (triangles) of upper halves of doubled pelvicalyceal systems of kidneys (arrows) in magnetic resonance urograms (Nolte-Erusting et al. [60])
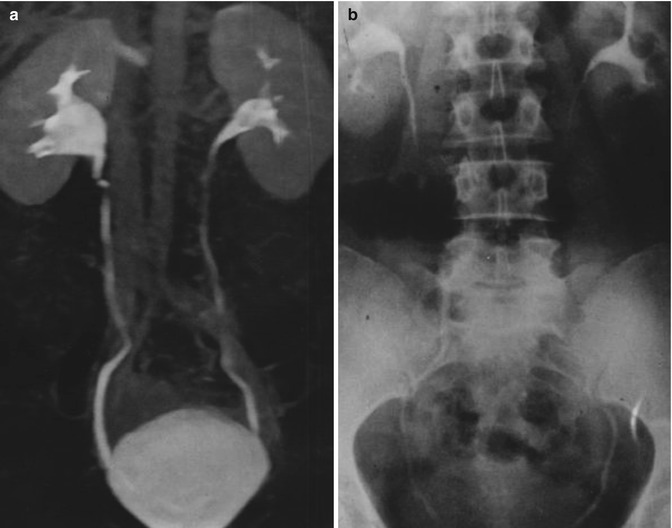
Fig. 1.9
Results of MRU with contrast enhancement (a) and of intravenous urography (b) done on a 43-year-old kidney donor. Unlike conventional urography, MRU allows to visualize outlines of a normal kidney parenchyma and condition of the upper urinary tract along the whole of its length (El-Diasty et al. [63])
Thus MRU is becoming the most perspective method for examination of the upper urinary tract, especially in children and in those cases when usage of roentgenocontrast preparations for EU is not possible or not recommended. The only drawback of MRU, which is, unfortunately, significant and difficult to overcome in many countries, is the high cost of magnetic resonance imaging units and paramagnetic contrast media. In major works issued in Russia by V.I. Dombrovsky [57] and Yu. G. Alyaev, V.E. Sinitsyn, and N. A. Grigoriev (2005) which are devoted to MRI in urology, their high efficiency and superiority over other kinds of diagnostics is highlighted. At the same time it is specified that these systems are still rather few; that is why “MRI usually serves as “second-tier” diagnostics to clarify data from preceding tests.” Thanks to implementation of the health investment program, the number of MRI systems has been constantly growing in our country during the recent years; therefore 2010 algorithm in urological radiology is optimal in our opinion, provided modern modifications of USG and MRI are used. The latter, which used to be a “second-tier” diagnostic method [56], considering data from “targeted” USG, will be shifting and has already started to shift to the “first tier” as technical abilities emerge [97].
1.7 Differential Diagnostics
Calyx diverticulum must be differentiated from congenital abnormalities of calyces, namely, tubulomedullar dilatation and medullar hypoplasia or megacalycosis, as well as with isolated hydrocalycosis and tuberculous caverna.
Tubulomedullar dilatation is the expansion of one or more outlet tubules in the renal pyramid. This kind of abnormality can be observed in one, two, and even in all kidney pyramids. Radiographically it appears as a spindle-shaped expansion located in a renal papilla or sometimes a thin duct between the spin-shaped expansion and the calyx opening at the top of the pyramid. This kind of X-ray visual structure can be easily mistaken for papilla necrosis. However, Yu. A. Pytel and I. I. Zolotaryov (1974, 1987) emphasize that in the case of tubulomedullar dilatation, the papilla and fornix stay unchanged. Moreover, image of the expanded tubule as contrasted urine accumulates in it emerges only in an excretory urogram [26, 64].
Medullar hypoplasia (megacalycosis) is an embryonic defect of medullary substance which appears in calyx expansion due to underdevelopment of the final kidney. In case of megacalycosis, pyramids lose their usual shape. Vacant space is left which is overtaken by the minor calyx separated from the cortex only with a thin layer of the underdeveloped pyramid. In excretory urograms, contrast media appears both in the kidney with megacalycosis and in the contralateral kidney at the same time. An abundance of enlarged calyces of triangle or faceted shape is detected which are located in the thickness of kidney parenchyma with their top toward the pelvis. Capacity of expanded calyces exceeds that of pelvis and they are filled slowly. The pelvis is not expanded. Urine drainage is not hindered. Urodynamics of the upper urinary tract is undisturbed. The main difference between calyx diverticulum and megacalycosis lies in its development—it usually appears in one calyx and is much less common in two calyces, unlike megacalycosis which affects all calyces. When it comes to differential diagnostics of calyx diverticula, which are generally found in one or, in very rare cases, in two calyces, and megacalycosis, the latter abnormality, as it follows from its name, can be only multiple on one and on both sides [68–70] (Fig. 1.36).
Calyx diverticulum is often mistaken for isolated hydrocalycosis, a much more commonly occurring condition resulting from calyx neck blockade and diminution due to various congenital and acquired processes. According to congenital hydrocalycosis sizes can have several degrees from the 1st degree, small upper calyx diverticulum; to the 2nd, when calyx diverticulum cavity can occupy up to 2/3 of the kidney volume; and to the 3rd, when calyx diverticulum cavity can occupy the whole kidney(Fig. 1.10).
Many authors emphasize the necessity to ensure differential diagnostics of isolated hydrocalycosis and calyx diverticulum [66, 67]. Ultrasound technique has a low practical efficiency in differential diagnostics of isolated hydrocalycosis and calyx diverticulum. At the same time a series of multiple-view spot excretory urograms as well as cineradiographic visualization allow to clearly observe the stable triangle shape of dilated calyx differentiating it from calyx diverticulum which has a rounded shape. Also a short oblique filling defect is discovered caused by compression from an accessory vessel varying in intensity which changes in width depending on the pelvicalyceal system filling, accessory vessel engorgement, and intra-abdominal pressure (Fig. 1.33).
We did not discover functional lability of diverticulum walls by investigation of urodynamics of pelvicalyceal system and of calyx diverticulum area performed by means of cineradiographic visualization [22]. The same result was obtained by [33, 74] as opposed to V. D. Grund and B. N. Voskresensky [73]. Filling of diverticulum cavity with contrast media was progressing slowly; it flew in from the pelvicalyceal system at different times depending on the length, diameter, and patency of the connecting duct. Small calyceal diverticula were filled almost simultaneously with the whole pelvicalyceal system; the larger ones got opacified later and were better distinguished in delayed urograms.
Absence of motor activity in calyx diverticulum walls may be explained by the presence of a fibrous capsule around the diverticulum [74] as well as by its location in the depth of the kidney which is a parenchymal organ, unlike alimentary tract diverticula as alimentary tract consists of hollow organs with walls capable of motor activity. This may also explain the absence of enlargement of calyx diverticulum as opposed to hydrocalycosis during a pharmacosonographic test with diuretics.
If contractions are observed during differential diagnostics of calyx diverticulum and isolated hydrocalycosis, this observation confirms the latter. Moreover, ectatic calyx does not have a strictly round shape, and in multiple-view scans, it almost always preserves a triangle shape (Fig. 1.34).
In case of congenital isolated hydrocalycosis, the triangle shape of the calyx is also maintained and usually an abnormal structure of the whole pelvicalyceal system is observed (Figs. 1.35, 1.36, and 1.37). On the contrary, in case of calyx diverticulum, pelvicalyceal system structure is normal.
Radiographic features of calyx diverticulum and of calyx hydrocalycosis are summarized in Table 1.1.
Table 1.1
Radiographic features of calyx diverticulum and of calyx hydrocalycosis
Calyx diverticulum | Calyx hydrocalycosis |
|---|---|
Most often a rounded single cavity located to the distal side of the fornix usually of an upper calyx with smooth sharp outlines | The shape of the cavity repeating the initial triangle shape of the calyx persists for a long time as far as the most intensive stages |
If multiple stones are present, they are grouped in the same way as multiple polished roentgenocontrast stones inside the gall bladder | Generally solitary and repeating the shape of the calyx |
A short duct connecting calyx or pelvis with diverticulum which is not always visible < div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|