Elbow/Forearm
Thomas H. Berquist
Laura W. Bancroft
Protocols
Key Facts
Routine radiography
Minimal series: anteroposterior (AP) and lateral views
Trauma series: AP, lateral, and both oblique views. (The optimal lateral view for hemarthrosis is a cross-table lateral.)
Computed tomography (CT)
3-mm axial sections (for conventional imaging)
Bone and soft tissue settings
1-mm sections at 0.5-mm intervals for coronal and sagittal reformatting or three-dimensional images
Magnetic resonance imaging (MRI) (Table 8-1)
Patient positioning arm at side
Coils
5-inch circular (allows more flexible positioning) Circumferential: elbow extended (more uniform signal intensity) Flat-phased array coil: if arm or forearm need to be included in field of view
Fractures/Dislocations: Distal Humeral Fractures
Key Facts
Eighty percent of distal humeral fractures occur in children.
Fifteen percent of physeal fractures in children involve the distal humerus.
The mechanism of injury is a fall on the outstretched hand.
Fractures may be flexion or extension injuries. Extension injuries are 10 times more common than flexion injuries.
Extension fracture: oblique fracture with posterior displacement of the distal fragment
Flexion fracture: older age group; transverse fracture line; distal fragment anterior
Fractures usually are obvious on AP and lateral radiographs. CT with coronal and sagittal reformatting if helpful for evaluating subtle injuries. MRI is useful for physeal fractures in young children.
Treatment: closed reduction
Complications: neurovascular injury, premature physeal closure, arthrosis, malunion, nonunion
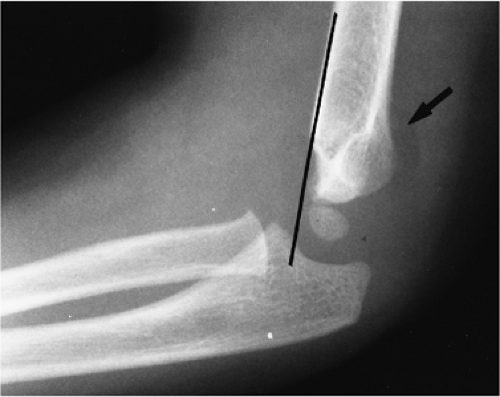
 FIGURE 8-1 Distal humeral fracture. Lateral (A) and AP (B) radiographs of an extension supracondylar fracture. The distal fragment is displaced posteriorly (arrow). |
Suggested Reading
Anderson SE, Otsuka NY, Steinbach LS. MR imaging of pediatric elbow trauma. Semin Musculoskel Radiol 1998;2:185–198.
Kinik H, Atalar H, Mergen E. Management of distal humeral fractures in adults. Arch Orthop Trauma Surg 1999;119:467–469.
Murphy BJ. MR imaging of the elbow. Radiology 1992;184:525–529.
Fractures/Dislocations: Epicondylar Fractures
Key Facts
Avulsion fractures of the epicondyle are common in children.
The injury is common in throwing athletes, specifically pitchers.
The medial epicondyle is particularly vulnerable between ages 9 and 14 years.
Mechanism of injury is varus and valgus forces. Medial epicondylar fractures are common; lateral epicondylar fractures are rare.
Displaced medial epicondylar fragments may be trapped in the joint.
Routine radiographs usually are adequate for diagnosis. MRI is useful for subtle undisplaced fractures and associated soft tissue injuries.
Treatment: closed reduction for undisplaced fractures; pinning of displaced (>3 mm) fractures.
Complications: fragment entrapped in joint, instability.
Suggested Reading
Larson RL. Epiphyseal fractures in the adolescent athlete. Orthop Clin North Am 1973;4:839–851.
Fractures/Dislocations: Adult Distal Humeral Fractures
Key Facts
The distal humerus consists of medial and lateral columns with the trochlea between the two columns.
The mechanism of injury is trochlear impaction into the humeral articular surface with flexor and extensor muscles causing displacement of the epicondyles.
Fractures may be nonarticular, involve one condyle or have a “T” or “Y” configuration with varying degrees of comminution.
Treatment: internal fixation commonly required
Routine radiographs usually are diagnostic. CT with coronal and sagittal reformatting is important for operative planning.
Complications: poor reduction, exuberant callus, reduced range of motion, arthrosis, nonunion (2%–10%), nerve compression (15%), and postoperative infection.
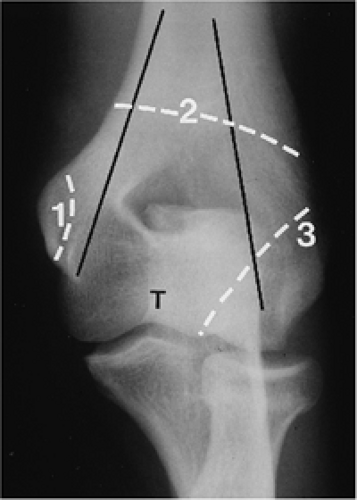
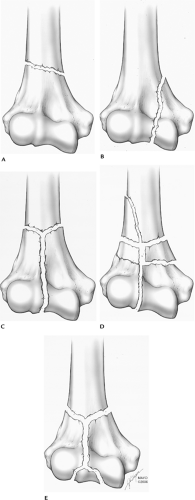 FIGURE 8-5 Adult distal humeral fracture patterns. (A) Extra-articular. (B) One condyle. (C) Both condyles. (D,E) Both condyles with comminution. |
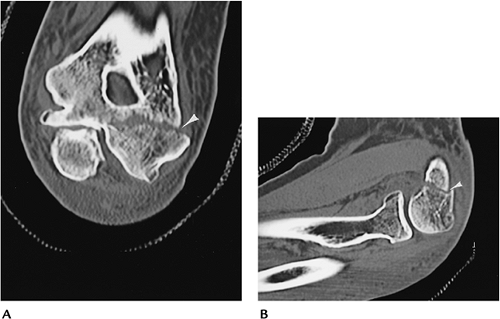 FIGURE 8-7 CT images of a lateral column fracture reformatted in the coronal (A) and (B) sagittal planes. |
Suggested Reading
Helfet DL, Kloen P, Anand N, et al. Open reduction and internal fixation of delayed unions and nonunions of fractures of the distal part of the humerus. J Bone Joint Surg 2003;85A:33–44.
Ring D, Jupiter JB. Complex fractures of the distal humerus and their complications. J Shoulder Elbow Surg 1999;8:85–97.
Fractures/Dislocations: Capitellar Fractures
Key Facts
Capitellar fractures account for 1% of elbow injuries.
Fractures may involve the entire capitellum or the articular surface, or be comminuted and involve the radial head.
Mechanism of injury: direct blow or fall on the outstretched hand with force transmitted from the radius to the capitellum.
Subtle fractures may present with a positive fat pad sign and may require CT or MRI for detection.
Treatment: Loose fragments may require removal. K-wire fixation of large fragments may be necessary in certain cases.
 FIGURE 8-8 Lateral view of the elbow demonstrating a capitellar fracture (arrow) and displaced fat pad (open arrow). |
Suggested Reading
Fowles JV, Dassab MT. Fractures of the capitellum humeria. J Bone Joint Surg 1975;56A:794–798.
Fractures/Dislocations: Fractures of the Proximal Radius
Key Facts
Fractures of the radial head and neck are common, accounting for one third of elbow fractures. Fractures are categorized as three types based on displacement or comminution of the radial head or neck. Type I, undisplaced (<2 mm) head or neck fracture; Type II, displaced head or neck fracture; Type III, comminuted head or neck fracture.
Mechanism of injury: Fall on the outstretched hand with the elbow partially flexed and pronated.
Associated elbow, forearm, and wrist injuries may be present.
Routine radiographs may be normal, except for a positive fat pad sign. Follow-up in 10 to 14 days may demonstrate the fracture. MRI or CT may be required for detection of subtle fractures and for operative planning with complex fractures.
Treatment: Undisplaced fractures are treated with closed reduction. Displaced or comminuted fractures may require internal fixation, resection, or arthroplasty.
Complications include associated ulnar fracture, heterotopic ossification, instability, and arthrosis.
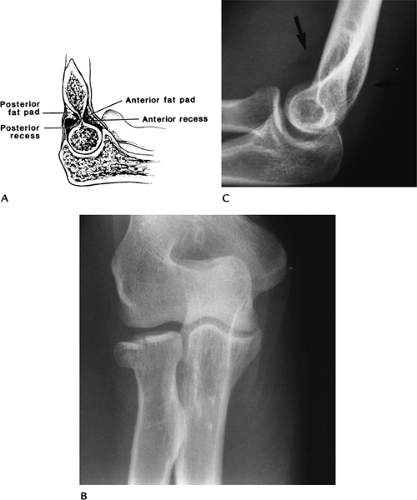 FIGURE 8-9 Fat pad sign. (A) Normal position of the fat pads. AP (B) and lateral (C) radiographs of a radial head fracture with displaced fat pads on the lateral view (arrows). |
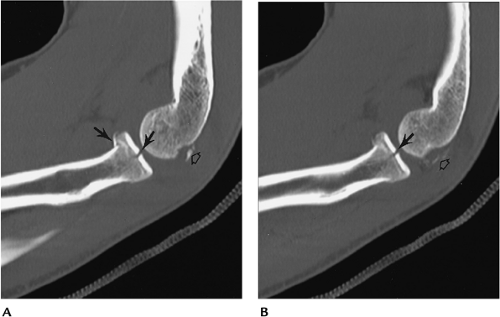 FIGURE 8-10 CT images in the sagittal plane (A,B) demonstrate a minimally displaced comminuted radial head fracture (arrows) with associated capitellar fragments (open arrow). |
Suggested Reading
Corbett RH. Displaced fat pads in elbow trauma. Injury 1978;9:297–298.
Geel CW, Palmer AK. Radial head fractures and their effect on the radioulnar joint: A rationale for treatment. Clin Orthop 1992;275:79–84.
Fractures/Dislocations: Ulnar Fractures
Key Facts
The ulnar is susceptible to trauma because of its superficial location.
Mechanism of injury: direct blow after fall on the flexed elbow.
Most fractures are intra-articular.
Triceps fascia disruption leads to significant displacement and articular deformity.
Routine radiographs usually are diagnostic. The lateral view is most useful.
Treatment: Joint congruity must be restored, which usually requires internal fixation for displaced fractures.
Complications: instability, decreased range of motion (3%–50%), articular deformity and arthrosis, ulnar neuropathy (10%), and nonunion (5%).
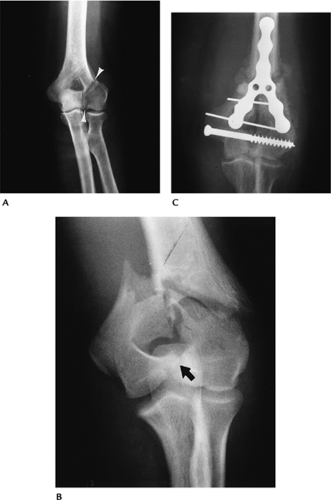
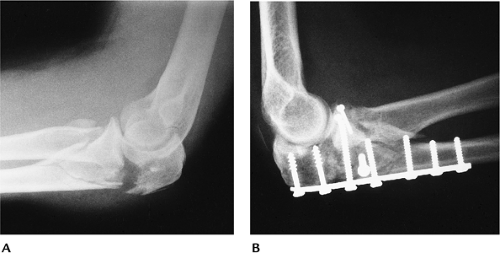 FIGURE 8-11 (A) Lateral view of the elbow showing a displaced olecranon and radial head fractures. (B) Fractures were internally fixed using plate and screw fixation. |
Suggested Reading
Rettig AC, Waugh TR, Evanski PM. Fracture of the olecranon. A problem of management. J Trauma 1979;19:23–28.
Fractures/Dislocations: Coronoid Fractures
Key Facts
Isolated coronoid fractures are uncommon. There are three categories of fracture. Type I: small avulsion of the coronoid tip. Type II: fracture involves 50% of the coronoid, but does not extend to the base. Type III: fracture of the coronoid base.
Coronoid fractures are seen most commonly with posterior dislocations.
Recurrent dislocation is common after coronoid fracture/dislocation.
Displaced fractures can be detected on radiographs. The lateral view is most useful. CT may be required for detection of undisplaced fractures.
Treatment: Closed reduction is adequate in most cases.
Complications: instability, arthrosis, recurrent dislocation.
Suggested Reading
Regan W, Morrey BF. Fractures of the coronoid process of the ulna. J Bone Joint Surg 1989;71A:1348–1354.
Fracture/Dislocations: Elbow Dislocations
Key Facts
Dislocation classifications refer to the position of the dislocation.
Most elbow dislocations are posterior and involve both the radius and ulna.
The mechanism of injury is a fall with the elbow extended.
Anterior, medial, and lateral dislocations are uncommon.
Associated injuries include coronoid, radial head, epicondylar fractures, and neurovascular injuries.
Postreduction CT imaging is important to fully assess the joint space and associated fractures.
Complications include arthrosis, instability, decreased range of motion, neurovascular injury, and extensive heterotopic ossification.
 FIGURE 8-13 AP (A) and lateral (B) radiographs of a posterolateral dislocation with associated fracture of the radial head (arrow) and neck. |
Suggested Reading
Koyle SG. Posterior dislocations of the elbow. Clin Orthop 1991;269:201.
O’Driscoll SW, Morrey BF, Korinek S, et al. Elbow subluxations and dislocations: A spectrum of instability. Clin Orthop 1992;280:186–197.
Pugh DMW, Wild LM, Schemitsch EH, et al. Standard surgical protocols for treatment of elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg 2004;86A:1122–1130.
Fractures/Dislocations: Monteggia Fractures
Key Facts
Monteggia fracture or lesion is a dislocation of the radial head with an associated proximal ulnar fracture.
This injury accounts for only 7% of ulnar fractures and 0.7% of elbow injuries.
Four injury patterns are commonly described:
Type I
Fracture of the ulna with anterior dislocation of the radial head (50%–75% of cases)
Type II
Fracture of the ulna with posterior or posterolateral radial head dislocation (10%–15% of cases)
Type III
Fracture of the ulna with lateral or anterolateral radial head dislocation (6%–20%; more common in children)
Type IV
Anterior dislocation with radial and ulnar fractures (5% of cases)
Mechanism of injury: direct blow to posterior ulna, fall on the outstretched hand with elbow flexed, or hyperextension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree