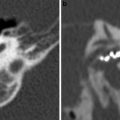
Fig. 1
9-year-old child showing microtia on left side. a, b Coronal CT-images. The right external auditory canal appears normal, while on the left side it is narrowed and has a steeper slope (asterisks). c, d Axial images. Normally developed middle ear cavity on right side. On the left side, the epitympanon is very small, only containing the head of the malleus (arrow). The incus and stapedial superstructure are absent on the left side, while the left footplate (arrowhead) is well developed, although somewhat turned towards the coronal plane compared to the right side. The left mastoid is not pneumatized. The inner ear structures appeared normal on both sides
When no external auditory canal is formed, the tympanic bone is aplastic. The lateral wall of the middle ear consists of soft tissue (Fig. 2), or a bony plate which is situated at the expected level of the tympanic membrane (Fig. 3). Such a bony plate is called an atresia plate, and this may correspond to a ‘frust’ tympanic bone or to downward extension of the squamous part of the temporal bone, meeting the floor of the middle ear.
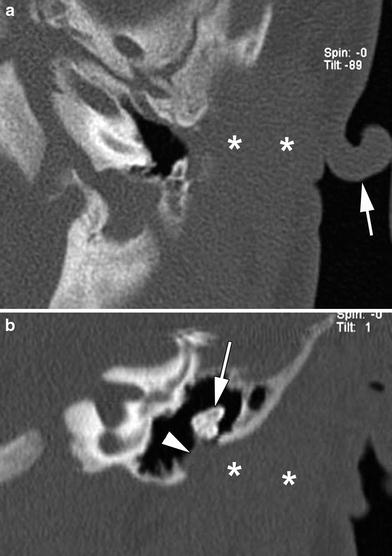
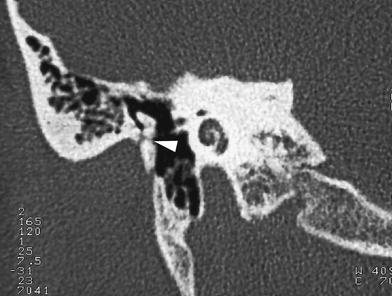
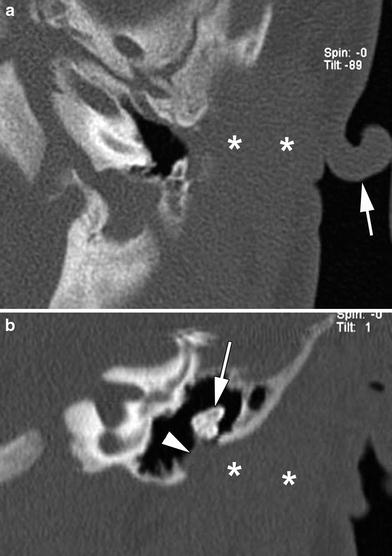
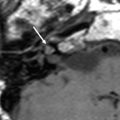
Fig. 2
Axial and coronal CT-image of left temporal bone in a neonatus. Abnormal auricle (arrow, a) The external ear canal is absent: only soft tissue is seen (asterisks). The lateral wall of the middle ear consists of soft tissue (arrowhead, b) no tympanic membrane is identified. The malleus and incus appear deformed and fused (arrow, b)
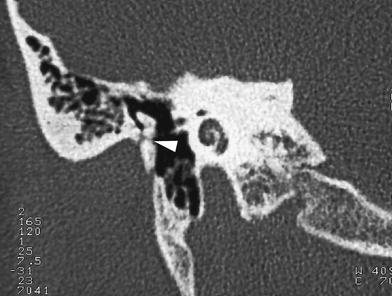
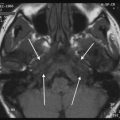
Fig. 3
Coronal CT image through right temporal bone in an adult patient. Atresia of the external auditory canal. The neck of the malleus is fused with the atresia plate (arrowhead)
The size of the tympanic cavity is often diminished, making surgery more difficult. The tegmen may have a low position, which may also complicate the surgical approach. The air content of the mastoid is often reduced, correlating with the degree of abnormality of the external ear.
The size of the bony Eustachian tube may be reduced, but sometimes this structure appears enlarged (Mayer et al. 1998).
Ossicular chain abnormalities are very frequently associated with aural dysplasia. Aplasia of the tympanic bone is associated with fusion of the neck of the malleus to the lateral epitympanic wall or atresia plate (Figs. 2 and 3). In addition, other ossicular anomalies may be present: fusion of the malleus and incus, with absence of the normal malleoincudal joint, is common, and the long process of the incus may have an abnormal orientation or be hypoplastic or absent. The most important ossicular structure to look for on CT is the stapes; absence of the stapes makes surgical reconstruction more complex. Furthermore, the presence and width of the oval window should be checked; on coronal images, it should have a diameter of about 2 mm (Yeakley and Jahrsdoerfer 1996).
The tympanic segment of the facial nerve canal is often displaced caudally, sometimes reaching as low as the round window (Mayer et al. 1998). The second genu and mastoid portion of the facial nerve typically are more anteriorly positioned than normal, which is important for the surgeon to know, as this may severely hinder surgical reconstruction. The mastoid portion of the facial nerve may curve anteriorly toward the area of the temporomandibular joint, or leave the temporal bone in a more lateral direction. Determining the exact course of the facial nerve is of utmost importance to avoid postoperative facial paralysis (Fig. 4).
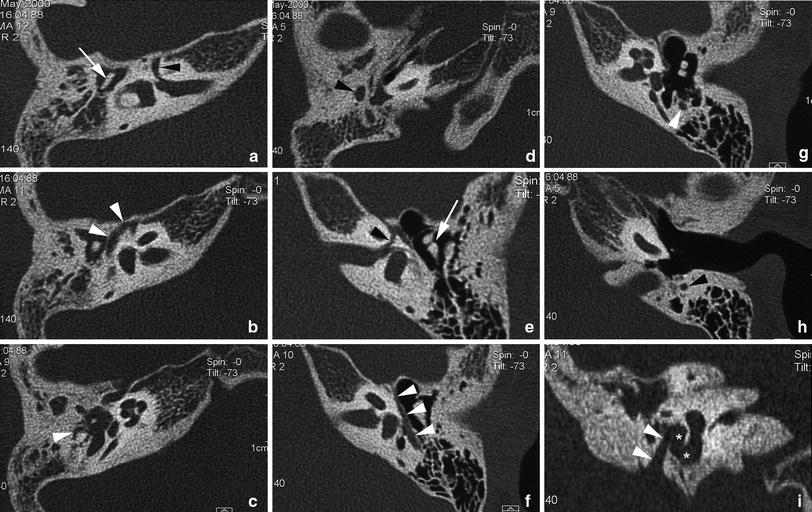
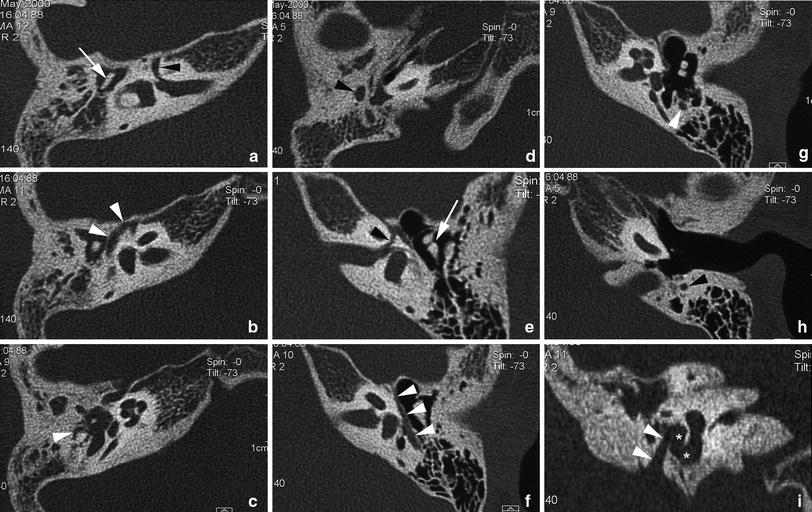
Fig. 4
Right-sided Goldenhar syndrome in a 12-year-old patient. a–d Axial CT images through right temporal bone. The facial nerve canal shows a relatively long labyrinthine segment (a, arrowhead); note the associated hypoplastic appearance of the ossicular chain (a, arrow). Short tympanic segment of facial nerve (b, arrowheads); a second genu cannot be clearly identified, but the mastoid segment of the facial canal is running posterolaterally to the tympanic cavity (c, arrowhead). At a lower level, the mastoid segment of the facial nerve can be seen to run lateral to the middle ear cavity (d, arrowhead). e–h For comparison, the corresponding heterolateral structures are labelled on axial CT images of the normal left temporal bone at similar levels. i Coronal CT image through right temporal bone. The short mastoid segment of the facial nerve canal (arrowheads) can be seen to run inferolaterally, just lateral from the middle ear cavity (asterisks) (the opacification of the right middle ear cavity is presumably caused by chronic dysfunction of the Eustachian tube)
When the tympanic bone is aplastic, the position of the temporomandibular joint is frequently more posterior than normal, because of lack of a posterior bony support. Confluence of the temporomandibular joint soft tissue with the middle ear is regarded unfavourable for surgery, as maintaining support for the surgically created hearing apparatus is more difficult (Yeakley and Jahrsdoerfer 1996).
A 10-point scale has been devised based on the CT-findings, predicting the risk of complications and postoperative hearing results (Yeakley and Jahrsdoerfer 1996).
The CT study should also exclude the presence of a congenital or acquired cholesteatoma: atresia or stenosis of the external ear canal may hinder the normal migration of epithelium, leading to the accumulation of keratinized debris and hence formation of a cholesteatoma.
Although rare, abnormalities of the inner ear should be looked for. Usually, when associated with aural dysplasia, these inner ear malformations are minor; the labyrinthine function is not necessarily abnormal. The internal auditory canal may appear widened and more angled than normal.
2.2 Branchiogenic Anomalies
Although aural dysplasia can be regarded as a branchiogenic anomaly (see above), other anomalies arising from the branchiogenic apparatus may occur around the external ear.
Defects of the branchial apparatus manifest as a cyst, a sinus, or a fistula. Anomalies of the branchial complex are vestigial remnants, resulting from incomplete obliteration of the branchial apparatus or buried epithelial cell rests.
As indicated above, the first branchial apparatus is involved in the development of the external and middle ear, but also the Eustachian tube, maxilla, and mandible.
First branchial cleft anomalies lie close to, or have a connection with the external ear canal. Various classifications have been proposed, such as that described by Work (Work 1972). A Work type I anomaly corresponds to a lesion in the preauricular region, running more or less parallel to the external ear canal, embedded within the parotid gland, and lateral to the facial nerve (Fig. 5).
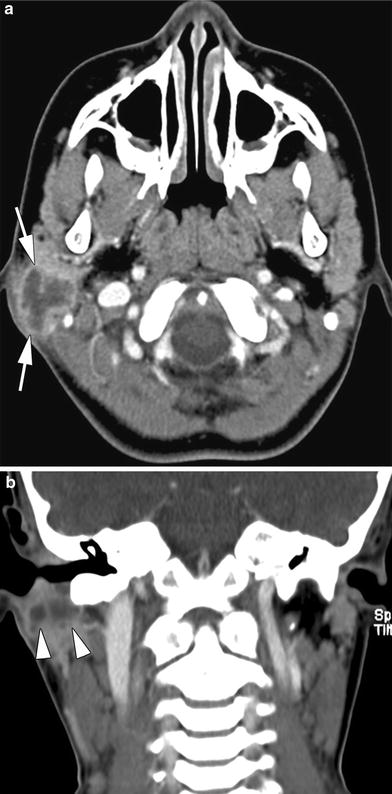
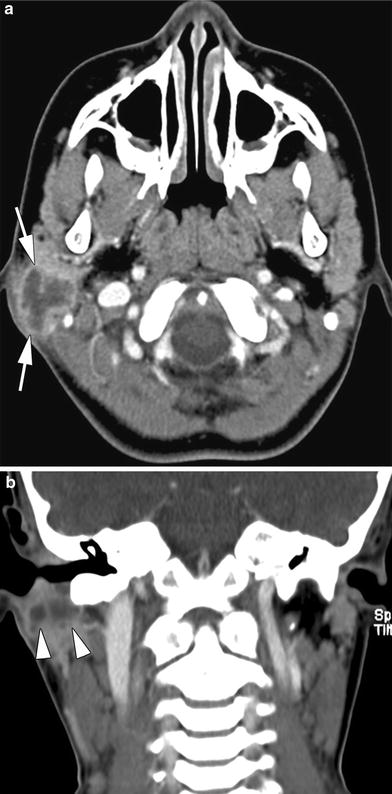
Fig. 5
7-year-old child presenting with a painful infra-auricular swelling. Axial (a) and coronal CT-image (b) show a cystic lesion with a thick enhancing wall, embedded in the parotid gland (a, arrows) and running parallel to the external ear canal (b, arrowheads). Infected first branchial cleft cyst (type I)
A Work type II anomaly extends downward to the angle of the mandible; it may be lying medial or lateral to the facial nerve branches, or between these nerve branches (Fig. 6). At the level of the mandibular angle an inflammatory mass lesion may be produced (Fig. 7). Demonstration of a connection to the external ear canal, typically at the junction of the cartilaginous and bony part, allows confirming the diagnosis.
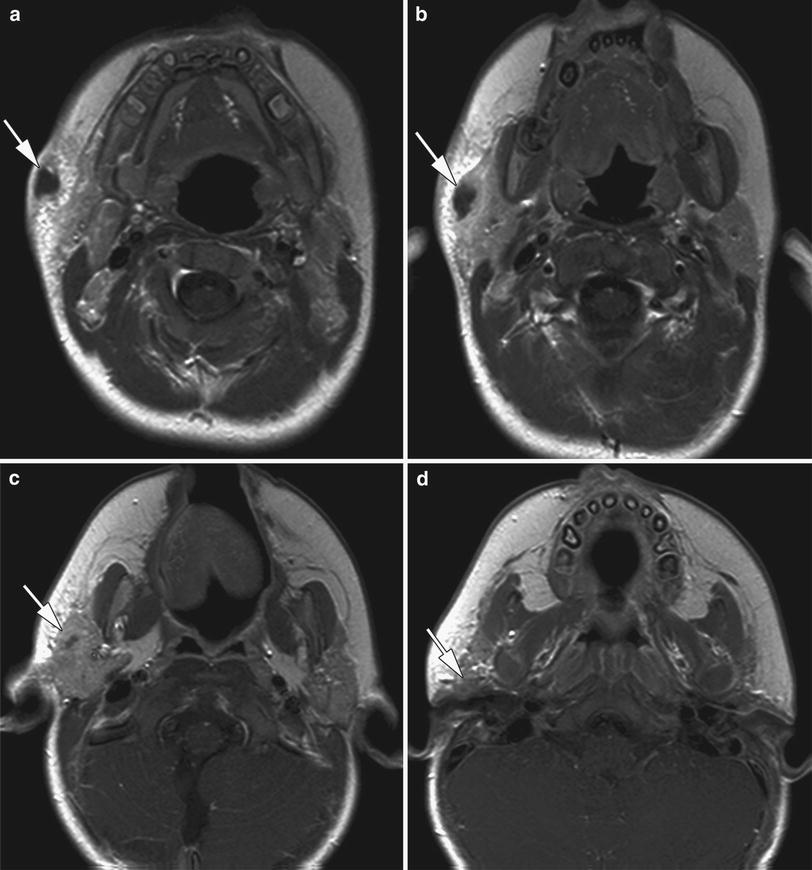

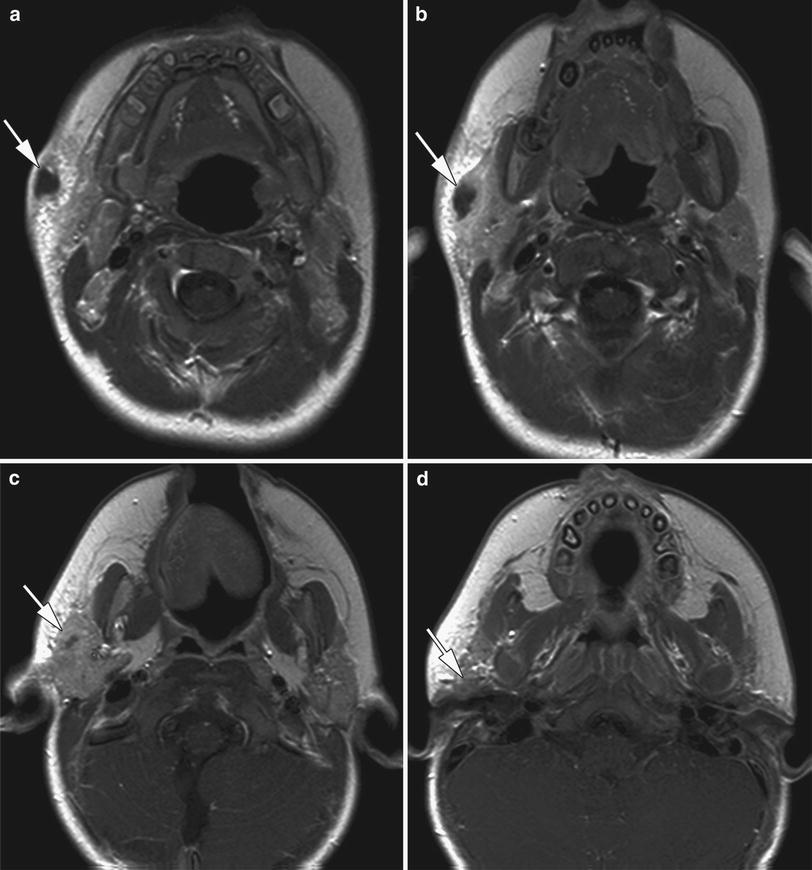
Fig. 6
18-month-old child initially presenting with a right-sided preauricular abscess and a sinus opening at the level of the right mandibular angle. This opening was present since birth. Axial contrast-enhanced T1-weighted spin echo images (a–d) show a tubular enhancing structure (arrows), partially fluid-filled, extending from the skin at the level of the mandibular angle (a), through the superficial lobe of the parotid gland (b, c), eventually reaching the external ear canal (d). This sinus was excised, including its connection with the external ear canal. First branchial cleft anomaly (type II)

Fig. 7
Axial contrast-enhanced CT images. Right sided tubular anomaly communicating with the malformed tympanic bone (a, arrow), extending inferiorly just deep to the parotid gland (b, arrow), ending in an inflammatory mass in the submandibular space (c, arrows). First branchial cleft anomaly (type II)
2.3 Preaurical Sinus
The auricle develops from six mesenchymal proliferations surrounding the first pharyngeal cleft. These swellings fuse and gradually form the definitive auricle. As this fusion is a rather complicated process, developmental abnormalities may arise (Langman 1981). A sinus results when one of the sulci between the auricular hillocks incompletely disappears. Most authors believe that a preauricular sinus is not an anomaly of the first branchial apparatus.
A preauricular sinus is a relatively common congenital abnormality. It consists of a blind-ending opening in the external ear, often located at or near the anterior crus of the helix. The diagnosis is made clinically. Most of these sinuses remain asymptomatic, but repeat infection may cause chronic discharge, repeated abscess formation and scarring, making surgical excision of the sinus and its possible ramifications necessary. Recurrences may follow incomplete resection (Currie et al. 1996).
Preoperative visualisation of the extent of the lesion may be helpful to prevent incomplete resection. Usually, injection of the sinus tract with contrast medium is not successful, as the lumen is often blocked by epithelial debris (Lau 1983). Forced injection of methylene blue, followed by surgery a few days later has also been suggested. A noninvasive method is high-resolution ultrasound, allowing to visualise the sinus, its branches, and any associated cystic component in the subcutaneous tissues; also the relationship of the lesion to the auricular cartilage and parotid gland can be demonstrated (Ahuja et al. 2000).
3 Inflammatory Conditions
3.1 External Otitis
In most cases of external otitis, imaging studies are not required as the disease can be well inspected and followed up by clinical examination.
External otitis, also known as swimmer’s ear, is a common condition; maceration by water or trauma is often the etiologic factors. Also dermatologic and endocrinologic conditions may give rise to external otitis. External otitis presents with itching, sometimes severe pain, and a cheesy discharge. The ear canal is diffusely swollen and tender. Most cases are controlled with topical treatment. In severe cases, cellulitis of the surrounding structures may be present, requiring systemic antibiotic treatment.
External ear furuncles are also common; they appear as localized, tender, and possibly fluctuant swellings. Treatment is by drainage of fluctuant areas and topical antibiotics; systemic antibiotics are needed when there is cellulitis or systemic symptoms.
Chronic external otitis may lead to acquired stenosis of the external auditory canal (Keohane et al. 1993), as recurrent inflammation with formation of granulation tissue may eventually lead to fibrosis and obliteration of the canal. Treatment is either by surgical correction or by a hearing aid.
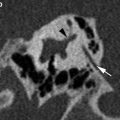
Ramsay–Hunt syndrome (also known as herpes zoster oticus) corresponds to acute facial neuritis, causing facial paralysis, otalgia, and vesicles in the external ear. It is thought to be a cranial polyneuropathy caused by the herpes zoster virus (De and Pfleiderer 1999). Sometimes also hearing loss, tinnitus, or vertigo may be present. MRI shows enhancement of the facial nerve, similar as in Bell’s palsy; enhancement of the intracanalicular portion of the vestibulocochlear nerve and the labyrinth may sometimes be seen.
Relapsing polychondritis is a rare inflammatory disease of cartilage of unknown origin, producing a bizarre form of arthritis. It may involve the cartilages of the ear, nose, and respiratory tract. Involvement of the auricle and cartilaginous portion of the external auditory canal is clinically apparent. Imaging is not required for evaluation of the external ear. Also the inner ear may be involved in this condition; enhancement of the labyrinthine structures on MRI has been reported (Vourtsi et al. 1998).
3.2 Necrotizing External Otitis
Necrotizing external otitis is a severe infection of the external ear, almost exclusively caused by Pseudomonas aeruginosa. Because of the aggressive clinical course, it has also been called ‘malignant external otitis’ (Chandler 1968). However, the disease is not neoplastic, and also does not remain limited to the external ear. Generally, ‘necrotizing external otitis’ is considered the most accurate descriptive name of this disease process.
Most patients are suffering from diabetes, or otherwise immunocompromised; the disease also occurs in elderly patients. It usually occurs unilateral, but bilateral cases have been described. Severe otalgia is the most common symptom; the patients may also suffer from purulent otorrhea. Clinical examination shows inflammatory changes and the presence of granulation tissue at the junction of the bony and cartilaginous part of the external auditory canal.
The exact pathogenesis is unknown. Pseudomonas is not a commensal of the external auditory canal, but may colonise this structure; colonisation may occur after nondiscriminant use of broad spectrum antibiotics for ear infection or after irrigation of the ears with nonsterile tap water containing Pseudomonas (Rubin and Yu 1988). Ischaemic conditions, related to diabetic microangiopathy or the effect of ageing, result in hypoperfusion and may increase susceptibility to infection. Also decreased activity of white blood cells may be a contributing factor.
The infection rapidly spreads to involve surrounding bone and soft tissues. The disease may erode into the bone of the mastoid. Anterior extension into the temporomandibular joint may occur, possibly causing destructive osteomyelitis (Midwinter et al. 1999); anterior spread may also involve the parotid gland.
Anteromedial extension into the infratemporal space may occur. Facial nerve palsy develops in 24–43 % of the cases, and is considered to be bad prognostic sign (Rubin and Yu 1988). The facial nerve usually becomes affected by infratemporal spread of the infection toward the stylomastoid foramen. As the infection spreads below the skull base, other cranial neuropathies can result. Intracranial extension may occur in advanced cases.
CT and MRI are excellent techniques to visualise the disease extent. MRI is the preferred modality if intracranial spread is suspected (Grandis et al. 1995).
CT shows thickening of the soft tissues in the external ear canal, possibly with erosion of the tympanic bone. Erosion and destruction of the temporomandibular joint may occur (Fig. 8). Typically, subtemporal extension begins at the junction of the osseous and cartilaginous part of the external auditory canal. Soft tissue infiltration and abnormal enhancement may be seen underneath the temporal bone, extending into the stylomastoid foramen; this infiltration may further progress into the parapharyngeal space (including the carotid space) and masticator space. Soft tissue infiltration and/or abnormal enhancement of the parotid gland may be observed. Hypodense regions with thick and/or irregular rim enhancement, corresponding to abcedation, may be present.
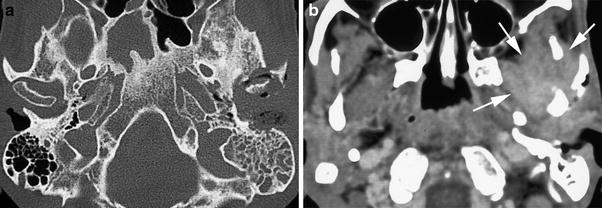
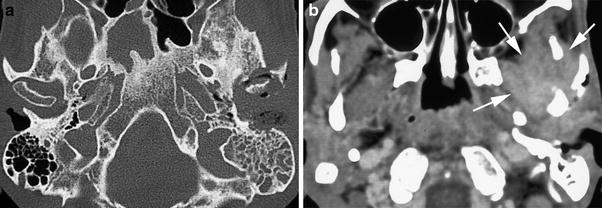
Fig. 8
Axial CT-images through skull base show destruction of the bony external auditory canal, erosion of the mastoid bone and invasion of the temporomandibular joint (a). The contrast-enhanced image reveals extension of the infection into the soft tissues of the infratemporal fossa (b, arrows). Necrotising external otitis
The disease may extend toward the clivus and apex of the petrous bone. A discontinuous pattern of bone destruction, with ‘skip’ areas, may be seen. In severe cases, not only cortical erosion, but also trabecular alterations in the medullary bone space may be observed; these medullary changes may appear osteosclerotic, osteolytic, or mixed.
The disease may extend posteriorly and erode into the mastoid, possibly causing destruction of the mastoid portion of the facial nerve canal.
The most common finding on MRI is infiltration of the fat behind the mandibular condyle (Kwon et al. 2006). Other common findings are parapharyngeal fat infiltration, skull base bone marrow infiltration, lateral nasopharyngeal wall thickening, and preclival soft tissue infiltration (Fig. 9).
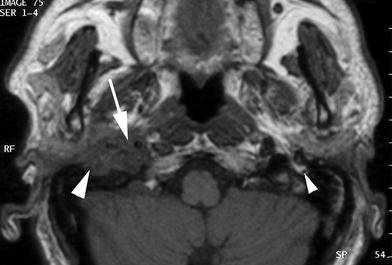
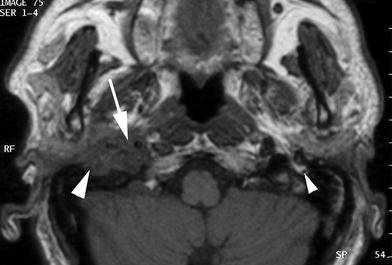
Fig. 9
Axial T1-weighted MR image. Diabetic patient suffering from right sided external otitis and facial palsy. In continuity with the external auditory canal, an infratemporal soft tissue infiltration is seen, extending in the fat pad below the stylomastoid foramen (large arrowhead), and into the carotid space (arrow). On the left, note normal facial nerve just below the stylomastoid foramen (small arrowhead). Necrotising external otitis
An abnormal flow void in the internal carotid artery, which may be displaced, and intracranial dural enhancement (in the middle or posterior cranial fossa, in severe cases extending into the foramen magnum) may be present.
Necrotizing external otitis occasionally causes central skull base osteomyelitis. Atypical cases of central skull base osteomyelitis, arising from the sphenoid or occipital bone, without obvious external otitis, are much less frequently seen (Chang et al. 2003). Inadequately treated necrotizing external otitis may also give rise to contralateral skull base osteomyelitis (Singh et al. 2005).
The radiographic differentiation from true malignant neoplasia may be difficult; rarely both conditions are present at the same time (Rubin et al. 1990). In cancer, the bone involvement is expected to display a more contiguous pattern of destruction, while in necrotizing otitis media ‘skip’ areas may be present. The clinical picture in external ear cancer is different, without or with only minimal pain. However, cancer may rarely mimic necrotizing otitis media in its clinical appearance (Mattuci et al., 1986; Al-Shihabi 1992).
The treatment consists of surgical debridement of the external auditory canal, drainage of collections, and intravenous antibiotics. Malignant otitis externa used to have a grave prognosis, but with the advent of more effective antibiotics, the infection can be controlled in the majority of cases. Cranial nerve involvement is often quoted as a bad prognostic sign. It does reflect more extensive disease, and the mortality rate is higher in these patients. However, recovery of facial nerve function after successful treatment has been observed.
4 Trauma
Trauma to the external canal is most commonly caused by instrumentation, either by the patient itself, or by a physician. Most of these smaller lacerations or canal haematomas can be handled with antibiotic drops, but more complex lacerations need temporary packing of the ear canal, in order to avoid fibrotic stenosis.
Fractures of the tympanic bone are quite frequent; they are usually caused by the impact of a posteriorly displaced mandibular condyle, itself resulting from a blow to the chin region. Care should be taken not to misinterpret the normal squamotympanic suture as a fracture line (Fig. 10).