Chapter 98 Phonation and coordinated movement of liquid and food are the result of complex, integrated, and intact neuromuscular function. When a person’s swallowing function is abnormal because of a structural anomaly, neuromuscular deficit, or postsurgical change, a swallowing function study can be performed. Most swallowing disorders in infants and children are a result of neurologic abnormalities, of which cerebral palsy is the most common.1,2 The initial step in the swallowing evaluation is to assess the competence of the velopharyngeal mechanism. First, the patient is observed during quiet breathing and phonation. During feeding, the patient is placed in the true lateral position and is fed contrast material of varying thickness with a bottle with a nipple initially, while swallowing is evaluated in real time with video fluoroscopy, including examination from the mouth to the carina. Either a single image or a sweeping image down to the carina and back to the mouth may be obtained.3–6 Imaging in the frontal projection using a basal or Towne view6 may be performed after lateral imaging; this view permits evaluation of lateral wall movement and correlation with nasopharyngoscopy (e-Fig. 98-1).3,7 If the infant will not take contrast material from the nipple, the contrast material can be introduced into the baby’s mouth carefully with a blunt-tipped syringe (between the cheek and the lateral aspect of the teeth or gums), or a feeding tube can be inserted through the nipple into the baby’s mouth and contrast material can be introduced in a controlled manner under fluoroscopic guidance to initiate swallowing (e-Fig. 98-2). The contrast medium is mixed with increasingly thicker food mixtures, beginning with thin liquids and progressing to solid food if such food is age appropriate. Evaluation of the patient’s ability to handle food with different textures aids in planning an appropriate diet to meet nutritional needs and in planning future therapy. If the patient requires a special diet or only eats certain foods, this food can be brought to the examination and used for the study. e-Figure 98-2 Modified feeding technique. Overview: Cerebral palsy is the most common cause of swallowing dysfunction in infants and children. Other neuromuscular disorders are brainstem dysfunction, cranial nerve abnormalities, intracranial neoplasms, meningomyelocele, muscular dystrophies, and myasthenia gravis. Familial dysautonomia (Riley-Day syndrome) leads to autonomic dysfunction with esophageal dysmotility and frequent aspiration pneumonias. Abnormality of the neuromuscular mechanism elevating the soft palate may lead to reflux of contrast material into the nasopharynx, with subsequent pooling of contrast in the pharynx and potential airway aspiration. Abnormalities of other muscle groups lead to defective function of the epiglottis and upper esophageal sphincter, with aspiration into the airway being common1 (Fig. 98-3; Videos 98-1 and 98-2). Figure 98-3 Swallowing. Etiology: Swallowing dysfunction is related to dysfunction in one or more of the three phases of swallowing: the oral phase, with the inability to deliver food into the mouth (e.g., poor suck); the pharyngeal phase, with failure to move the food through the pharynx, elevate the soft palate, and close the epiglottis; and/or the upper esophageal phase, with abnormal coordination of relaxation and contraction of the upper esophageal sphincter.1 Swallowing coordination is mediated through the cranial nerves responsible for both sensation and motor function, as well as osseous and muscular structures supplied by both the autonomic and voluntary nervous system. Thus swallowing dysfunction may be due to a large number of conditions that affect any of the mechanical and functional processes necessary for normal swallowing and phonation. Clinical Presentation: The severity of disordered swallowing and the resultant degree of aspiration will vary with the level of neurologic deficit. Depending on the specific neurologic defect, any or all components of the swallowing mechanism may be affected. Symptoms include nasopharyngeal regurgitation, gagging, coughing and choking during feedings, recurrent pneumonia, malnutrition, and failure to thrive.1,8
Disorders of Swallowing
General Examination Principles
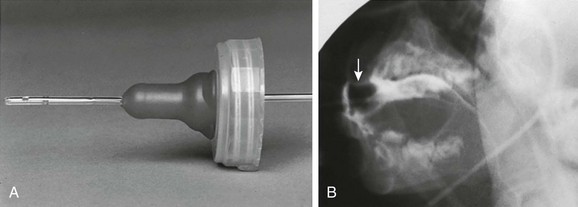
A, A number 8 Silastic feeding tube is placed through a nipple so that contrast material can be introduced into the mouth in a controlled manner as the swallowing mechanism is observed. B, Barium outlines the nipple (arrow) and the tube. (Modified from Poznanski A. A simple device for administering barium to infants. Radiology. 1969;93:1106.)
Causes of Swallowing Dysfunction
Central Neurologic Dysfunction
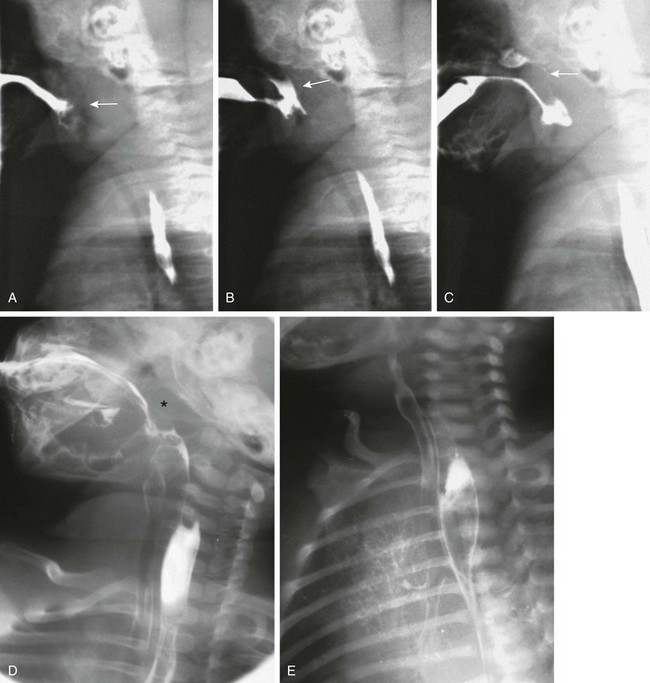
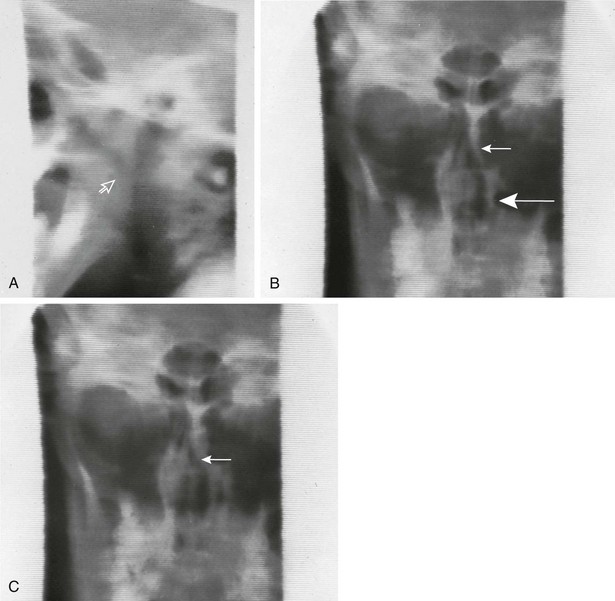
A, As the nipple is inserted into the infant’s mouth, the tongue and soft palate are relaxed and the nasopharynx opens (arrow). B, Normally, the tongue elevates, pushing the nipple to the roof of the mouth, and the soft palate elevates. In this example, the soft palate did not elevate and close off the nasopharynx, resulting in nasopharyngeal reflux (arrow). C, The infant finally did close the nasopharynx by elevation of the soft palate against the adenoid tissue (arrow). Contrast material remains in the nose and in the hypopharynx. D, During this barium swallow study, complete closure of the nasopharynx occurs and no nasopharyngeal reflux is present (asterisk), but aspiration of contrast into the larynx and trachea occurs. E, An oblique view in the same patient as shown in part D reveals extensive airway aspiration during a routine barium swallow study as a result of a lack of coordination during swallowing. Barium coating of the lung parenchyma is present.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree